Triamacinolone Acetonide Versus Bevacizumab in Treatment of Neovascular Age Related Macular Degeneration
Mona Abd El Kader*
Department of Ophthalmology, Mansoura University, Egypt
Submission: March 9, 2017; Published: July 20, 2017
*Corresponding author: Mona Abd El-Kader, Department of Ophthalmology, Mansoura University, Egypt, Email: monnabdelkader78@yahoo.com
How to cite this article: Mona A E K. Triamacinolone Acetonide Versus Bevacizumab in Treatment of Neovascular Age Related Macular Degeneration. JOJ Ophthal. 2017; 3(4): 555625. DOI:10.19080/JOJO.2017.03.555625
Abstract
Purpose: To evaluate the effects of intravitreal triamacinolone acetonide (IVTA) and bevacizumab injection on visual acuity, electro physiologic response and foveal thickness of patients with neo vascular age related macular degeneration (CNVs).
Methods: The study included three groups. Group 1 included fifty eyes (50 patients) with progressive occult or predominately occult sub foveal choroidal neovascularization treated with intravitreal injection of trimacinolone acetonide. Group 2 included another fifty eyes (50 patients) with progressive macular degeneration of occult or predominately occult sub foveal choroidal neovascularization treated with intravitreal bevacizumab. The patients is followed up every month by bio microscopy, optical coherence tomography (OCT), photography, fluoresce in angiography, Ganzfeld full field electro retinogram(F-ERG), multifocal electro retinogram (MF-ERG) and determination of best corrected visual acuity (BCVA). Group 3 (control group) included 50eyes (50 patients) with neo vascular age related macular degeneration who did not receive treatment for macular degeneration.
Results: Apparent improvement of morphological and functional characteristics were observed in 40/50 eyes after one month after first injection in group1, and in 45/50 in group 2. The mean±SD visual acuity improved significantly (p=0.003) from (0.12 ±0.19 to 0.35±0.25) in group1 and from 0.13±0.2 to 0.40±0.28 in group 2. Visual acuity was highest 1-2 month after intravitreal injection. Central macular thickness decreased from 325±50^m to 275±40^m at one month after first injection in group 1 and decreased from 320±53^m to 255±41^m in group 2 while in control group, there is statistically insignificant increase of the central thickness. The average amplitude of central macular ring of MFERG was improved from 25.5±5.8nv to 31±8.9nv in group 1 and from 26.6±6.1nv to 33±9.9nv in group 2, while no changes in F-ERG response. Intraocular pressure increased significantly (p=0.009) from 14±2.5mmHg to maximal 23±7.6mmHg in group 1. Intraocular pressure decreased significantly (p=0.006) to 16±2mmHg at the end of follow up while in group 2, there was no increase in intraocular pressure. No other serious drug related adverse events (endophthalmitis, retinal detachment, cataract or proliferative vitreo retinopathy) observed during the course of the study in groups 1, 2. In control group, visual acuity, central foveal thickness and function did not change significantly during follow up period (p=0.6, p=0.4, p=0.1 respectively).
Conclusion: Intravitreal injection of trimacinolone acetonide may transiently stabilize or improve visual acuity in some patients with progressive neo vascular age related macular degeneration. Intravitreal injection of bevacizumab led to a more visual improvement than IVTA in treatment CNVs. MFERG had an important role in describing the effect of treatment on retinal function. Intravitreal injection improved MFERG macular function responses with little insignificant change in F-ERG.
Keywords: Electroretinogram; Optical coherence tomography; Choroid neovascularization; Avastin; Triamacinolone acetate
Introduction
None of the present treatment decreases the loss of vision on the central 35° of the retina in macular degeneration. Neovascular age related macular degeneration is a common reason for irreversible reduction and loss of vision in the world [1] . Triamacinolone acetonide is one of the first drugs used for the management of age related choroidal neo vascularization [2] . Triamacinolone acetonide stabilizes blood retinal barrier, decreases the permeability and inflammation, increases the diffusion and reduces vascular endothelial growth factor [3]. Vascular endothelial growth factor (VEGF) plays important role in AMD pathogenesis [4]. Bevacizumab is humanized antibody to human vascular endothelium growth factor (VEGF) which combines to VEGF and hinders it from attachment to its receptors [5]. Electro retinogram of neo vascular macular degeneration gives information about the treatment safety. MF-ERG represents the photopic retinal response to a rapidly changing stimulus on the central 35° of the retina [6]. Neovascular age related macular degeneration decreases the central peak amplitude which is altered by subretinal fluid [7]. MF-ERG is used to monitor the localized change after treatment. Full field ERG response reflects general retinal electrical response and gives information about treatment toxicity [6,7]. The aim of the study was to evaluate and compare the effects of triamacinolone acetonide and bevacizumab on visual acuity and retinal thickness in neovascular age related macular degeneration patients and to study the effects of triamacinolone acetonide and bevacizumab on the retinal function.
Subjects and Methods
This study was carried out on patients attending the Outpatient's Clinic of Mansoura Ophthalmic Center during the period from February 2012 to December 2015. One hundred and fifty patients (150) with neovascular age related macular degeneration were included in the study.
The patients were divided into three group:
a) Group 1: Included progressive occult subfoveal choroidal neovascularization patients who received intravitreal injection of triamcinolone acetonide.
b) Group 2: Included occult subfoveal choroidal neovascularization patients who received intravitreal injection of bevacizumab.
c) Group 3 (control group): Included neovascular age related macular degeneration patients who refused intravitreal injection.
Exclusion criteria
Included patients with classic type of neovascular age related macular degeneration and any other ophthalmological. All patients were examined on the first day after injection, in first week, then every month for 6 months. A repeated injection was performed if there were activity of choroidal neovascularization (CNV). Intra-retinal and sub-retinal fluid accumulation, new intra-retinal and sub-retinal hemorrhage and CNVs growth were signs of CNVs activity. Re-treatment was done if there were signs of CNV activity or decreasing visual acuity. At baseline of the study and at monthly intervals, all patients underwent a routine ophthalmological examination. Goldman applanation tonometry, direct and indirect ophthalmology, optical coherence tomography (OCT), and electroretinogram (ERG) were done. Fluorescein angiography was done using Topcon Corporation 2000, TRC, 50Ix, Japan. Fluorescein angiography was performed for all patients at beginning and after 3months and 6 months.
Optical coherence tomography (OCT)
OCT was done with Topcon, 3 dimensional OCT-1000 (Topcon Corporation, Tokyo, Japan). Internal fixation was chosen because of better reproducibility. It scanned a cube of 6x6mm length. Central macular thickness of a circular 1-mm radius area around the fovea was calculated.
ERG
Full field ERG and MF-ERG were recorded using Roland Consult, (Germany system). ERG was done according to ISCEV standard [8]. After topical corneal anesthesia (Benoxinate hydrochloride 4%), positive electrode (Dawson, Trick and litzkow (DTL) electrode) was placed just contact with corneal limbus, ground electrode was installed on the forehead and negative electrode was placed near orbital rim temporary. The recording was monocular.
Full field ERG
The test was started and recorded in 5 steps, scotopic rod response, scotopic combined response, oscillatory potential then light adaptation for 10 minute then photopic cone response and flicker response recording.
MF-ERG
Patients were positioned 30cm from the stimulus monitor. Stimulus clarity was adjusted by over-refraction. Each hexagon was temporally modulated between light and dark according to binary m-squence [9,10]. Patients fixated a spot in the center of the stimulus. The results of two 8-minute recordings were averaged to improve the signal to noise ratio.
Intravitreal injection of triamacinolone acetonide (IVTA)
In group 1, 25mg of crystalline triamacinolone acetonide (Volona A, Bristol-Myers-Squibb, Munich, Germany, containing 40mg of triamacinolone acetonide in 1ml) was injected intravitreal. The injection of 25mg of crystalline triamacinolone acetonide was performed using sharp 27-gauge needle in inferio-temporal quadrant 3.5mm from limbus.Then antibiotic ointment was applied.
Intravitreal injection of bevacizumab
All patients in group 2 received Intravitreal injection of 1.25mg/0.05 of bevacizumab. A total of 0.05ml Bevacizumab was injected into vitrous cavity 3.5mm from limbus in inferotemporal quadrant using 30 gauge needles. Postoperative antibiotics were used and a light patch was placed. The eye patch is removed the next day.
Statistical Analysis
Statistical analysis was performed using soft ware (SPSS WIN Version11.5, SPSS Inc, Chicago). Non parametric Wilcoxon test was applied for comparison. Spearman rank test and linear correlation analysis were used in order to evaluate the correlation with changes of MFERG, changes of OCT and best correct visual acuity. Significance was set at p=0.05 (2-tailed) for all statistical tests.
Results
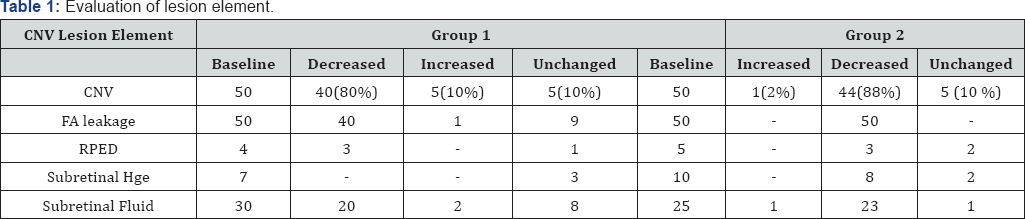
The study included one hundred and fifty (150) patients (one hundred and fifty eyes). The patients were divided into three groups. Group 1 included fifty eyes (50) of fifty patients (50) with progressive occult or predominately occult subfoveal choroidal neovascularization who received one or more than one of intravitreal injection of 25mg of triamcinolone acetonide, Mean age was 60±8.6years ,ranged (55 -75 years old). Group 2 included another fifty eyes (50) of fifty patients with progressive occult or predominately occult sub foveal choroidal neovascularization) who received one or more than one of intravitreal injection of 1.25mg/0.05ml of bevacizumab. The Mean age was 62±6.9 years, ranged (58-74 years). Group 3 (Control group) included fifty eyes (50) of fifty patients (50) (with neovascular age related macular but did not receive intravitreal injection of tri amcinolone acetonide for this disease after explanation the importance of treatment for visual acuity and CNVs. The Mean age was 61 ±7.9 years, ranged (58-74 years). There was no significant difference between groups. In group 1, Ten (10) patients received a second intravitreal injection of 25mg of triamcinolone acetonide. According to flourescein angiography, group 1 were further divided into subgroups with occult or mostly (>50%) occult without hemorrhage (n=40, 80%), subgroup with sub-retinal hemorrhage (n=7, 14%) and subgroups with retinal pigment detachment (n=4, 8%). While in group 2, occult CNV without haemorrhage was presented in 35 eyes (70%), with haemorrhage was present in 10 eyes (20%) and retinal pigment detachment was found in 5 eyes (10%) ( Table1). All three subgroups did not vary significantly (p=0.2) at baseline. In control group, all subjects were having occult CNV without sub retinal hemorrhage.
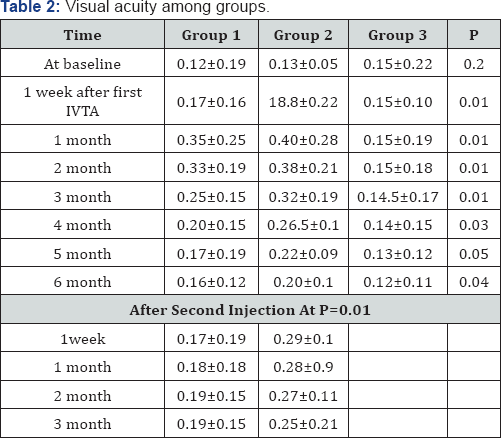
Visual acuity(VA)
All patients complained of decreased visions which were diagnosed by ophthalmologic examination within three months before IVTA. The mean VA at baseline in group 1, group 2 and control Group (0.12±0.19, 0.13±0.05 and 0.14±0.22) respectively. (Range from finger counting to 0.3 in group 1, from finger count to 0. 32 in group 2 and from finger counting to 0.5 in control group. For the Group 1 and Group 2, mean VA increased significantly (p=0.003) after first injection to maximum 0.35±0.25 during the follow up period (Table 2). The maximum postoperative VA was detected 1-2 months after the injection. The increase in VA was statistically significant in 1st month (p=0.003) and 2nd month (p=0.004) after the injection. The preoperative visual acuity and postoperative visual acuity achieved at the end of the follow up period did not differ significantly (p=0.2) in group 1 while in group 2, there is statistically significant difference between VA at the baseline and VA at the end. In group 1, Visual acuity significantly decreased towards the end of the follow up period, parallel to a disappearance of triamacinolone acetate crystals out of vitreous cavity. In group 1, after 1 month, 40eyes (80%) gained in visual acuity and 4eyes (8%) lost visual acuity. Visual acuity was unchanged for 6 eyes (12%). While, in group 2, 45 eyes (90%) gained in visual acuity. There were no significant correlation between postoperative visual acuity and postoperative change in visual acuity (p=0.6). For three subgroups, there were significant difference in gain in visual acuity (p=0.04). Ten eyes received second injection three months after first injection, visual acuity increased in eight eyes about one month after the re-injection and declined again after about 3 month in group 1 while in group 2, fifteen eyes received second injection after 2 months, and fourteen eyes of fifteen improved after reinjection.
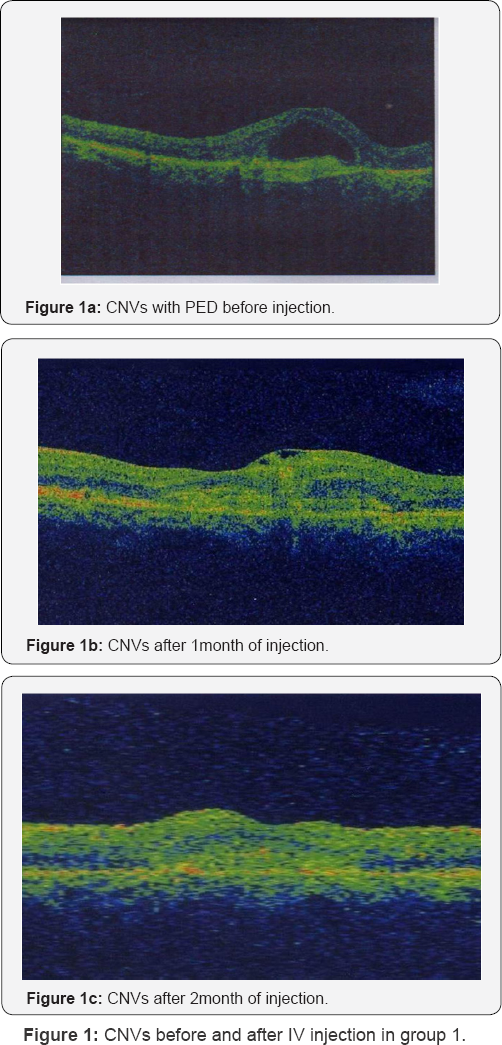
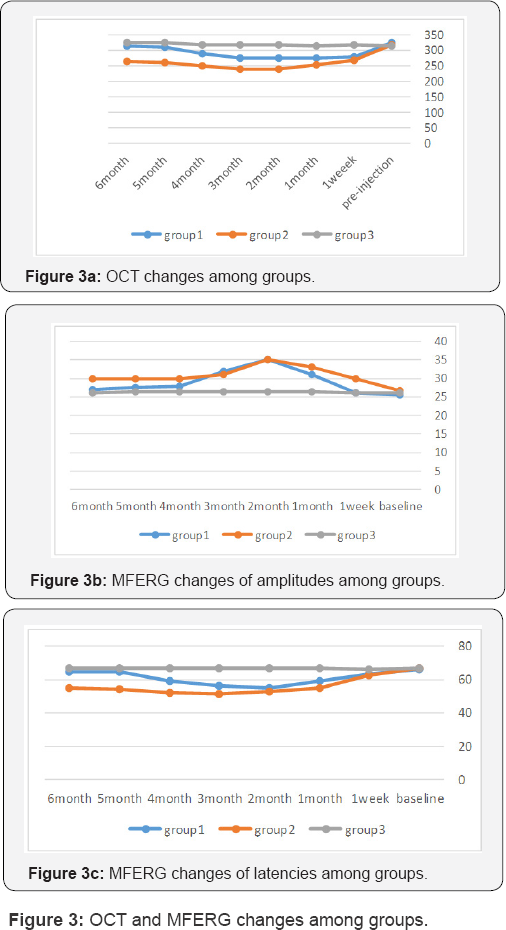
OCT
For group 1, Central subfield OCT thickness was 325±50μm at baseline. The central subfield OCT thickness decreased to 280±55μm at one week and 275± 40μm at one month (Table 3, Figure 1). In group 2, central subfield OCT thickness was 320±53μm at baseline. The Central subfield OCT thickness decreased to 270± 40μm at one week and 255±41μm at one month

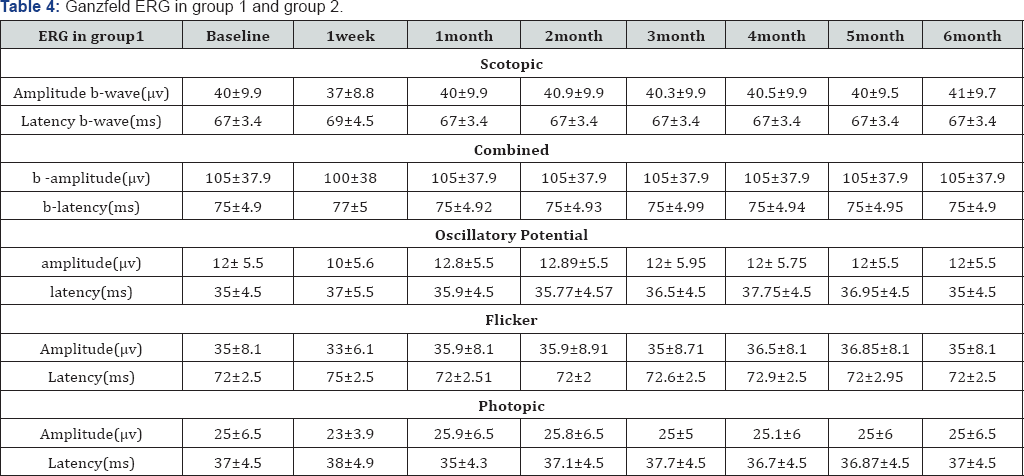
ERG
F-ERG data is presented in (Table 4). No significant worsening of FERG response was observed during follow up period in the three groups. Most of the values were within the limits normal variation. For most subjects retested one month with F-ERG, the amplitude returned to baseline after a slight decrease in scotopic and photopic amplitudes at one week. For all subjects who was received either triamacinolone acetate or bevacizumab had an essentially stable F-ERG.
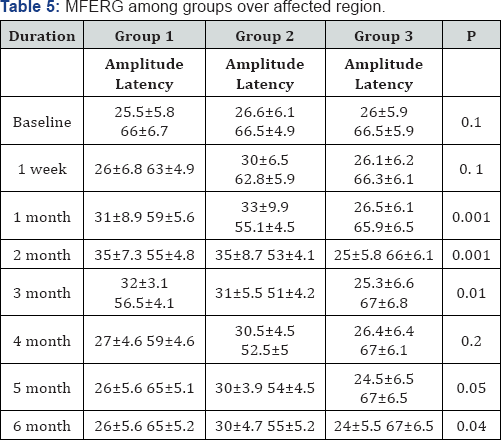
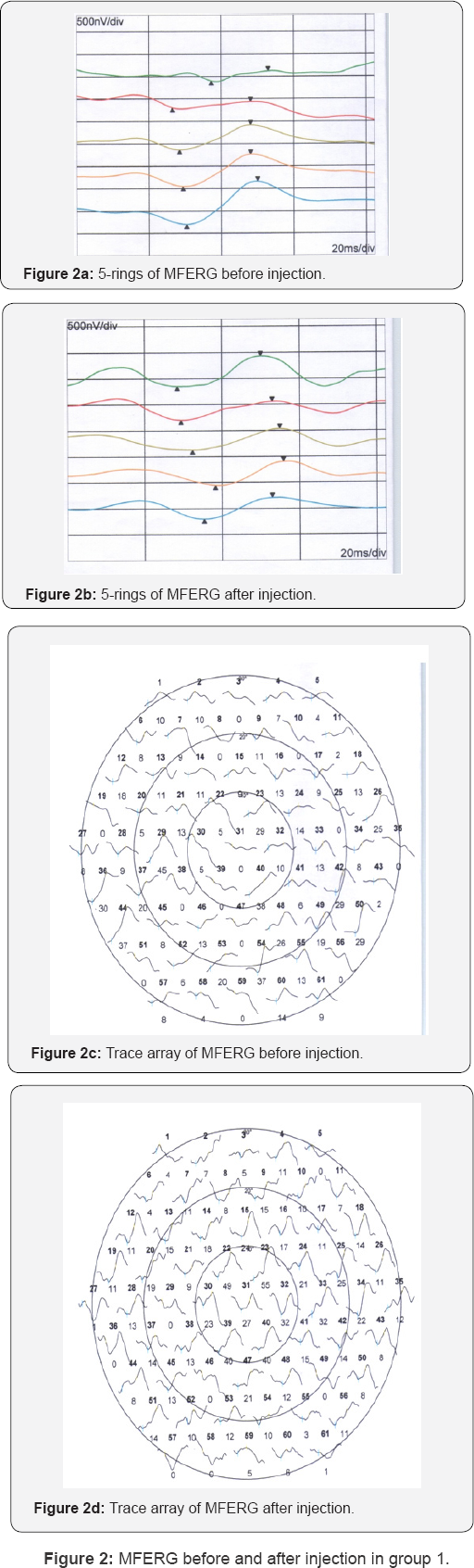
MFERG
In most cases, there was improvement at one week, one month and two months of IVTA, then return to baseline value at 3 months (Table 5, Figure 2 & 3). In group 2, there was increase in amplitude and decrease in latency reach the maximum after 2 months.
Intraocular complications
In group 1, IOP increased significantly (p=0.005) from 14.5±2.5mmHg at baseline of the study to a mean maximal value of 20±5.6mmHg again decreased significantly to 16.5mm Hg at 6 months after IVTA at p=0.001. IOP measurements at the end were slightly and significantly (P=0.05) higher. During the study, IOP was higher than 22mmHg in 30 eyes (60%). In those patients, IOP normalized by topical anti-glaucomatous drugs. Optic nerve damage was not detected. While in group 2, there was no case with increase in intraocular pressure. With respect to other complication of IVTA, three cases of cataract were detected in group 1, while no case of cataract was observed in group 2. No postoperative infectious endophthalimitis, rhegmatogenous retinal detachment or proliferative vitreo-retinopathy was detected in groups 1 and group 2.
Discussion
While, classic type of subfoveal neovascularization, photodynamic therapy with verteporfin stabilizes or increases visual acuity. Photodynamic therapy for occult subfoveal neovascularization is unsuccessful [11,12]. Steroids have antiinflammatory, antiangiogenic, antifibrotic and antipermeability properties, which contribute to stabilization of the blood- retina barrier [13] Penfold et al. [14,15] Chella et al. [16], injected trimacinolone intraviteal to treat exudative macular degeneration. Additionally, Danis et al. [17], detected a beneficial effect of trimacinolone in the study group compared with control group. Also, Ranson et al. [18], treated recurrent subfoveal neovascularization after laser treatment by IVTA. Chella et al. [16] evaluated the efficacy of intravitreal of trimacinolone for one and half year in exudative age related macular degeneration. They reported that a single intravitreal injection of 4mg of trimacinoloneacetate was helpful in treatment of exudative age related macular degeneration. In this study (in group 1), there was increase in visual acuity, reduction of fluorescein angiography leakage, reduction central macular thickness and increase in amplitude of MFERG with reduction of implicit time in 40 eyes of 50eyes (80%) within 2 months. Ten eyes of 40 eyes (25%) receive another intravitreal injection after 3 months (after beginning of reduction of visual acuity with increase macular thickness, reduction of amplitude of MFERG and increase implicit time). There was improvement of six of ten eyes (60%).
There was correlation between visual acuity and central macular thickness (p=0.008, R=0.5) and visual acuity and MFERG amplitude (P=0.006, R=0.55). Also, there was significant correlation between central macular thickness and MFERG amplitude (P=0.001, R=0.65) in group 1. In this study, we injected high dose of triamcinolone acetate intravitreal in group 1, because the results of previous studies were not clear; Jonas et al found significant increase in visual acuity after intravitreal injection of 25mg of trimacinolone acetate [19,20]. while Gillies et al. [21], reported no effect of 4mg of intravitreal injection of trimacinolone acetate on the development of sever visual loss during one year follow up. The Causes for the difference between studies may be the amount of injected trimacinolone acetate Second cause for difference between studies may be related to the effect of development of cataract on vision. Other cause for discrepancy between this study and investigation of Gillies et al. [21] may be that their study included classic subfoveal neovascularization that had a worse prognosis than occult choroidal neovascularization.
There was significant elevation in intraocular pressure in group 1 compared with other groups. There was 30 eyes (60%) had increased intraocular pressure. All cases were controlled with medical anti-glaucomatous treatment. Various studies have reported increase of IOP ranging from11-30% of subjects following IVTA [17,19,22] None of patients had been shown infectious endophthalmitis, rhgmatogenous retinal detachment , or proliferative vitreo retinopathy in this study .
Jonas et al. [19] found the reduction of visual acuity started 4-5 months after initial increase in visual acuity two months after injection. Similarly, in the present study after initial increase of vision two month after injection, visual performance started to decrease again. This may be result from resolving of trimacinolone acetate crystals Vascular endothelial growth factor (VEGF) plays an important role in the pathogenesis of AMD 22 Intravitreal bevacizumab injection was reported to be effective for treatment exudative AMD. Bevacizumab inhibit VEGF, decrease angiogenesis and decrease vascular permeability. [23-25].
In group 2, there were increase in visual acuity, reduction in retinal thickness and improvement of electrophysiological amplitudes and latencies. The improvement was slightly more significant in group 2 than in group 1 (As seen in Table 1) The cause for this improvement in group 2 more than group 2 is that triamcinolone exerted its antiangiogenic effect by enhancing endostatin expression rather than suppressing VEGF expression [26]. While bevacizumab decrease angiogenesis by decreasing VEGF expression and enhancing endostatin [27]. There was correlation between visual acuity and central macular thickness (p=0.006, R=0.55) and visual acuity and MFERG amplitude (P=0.005, R=0.65). Also, there was significant correlation between central macular thickness and MFERG amplitude (P=0.003, R=0.6) in group 2. Similarly, Rosenfeld et al reported that intravitreal injection of bevacizumab cause marked decrease in retinal thickness without toxicity [28]. Ahmadieh et al. observed improvement of vision and reduction of thickness after bevacizumab [29]. Also, Falkenstein et al showed that primary bevacizumab therapy resulted in significantly visual improvement [30]. The bevacizumab preparation is unpreserved and contains no ingredients that are toxic to the eye [28]. Intravitreal bevacizumab is well tolerated in the majority of patients. In this study, there were no complications in group 2. Only subconjuctival heamorrhage in two cases which resolved within a week. While, Ahmadieh et al. [29]. Observed one case with pigment epithelial detachment without any cases of endophalmitis or sub-conjuctival haemorrhage [29]. Also, Cleary et al. [30]. Found endophthalmitis in 1 of 112 eyes, submacular hemorrhage in 3 of 112 eyes and retinal pigment epithelial tears in 3 of112 eyes. Ronan et al. [31], and Avery said that the presence of pigment epithelial detachment was risk factor for retinal pigment epithelial tear after IVB injection [32]. The limitations of this study were the method of measuring visual acuity. Instead of the charts used for the Early Treatment Diabetic Retinopathy [33], visual acuity was determined using Snellen charts. But, the same method was used to three groups. Other limitation of this study was limited follow up and limited number of the patients, the relatively high dose of trimacinolone acetate injected into eye. In summary, intravitreal injection of trimacinolone acetate and bevacizumab improve visual acuity transiently in patients with neovascular age related macular degeneration. Furthermore, intravitreal injection caused anatomical changes and functional improvement of MFERG. Bevacizumab gave more favorable visual outcome and anatomical and functional improvement than triamcinolone acetate. To stabilize visual acuity, repeated intravitreal injection is recommended with 2-3 months apart with take care of complication especially intraocular pressure in cases of IVTA.
References
- Vingerling JR, Dielemans I, Hofman A (1995) The prevalence of age- related maculopathy in the Rotterdam Study. Ophthalmology 102(2): 205-210.
- Becerra E, Morescalchi F, Gandolfo F, Danzi P, Nascimbeni G, et al. (2011) Cliical evidence of intravitreal triamcinolone acetonide in the management of age related macular degeneration. Curr Drug Targets 12(2): 149-172.
- Gholam PA, Darius M Intravitreal trimacinolone acetonide. Retina 24: 488-50.
- Augustin AJ, Puls S, Offermann I (2007) Triple therapy for choroidalneovascularization due to age-related macular degeneration: verteporfin PDT, bevacizumab, and dexamethasone. Retina 27(2): 133140.
- Luke M, Warga M, Ziemssen F, Gelisken F (2006) Effects of bevacizumab on retinal function in isolated vertebrate retina. Br J Ophthalmol 90(9): 1178-1182.
- Maluri RK, Laura A, Bleau LPN, Donald L, Wilson M (2006) Electrophysiologic findings after intravitreal Bevacizumab (Avastin) treatment. Retina 26(3): 270-274.
- Sutter EE, Tan D (1992) The field topography of ERG Components in men, I: the photopic luminance response. Vision Res 32(3): 433-446.
- Mc Culloch DL,Marmor MF, Brigell MG, Hamilton R, Holder G, set al. (2015) ISCEV Standard for full-field clinical electroretinography. Doc Ophthalmol 130(1): 1-12.
- Hood DC, Li j A (1997) Technique for measuring individual multifocal ERG records. In : Yages D, (edn). Non invasive assessment of the visual system . Trends in optic and photonics11: 280-283.
- Hood DC, Seiple W, Holopigien K (1997) A Comparison of the Components of multifocal and full field ERG. Vis Neuro Sci 14: 533-544.
- Grover S, Fishman GA, Birch DG, Locke KG, Rosner B (2003) Variability of full-field electroretinogram responses in subjects without diffuse photoreceptor cell disease. Ophthalmology 110(6): 1159-1163.
- Schimdt-Erfurth U, Miller JWS, Sickenberg M (1991) Photodynamic therapy with verteporfm for choroidal neovascularization by age related macular degeneration. Arch Ophthalmology 17: 1177-1187.
- Penfold PL, Gyory JF, Hunyor AB, Billson FA (1995) Exudative macular degeneration and intravitreal trimacinolone. Aust NZJ Ophthalmology 23(4): 293-298.
- Ciulla TA, Criswell MH, Danis RP (2001) Intravitreal triamcinolone acetonide inhibits choroidal neovascularization in a laser-treated rat model. Arch Ophthalmol 119(3): 399-404.
- Penfold PL (2002) Intravitreal trimacinolone in recurrence of choroidal neovascularization. Br J Ophthalmology 86(6): 600-601.
- Chella JK, Gillies MC, Penfold PL, Gyory JF, Hunyor AB, (1998) Exudative macular degeneration and intravitreal trimacinolone acetenoid;18 months follow up. Aust NZJ Ophthalmology 26(4): 277-281.
- Danis RP, Ciulla TA, Pratt LM, Anliker W (2000) Intravitreal trimacinolone acetenoid in exudative age related macular degeneration. Retina 20(3): 244-250.
- Ranson NT, Danis RP, Ciulla TA, Pratt LM (2002) Intravitreal trimacinolone in subfoveal recurrence of choroidal neovascularization after laser treatment in macular degeneration. Br J Ophthalmology 86(5): 527-529.
- Jonas JB, Kreissing I, Hugger P, Sauder G, Panda-Janas S (2003) Intravitreal trimacinolone acetenoide for exudative age related macular degeneration. Br J Ophthalmology 87(4): 462-468.
- Jonas JB, Akkoyun I, Budde WM, Kreissing I, Degenring RF (2004) Intravitreal reinjection of trimacinolone for exudative age related macular degeneration. Arch Ophthalmology 122(2): 218-222.
- Gillis MC, Lao W, Chua W (2001) The efficacy of a single intravitreal injection of trimacinolone for neovascular age related macular degeneration, One year results of randomized clinical trial IVTA .Invest Ophthalmology Vis Sci 42: 437-439.?
- Augustin AJ, Puls S, Offermann I (2007) Triple therapy for choroidal neovascularization due to age-related macular degeneration: verteporfin PDT, bevacizumab, and dexamethasone. Retina 27(2): 133140.
- Wingate RJ, Beaumont PE (1999) Intravitreal trimacinolone and elevated intraocular pressure. Aust NZJ phthalmology 27(6): 431-432.
- Van Wijngaarden P, Coster DJ, William KN (2005) Inhibitors of ocular neovascularization: promises and potential problems. JAMA 293(12): 1509-1513.
- Arevalo JF, Fromow-Guerra J, Sanchez JG, Maia M, Berrocal MH (2008) Primary intravitreal bevacizumab for subfoveal choroidal neovascularization in age related macular degeneration: results of the Pan-American Collaborative Retina Study Group at 12 months follow- up. Retina 28(10): 1387-1394.
- Tatar O, Shinodo K, Kaiserling E (2008) Early effects of triamcinolone on vascular endothelial growth factor and endostatin in human choroidal neovascularization. Arch Ophthalmol 126(2): 193-199.
- Tatar O, Shinoda K, Kaiserling E (2009) Tubingen Bevacizumab Study Group, Grisanti S. Implications of bevacizumab on vascular endothelial growth factor and endostatin in human choroidal neovascularisation. Br J Ophthalmol 93(2): 159-165.
- Rosenfeld PJ, Moshfeghi AA, Puliafito CA (2005) Optical coherence tomography findings after intravitreal injection of bevacizumab (Avastin) for neovascular age-related macular degeneration. Ophthalmic Surg Laser Imaging 36(4): 331-335.
- Ahmadieh H, Taer R, Riazi-esfahani M, PIRI N (2011) Macular degeneration intravitreal bavacizumab versus combined intravitreal bevacizumab and triamacinolone for neovascular age related .Retina 31(9): 1819-1826.
- Cleary CA, Jungkim S, Ravikumar K (2008) Intravitreal bevacizumab in the treatment of neovascular age-related macular degeneration, 6-and 9-month results. Eye 22(1): 82-86.
- Ronan SM, Yoganathan P, Chien FY (2007) Retinal pigment epithelium tears after intravitreal injection of bevacizumab (Avastin) for neovascular age-related macular degeneration. Retina 27(5):535-540.
- Avery RL, Pieramici DJ, Melvin D, Rabena BS (2006) Intravitreal bevacizumab (avastin) for neovascular age related macular degeneration. Ophthalmology 113(3): 363-372.
- Falkenstein IA, Cheng L, Morrison VL (2007) Standardized visual acuity results associated with primary versus secondary bevacizumab (Avastin) treatment for choroidal neovascularization in age-related macular degeneration. Retina 27(6): 701-706.






























