Lived Reality and Impacts Of COVID-19 on Nurses Who Provided Care in The First Wave on Brazilian Amazon
Marcos Miranda R1, Josivane Quaresma T1, Marceli Batista ML2, Marcos Jessé Abrahão S1,*, Ligia Regina Franco SK3, Bernard Carl K4, Karla Valéria BL5, Luana Nepomuceno Gondim CL5
1Postgraduate Program in Epidemiology and Health Surveillance (PPGEVS), Evandro Chagas Institute (IEC), Ananindeua, Pará, Brazil
2Postgraduate Program in Zoology (PPGZOO), Federal University of Pará (UFPA), Emilio Goeldi Museum (MPEG), Belém, Pará, Brazil
3Medicine Faculty Department, Federal University of Ceará (UFC), Fortaleza, Ceará, Brazil
4Department of Global Community Health and Behavioral Sciences, Tulane School of Public Health and Tropical Medicine, New Orleans, LA, United States of America
5Bacteriology and Mycology Section, Evandro Chagas Institute (IEC), Ananindeua, Pará, Brazil
Submission: June 1, 2024; Published: June 28, 2024
*Corresponding author: Marcos Jessé Abrahão Silva, Postgraduate Program in Epidemiology and Health Surveillance (PPGEVS), Evandro Chagas Institute (IEC), Ananindeua, Pará, Brazil, Email: jesseabrahao10@gmail.com
How to cite this article: Marcos Miranda R, Josivane Quaresma T, Marceli Batista ML, Marcos Jessé Abrahão S, Ligia Regina Franco SK, et al. Lived Reality and Impacts Of COVID-19 on Nurses Who Provided Care in The First Wave on Brazilian Amazon. JOJ Nurse Health Care. 2024; 13(4): 555869. DOI:10.19080/JOJNHC.2024.13.555869
Abstract
COVID-19 is an infectious disease caused by SARS-CoV-2, which was responsible for causing incalculable damage to humanity, especially during the 1st pandemic wave, which corresponds to a unique, disastrous, and emergency public health event global. In this sense, the individuals considered most exposed to the virus were frontline professionals, such as nurses. The purpose of this work was to evaluate the effects of the work activity of nurses who aid suspected or confirmed cases of SARS-CoV-2 on their health. This is a cross-sectional study, with RDS sampling carried out in the metropolitan region of Belém. To evaluate the mental/emotional impacts, the following were used: SRQ-20; AUDIT C; PHQ-9; GAD-7; PCL-5. If the score obtained on the SQR-20 was > 8 and on the AUDIT-C was > 6, they were directed to the PHQ-9, GAD-7 and PCL-5 instruments. Data were analyzed using the Chi-Square test in a bivariate method. Only 69.10% of nurses were tested for SARS-CoV-2 with a positivity rate of 70.73%. A significant association was found between positive cases and symptoms. The unavailability of PPE with surgical mask with gloves applied with 71.35%, and external cap, with 80.34% were observed. In positive cases, non-use of waterproof jackets was 24.39% and easy protection jackets were 21.95%. For anxiety and post-traumatic stress tests, 44.63% of nurses presented some common mental disorder after being evaluated by the SQR-20. The study data confirmed the severity of the vulnerability of the nursing class and emphasized the vulnerabilities to which this category is susceptible.
Keywords: COVID-19; Nurses; Worker’s health; SARS-CoV-2; Public Health
Abbreviation: STROBE: Strengthening the Reporting of Observational Studies in Epidemiology; RDS: Respondent-Driven Sampling; AUDIT: Alcohol Use Disorders Identification Test; GAD-7: General Anxiety Disorder-7; SRQ: Self Report Questionnaire; PCL-F: Posttraumatic Stress Disorder Checklist for DSM-5; PPE: Personal Protective Equipment; CMD: Common Mental Disorder
Introduction
The new SARS-CoV-2 began in the city of Wuhan in the province of Hubei in China in 2019 and spread rapidly around the world, causing high numbers of cases and deaths, which led to the collapse of health systems in several countries. whether due to the lack of beds, medicines and supplies, as well as the availability of protective equipment for health professionals [1]. Health workers in their various categories had to deal directly with patients infected by COVID-19, leaving them in a vulnerable situation. The care provided to patients infected by SARS-CoV-2 is intense, inevitable and involves several procedures in the respiratory tract that increase the possibility of dissemination and favor contamination [2]. As a result, infections of healthcare professionals can occur due to a failure in protective measures or the absence of personal protective equipment (surgical masks, PFF2 and clothing) [3]. The absence of personal protective equipment violates both global recommendations and regulatory standard 32 (NR 32), one of the main pieces of legislation for Brazilian health professionals, which aims to establish basic guidelines for the implementation of safety protection measures. and the health of health service workers, as well as those who carry out health promotion and assistance activities in general [4].
Nurses have played an extraordinary role in the fight against COVID-19, however, these professionals are susceptible to contamination through direct exposure to infected patients [5]. Furthermore, during the complex care process, they are faced with stressful situations such as constant use of personal protective equipment linked to long working hours and work overload, leading to strong physical/emotional exhaustion [6]. The assistance provided to those infected with SARS-CoV-2 has generated emotional changes, as highlighted by a study carried out in China, 25% (n= 44) had severe anxiety [7]. Likewise, another study identified that 47.52% and 56.74 % of nurses working against COVID-19 had anxiety and depression respectively [8]. Therefore, this article evaluated the main impacts of COVID-19 on nurses who provided care to suspected or confirmed cases of SARS-CoV-2 in the metropolitan region of Belém in 2021.
Material and Methods
The research was conducted in accordance with the ethical precepts stipulated by the Declaration of Helsinki, and its protocol was approved by the Research Ethics Committee of FIOCRUZ campus Instituto Aggeu Magalhães (authorization number 4021099). All participants signed their written consent before starting the evaluation stage through an ICF. The methodological procedures were reported in accordance with STROBE - Strengthening the Reporting of Observational Studies in Epidemiology.
This Study was carried out in the metropolitan region of Belém, Pará, northern Brazil. Comprising 7 municipalities (Belém, Ananindeua, Marituba, Benevides and Santa Bárbara, Santa Izabel and Castanhal) and totaling 2,505,242 inhabitants according to IBGE estimates, with the majority of the population residing in urban areas [9]. The first case of COVID-19 in the city of Belém was registered on March 18, 2020.
Cross-sectional study with 178 nurses from different levels of complexity of the Health System of Belém - PA. The recruitment of research participants used the sampling technique known as Respondent-Driven Sampling (RDS) developed by Heckathorn in 1997 and was widely known and used in studies on HIV/AIDS [10]. RDS replaces the snowball sampling technique, as it uses a mathematical model that weights the sample to compensate for the fact that the collection was done non-randomly [10]. Thus, three nurses were selected who were called “seeds”, who, after answering the questionnaire, invited three professional colleagues (nurses) through a WhatsApp message, expanding the study population through their contact chains and so on until reaching the sample of 178 professionals. In this way, all participants were contacted via telephone message, in which the research was guided and a link was sent that guaranteed access to the informed consent form and the digital questionnaire.
The digital questionnaire used in this study was an adaptation based on the WHO Guide for risk assessment of health professionals (2020). The following variables were evaluated: sex, age, race, comorbidities, place of work, work sector, number of places where they work, adherence to the use of PPE, work overload, training in the use of PPE, accidents with biological material, symptoms suggestive of COVID-19.
To assess the mental/emotional impacts, five validated instruments were used: the Self Report Questionnaire (SRQ- 20) that assesses mental suffering; o Alcohol Use Disorders Identification Test (AUDIT C), used to check the harmful consumption of alcoholic beverages, Patient Health Questionnaire (PHQ-9), a tool used to identify signs of depression; O General Anxiety Disorder-7 (GAD-7), responsible for checking the presence of anxiety, and the Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5) , which assesses the possible presence of posttraumatic stress. Thus, a flow was created in which participants responded first to the validated instruments SQR-20 and AUDIT - C. If the score obtained in the SQR-20 was > 8 and in the AUDIT-C was > 6, they were directed to the PHQ-9 instruments, GAD-7 and PCL-5.
The frequency of positivity of nurses participating in the study was assessed through self-reporting of positivity using the rapid test and/or RT-PCR, correlating with the variables from the WHO questionnaire and the instruments for assessing mental/emotional impacts. The data was organized and coded in Excel 2019 and will be submitted in Statistical Analysis. The variables were presented in absolute and relative frequencies. For categorical variables, bivariate analyzes were performed using Chi-square statistical tests of independence (table 2x2).
Results
The study population consisted of 178 nurses with a predominance of female participants at 73.03% (n=130). The most prevalent age group was between 30 and 39 years old with 48.31% (n=86). Regarding comorbidities, it was found that 71.35% (n=127) of participants reported having no previous pathologies, while 28.65% (n=51) marked “yes” in this item. The most common comorbidities were arterial hypertension with 10.67% (n=19) and obesity 10.11% (n=18).
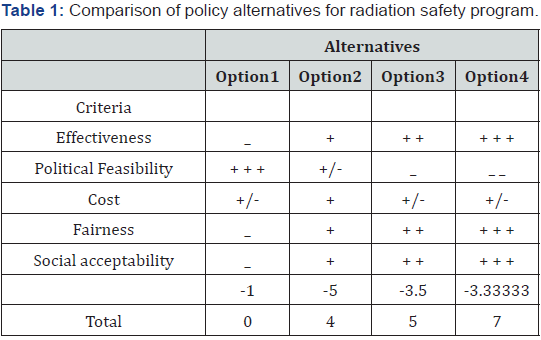
For the workplace, 88.76% (n=76%) reported having 01 or 02 employment relationships and 11.24% (n=20) reported having between 3 and 4 jobs. The most prevalent workplaces were the public hospital with 58.43% (n=104), followed by the private hospital with 22.47% (n=40). The most mentioned work environment was the ICU with 38.20% (n=68), followed by the emergency 33.71% (n=60) (Table 1).




It was reported by 35.96% (n=64) of those interviewed that they had not received any training in the use of PPE. For the use of disposable gloves, it was evident that 71.35% (n=127) of the interviewees marked the option that indicated they were not available in the service , as well as 19.10% (n=34) marked the option “never use”. Regarding the use of a PFF2 mask (N95), 64.61% (n=115) responded “not available at the service”, while 18.54% (n=33) reported “never” using it. For the surgical mask, it was evident that 40.45% (n=72) of the interviewees did not have this equipment in service and 25.28% (n=45) used it sometimes (Table 2).
In the item that indicated the use of a face shield, the option “sometimes” (<50%) had 43.82% (n=78), followed by the option “never use” with 19.10% (n=34). regarding the use of protective glasses, 41.01% (n=73) responded that they used them sometimes, while the option that “indicated never use” had 21.35% (n=38) of responses, while the option “did not have in the service” was reported by 17.98% (n=32) (Table 2). In the items that assessed the use of gowns, 54.49% (n=97) responded that they did not have a disposable surgical gown available in the service, and 19.66% (n=35) reported not having a waterproof gown available. The option “never use this equipment” was answered by 20.79% (n=37) and 17.98% (n=32) respectively, for disposable and waterproof coats (Table 2). In the question that assessed the use of disposable caps, it was shown that 80.34% (n=143) did not have this Epi available in the service. For the use of disposable props , only 8.43% (n=15) responded that they always used them, and 27.53% (n=49) that this item was not available in the service (Table 2).
Most nurses, 85.39% (n=152), responded that they participated in procedures with greater exposure to SAR-CoV-2 contamination. In the question that assessed the use of PPE during the performance of the most invasive procedures, participants reported percentages similar to those mentioned previously, in which the unavailability of disposable gloves in the service was 79.21% (n=141), as well as, N95 mask with 69.66% (n= 124) and disposable hat with 71.91% (n=128) (Table 3).
In the assessment of accidents with biological material , 87.64% (n=156) of the interviewees indicated that they had not suffered this injury, regarding the risk of being infected by COVID-19, 43.26% (n=77) of the nurses responded that are characterized as high risk (Table 4).
Regarding the test for COVID-19, any of the tests were considered: RT-PCR, serology and rapid test. Thus, the interviewees answered whether they had carried out any of these tests, showing that only 69.10% (n=123) of nurses had been tested. Among the professionals tested, 70.74% (n=87) were positive for SARSCoV- 2, while 29.27% (n=36) were negative (Table 5).
To analyze the factors associated with SARS-CoV-2 positivity in nurses, we compared the positive and negative results of serological tests or real-time PCR. However, only 123 were tested for COVID-19 with 70.73% (n=87) positive (Table 6). The age group with the highest positivity was between 30 and 49 years old with 54.48% (n=67) of participants. Positivity in women was 44.72% (n=55) and in men it was 26.02% (n=32). The race with the highest number of positive cases in the study was brown with 43.09% (n=53), followed by Caucasian race with 18.70% (n=23) and Afro-Brazilian race with 8.13% (n=10) (Table 6).
Regarding comorbidities, it was possible to identify that 65.85% (n=81) of the professionals who took the test responded that they did not have any. Hypertension and obesity were the most prevalent pathologies among nurses tested positive with 9.76% (n=12) and 10.57% (n=13), respectively (Table 6). In relation to workplaces and the positivity of those interviewed, there was a predominance of public hospitals with 39.84% (n=49), followed by private hospitals with 13.82% (n=17). For the non-use of personal protective equipment (PPE), it was identified that positive cases had a higher percentage, with “not using a waterproof coat” being the most reported with 24.39% (n =30), followed by “not using face shield” with 21.95% (n= 27) (Table 6).





*NOTE: Among the 178 participants in the questionnaire, 177 participants actually answered the questions, 1 person did not answer anything in the questions, so although 123 were tested for covid, only 122 were tested for covid-19 and answered the questions, being that of these 122, only 45 (36.88%) passed to the second phase of the mental health test considering the cutoff score >8 of the SQR test and/or >6 of the AUDIT-C
Of the 123 nurses tested, 65.85% (n=81) stated that they had received training in the use of PPE and of these, 82.84% (n=59) tested positive for COVID-19. For accidents with biological material, 13.01% (n=16) of the participants claimed to have suffered some injury, among these, 68.75% (n=11) were positive for SARS-Cov-2. Regarding symptoms suggestive of COVID-19, 101 professionals responded to this question with positivity for 81.19% (n=82) (Table 6).
In the assessment of mental health, not all professionals were directed to all questionnaires. The SRQ-20 and AUDIT C were answered by 177 participants, however, according to the criteria adopted in the methodology, only 53 participants reached the minimum cut-off scores (SRQ-20 > 8 and or AUDIT-C > 6) ( Table 7 and 8) and were directed to answer PHQ-9, GAD-7, PCL-5 . In the SRQ-20 responses - it was identified that sleeping poorly was a common characteristic for 54.80% (n=97) of respondents, “feeling nervous, tense and worried” common for 54.80% (n=97) of those interviewed, followed by the feeling of tiredness (52.54%; n=93) (Table 7).
When analyzing the score obtained by the group of interviewees in general, it was identified that 177 participants answered SQR 20, and that 29.94% (n = 53) reached the cutoff score > 8 . No participant reached the maximum score of 20 points, however 2.82% (n=5) of nurses had a score of 16, which indicates a high degree of mental suffering (Table 8).
To assess the risks of alcohol use in nurses, the AUDIT C tool was used, making it possible to identify that 47.46% (n=84) of participants had a score of zero, indicating no risk. No interviewee reached the maximum score of 12 points, but 11 nurses had a score of 6 to 7, indicating a high risk, while 3 nurses achieved a score between 8 and 12, indicating a severe risk for alcohol use (Table 9).
The AUDIT-C score is made on a scale of 0 to 12 points. Each question on the instrument has five answer options, allowing a score of 0 to 4 for each: a = 0 points, b = 1 points, c = 2 points, d = 3 points, e = 4 points. For men, a score of 0 to 3 is considered low risk; between 4 and 5 points, moderate risk; between 6 and 7 points, high risk and 8 to 12 points, severe risk. For women, a score of 0 to 2 is considered low risk; between 3 and 5 points, moderate risk; between 6 and 7 points, high risk and between 8 and 12 points, severe risk.
Regarding the nurses’ mental health scales, we descriptively present the average positive and negative scores. However, the sample number was reduced to 122 nurses who declared that they had been tested for COVID-19. Of the 122 professionals who answered the SRQ-20, 86 were positive for SARS-CoV-2, there was no significant difference in the average score between positive and negative. In AUDIT-C, also answered by 122 nurses, there was a slight difference between the means. For follow-up mental health assessment, 36.88% (n=45) of participants met the scoring and positivity criteria. At PHQ-9 the average score was higher in positives (9.26), the same happened with GAD-7 and PCL-5 (Table 10).
Discussion
The study in question showed a significant female participation, which reflects the demographic profile of nurses in Brazil, where historically nursing is predominantly carried out by women [11]. The age distribution of participants showed that the predominant age range was 30 to 39 years old, however, 21.91% were professionals under 30 years old, young people working on the front line of COVID-19, possibly professionals without much experience. At the other end of the age range were 5.06% of nurses over the age of 50, showing that even at considerably more vulnerable ages and with the possibility of having more comorbidities, these professionals continued to perform their duties in a high-risk environment.
The presence of comorbidities in this study was reported by a significant number of participants (28.65%), with high blood pressure and obesity being the most reported, which belong to the group of diseases that lead to an outcome adverse effect in patients with COVID-19 [12]. It was possible to demonstrate that nurses were mostly linked to public health care institutions and many of them had more than one employment relationship. This shows the reality of nursing, where nurses need to work double or triple shifts to ensure sufficient income to support their families. This can considerably affect their physical and mental health as excessive work leads to burnout and consequently to absence from work and risk to the care provided to patients [13].
It was identified that more than 64% of nurses received training at some point during the pandemic to use PPE. However, one relevant fact caught our attention: the lack of basic protective equipment such as gloves, masks, glasses and surgical gowns [14]. The item that checked the availability of these instruments in service, the options “never” or “sometimes (<50)” were considerably marked. The unavailability of these PPEs goes against the recommendations of both Anvisa and the WHO, in which health professionals who are involved in the direct care of patients with COVID-19 must use the equipment. Likewise, the Ministry of Labor and Employment established the basic guidelines for the implementation of measures to protect worker health and safety, requiring health services to comply with Regulatory Norms such as NR 32, which recommends the adoption of preventive and training workers for safe work [15].
Exposure to situations considerably more likely to eliminate aerosols or droplets, such as intubation, aspirations or resuscitation, was witnessed by more than 85% of the nurses interviewed, which fundamentally corroborates the need for availability of PPE, as well as its use by of these professionals. However, we found significant percentages of nurses who were not using their equipment, again due to the unavailability of this item in their services [16,17]. The unavailability or non-use of protective equipment predisposes to the risk of accidents with biological material such as blood or secretions. However, in this study, the percentage of nurses who suffered an accident was relatively low. Accident with biological material is defined as any direct or indirect exposure of a worker to biological (organic) material potentially contaminated by pathogens (viruses, bacteria, fungi, prions and protozoa), through sharp or non- sharp material [15,17]. The perception of the risks of contamination by COVID-19 was evident when approximately 80.9% (n=144) of nurses indicated a high to very high risk of being infected. A similar study published by Fernandez et al, 2021 identified that 78.9% of nurses received sufficient protective equipment and yet 63.20% stated that they felt unsafe even when using PPE [18].
We identified that 69.10% (n=123) of interviewees had been tested for SARS-CoV-2 at the time of the research, showing that even 1 year into the pandemic there were still many professionals who had not been tested. The prevalence of tested and positive participants in our study was higher than in other studies. In the publication by Buonafine et al., (2020) carried out in the city of São Paulo, Brazil, a positivity rate of 42% of health professionals was found, while in the publication by Schmitd Fernandes et al. [19] carried out in Porte Alegre, Brazil was reported 14% positivity [19].
Symptoms suggestive of COVID-19 were associated with test positivity (p<0.001). Likewise, research carried out by Coelho et al. [20] in the state of Ceará, Brazil, showed that 53% of the professionals surveyed showed signs and symptoms of COVID-19, among these 58% obtained a positive result (active infection or presence of antibodies), making a prevalence of 23.9% of the illness among participants [20].
We identified that the age group 30 to 49 years was the most prevalent in positive cases, which represented more than 54% of the sample analyzed.
In terms of race, the study identified that nurses who declared themselves mixed race were the most frequent, followed by caucasians and afro-Brazilian race. This reflects the classification of the Brazilian population, which is mainly made up of afro- Brazilian and brown people (53.92%), followed by Caucasian people (45.22%), yellow people (0.47%) and indigenous people (0.38%) [17].
Regarding comorbidities, hypertension and obesity were the most prevalent among positive nurses, but it was not possible to make a significant statistical correlation with positivity. However, these percentages were higher than those found in the study carried out by Püschel et al. [21] with nursing professionals, in which obesity was identified in 4.8%, diabetes in 3.1% and high blood pressure in 5.01% [21].
When we analyzed the workplace, we observed that the highest percentage of positive cases was in public institutions, especially public hospitals, which can be justified by the fact that 70.73% of nurses reported working in hospitals. However, we did not find statistical significance between workplace and positivity for SARS-CoV-2. However, research by Coelho et al. [20] managed to identify a significant association between coronavirus infection and whether the workplace was in the hospital or UPA, in which 62.8% tested positive (p=0.001).
In the analysis of the use of N95 masks, it was identified that the percentage of those who stopped using the mask was higher in positive cases, 18.70% (n=23), indicating that many nurses were caring for patients with COVID-19 without proper attire even the health of professionals is essential. In the study by Neto et al. [22] identified that 32.8% of healthcare professionals had already performed a procedure involving aerosol dispensing without using an N95 mask [22]. Although constant updates from the WHO and Ministry of Health reinforce the importance of PPE, several professionals reported the lack of these and/or the use of inappropriate materials during work activities, further worsening biosafety in health services. The types of PPE required to prevent COVID-19 in healthcare services are based on the activities performed and the biological risk to which professionals are exposed [19].
Having undergone training in the use of PPE in relation to positivity for SARS-CoV-2 did not prove to be statistically significant, however it is an issue that deserves to be highlighted as it is one of the measures cited by publications and guided by entities such as WHO to reduce the risks that professionals are exposed.
Accidents with biological material were rarely reported, and of the 16 participants who had an accident with biological material, 68.94% reported having tested positive, but without statistical significance. In the study by Aragão et al. (2019) a frequency of 53.9% of accidents involving biological material was reported, with sharp instruments being the most prevalent.
In the SQR-20 analysis, it was observed that more than half of these professionals were being impacted in some way by the difficult aspects involving the pandemic. In terms of feeling nervous, tense and worried, it showed the impacts that COVID-19 brought to the nurses interviewed, similar to those found in another study by Maier and Kanunfre [23], in which the presence of stress was predominant in nurses who work in the hospital sector, reaching 78% [23]. The feeling of tiredness felt over time reflected a common feeling among many nursing professionals who are subjected to long working hours and little free time to rest, as demonstrated in the study by Tomaszewska et al. [24], in which 56.9% of nurses interviewed reported working overtime, 49.2% reported a lack of free time and 49.2% stated that nurses’ work during the pandemic was more stressful [24].
The question that assessed “the feeling of feeling sad lately” indicated that a considerable portion of nurses were having problems assimilating the difficulties experienced during the pandemic, whether due to deaths, overwork and fear of becoming infected or taking it to the family. In this sense, the article by Noh et al. [25] corroborates the analysis, as it identified in South Korea that 55.9% of COVID-19 frontline nurses experienced high levels of general exhaustion and a 17.4% prevalence of mild to extremely severe depression [25].
It was identified with the SRQ-20 instrument that 29.94% of respondents were suffering from some common mental disorder (CMD). Similar to the study by Ribeiro et al [26], in which a significant percentage (37%) of participants also had CMD [26]. When using AUDIT-C, it was observed that professionals were not exhibiting excessive alcohol consumption, which is similar to those obtained by Cedrone et al. [27], in which 54.87% (n= 486) of women and 45.13% (n= 385) of men, Italian health professionals, were at low risk for harmful consumption of alcoholic beverages [27]. For the high-risk and moderate-risk categories of alcohol consumption, a low prevalence was identified in the present study, however in the study by Cedrone et al. [27], this percentage was higher, present in 35.96% (n= 114) for men and 64.04% (n=203) for women [27].
PHQ-9, GAD -7 and PCL-5 instruments , it was possible to identify that 28.75% (n=45) of the interviewees had significant emotional distress to the point to be directed to other assessment instruments. Furthermore, it is possible to identify that the general average in each instrument was higher in positive cases compared to negative cases, indicating that COVID-19 had real mental impacts on these professionals.
The overall average for the PHQ-9 of both positive and negative cases was within the values indicative of mild depression (7 to 10), similarly identified in the study by Zhou et al. [28], with 963 health professionals from Hubei, where the prevalence of mild depression was 34% [28].
For the GAD-7 instrument, it was possible to identify an association between the psychological health of health professionals and positivity for COVID-19. Nurses who reported being positive for COVID-19 had a higher average compared to those who were negative, indicating an increase in anxiety. A similar fact was found by both Hariri et al. [29] and by Martínez et al. [30] in which 24.32% and 53.6%, respectively, of health professionals presented anxiety symptoms ranging from mild to severe [29,30]. The average PCL-5 score was also higher in respondents positive for SARS-CoV-2 compared to those negative, which may indicate greater suffering in those who had the infection, but as it is an average, we cannot indicate the degree of suffering of the analyzed group.
The limiting factors of the research were the difficulty of health professionals in accepting to participate in the project, not answering the questionnaire completely, even though they stated that they would respond, and not passing on the link generated to other research participants.
The methodological advantage of the research was the use of an electronic form with objective double-alternative questions (yes or no) and an application time of approximately 15 minutes, as well as total confidentiality of the information and respect for the recommendations of the season of non-crowding or direct contact, online only. Additionally, the use of RDS reduced the potential bias of previous methodologies, controlling the bias resulting from differences in the size of contact networks, that is, each participant had a limited number of links to send to colleagues.
It is expected that the results found in this study can serve to improve professional practice in facing future pandemics, as well as serve as a theoretical basis for new publications.
Conclusions
It was possible to demonstrate that only 69.10% of nurses were tested for SARS-CoV-2 with a positivity rate of 70.73%. Furthermore, a significant association was found between positive cases and having had symptoms of COVID-19. For positive nurses, the most frequently cited comorbidities were hypertension and obesity. The unavailability was observed mainly of PPE with surgical mask with 40.45%, surgical gowns with 54.49%, pff2 mask (N95) with 64.61%, disposable gloves with 71.35%, and disposable cap, with 80.34%. In positive cases, we identified significant percentages of non-use of a waterproof coat with 24.39% and an easy protector with 21.95%.
It was identified that many nurses worked in more than one location and the public service showed the biggest difference between the number of nurses positive and negative for SARSCoV- 2. Furthermore, it was identified that only 13.01% of participants reported some type of accident with biological material, with a prevalence of 68.75% among positive nurses.
For anxiety and post-traumatic stress tests, it was observed that the average was higher in individuals who tested positive for COVID-19 and that 44.63% of nurses had some common mental disorder after being evaluated by the SQR-20. In the assessment of alcohol abuse, we identified a low risk of harmful alcohol consumption.
The COVID-19 pandemic had serious impacts on nurses, mainly due to the overload of work linked to the lack of conditions for professional practice, leading to serious changes in the mental health of these professionals. The data collected by this study highlighted the weaknesses that this category is exposed to and confirm how urgent the demands of the nursing class are.
Conflicts of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Author Contributions
MMR, JQT, and MBML designed the study. MJAS and MMR searched databases and performed the selection of studies. MJAS and MBML analyzed the data and wrote the manuscript. BCK and MMR performed the resources and software. LRFS and BCK done the visualization and validation of the article. LNGCL, KVBL, LRFS, BCK critically evaluated the review and commented on it. All authors read and approved the final manuscript.
Funding
None.
Acknowledgments
None.
References
- Ribeiro AP, Oliveira GL, Silva LS, Souza ERD (2020) Saúde e segurança de profissionais de saúde no atendimento a pacientes no contexto da pandemia de Covid-19: Revisão de literatura. Rev Brasil Saúde Ocupacional 45: e25.
- Nabuco G, Oliveira MHPP de, Afonso MPD (2020) The impact of COVID-19 pandemic on mental health: What is the role of Primary Health Care? Rev. bras. med. fam. Comunidade 2532-2532.
- Ehrlich H, McKenney M, Elkbuli A (2020) Protecting our healthcare workers during the COVID-19 pandemic. Am J Emergency Med 38(7): 1527.
- La-Rotta EIG, Garcia CS, Barbosa F, Santos AF dos, Vieira GMM, et al. (2013) Evaluation of the level of knowledge and compliance with standart precautions and the safety standard (NR-32) amongst physicians from a public university hospital, Brazil. Revista Brasileira de Epidemiologia 16: 786-797.
- Pereira MD, Torres EC, Pereira MD, Antunes PFS, Costa CFT (2020) Sofrimento emocional dos Enfermeiros no contexto hospitalar frente à pandemia de COVID-19. Res Soc Dev 9(8): e67985121-e67985121.
- Dos Santos Andrade TGV, da Silva Feitosa AB, de Souza Silva L, da Silva NMR (2022) COVID-19 and its negative impact on the mental health of health professionals: An integrative literature review. Rev Bras Med Trab 20(1): 132.
- Leng M, Wei L, Shi X, Cao G, Wei Y, et al. (2021) Mental distress and influencing factors in nurses caring for patients with COVID‐19. Nurs Critical Care 26(2): 94-101.
- Vitale E, Galatola V, Mea R (2021) Observational study on the potential psychological factors that affected Italian nurses involved in the COVID-19 health emergency. Acta Bio Medica: Atenei Parmensis 92(Suppl 2): e2021007.
- Del Pozo-Herce P, Garrido-García R, Santolalla-Arnedo I, Gea-Caballero V, García-Molina P, et al. (2021) Psychological impact on the nursing professionals of the rioja health service (Spain) due to the SARS-CoV-2 virus. Int J Environ Res Public Health 18(2): 580.
- Heckathorn DD, Semaan S, Broadhead RS, Hughes JJ (2002) Extensions of respondent-driven sampling: A new approach to the study of injection drug users aged 18-25. AIDS and Behav 6(1): 55-67.
- Li X, Zhou Y, Xu X (2021) Factors associated with the psychological well-being among front-line nurses exposed to COVID-2019 in China: A predictive study. J Nurs Management 29(2): 240-249.
- Russell CD, Lone NI, Baillie JK (2023) Comorbidities, multimorbidity and COVID-19. Nature Med 29(2): 334-343.
- Knight SR, Ho A, Pius R, Buchan I, Carson G, et al. (2020) Risk stratification of patients admitted to hospital with covid-19 using the ISARIC WHO Clinical Characterization Protocol: Development and validation of the 4C Mortality Score. BMJ 370.
- Santos JLG dos, Balsanelli AP, Freitas E de O, Menegon FHA, Carneiro IA, et al. (2021) Work environment of hospital nurses during the COVID‐19 pandemic in Brazil. Int Nurs Rev 68(2): 228-237.
- Oliveira MM de, Treichel CA dos S, Bakolis I, Alves PF, Coimbra VCC, et al. (2022) Mental health of nursing professionals during the COVID-19 pandemic: A cross-sectional study. Rev Saude Publica 56: 8.
- Muze M, Abdella B, Mustefa A, Ali A, Abdo A, et al. (2021) Availability of PPEs and training status of health professionals on COVID-19 in Silte Zone, Southern Ethiopia. Pan Afr Med J 39: 38.
- World Health Organization (2021) Infection prevention and control during health care when coronavirus disease (COVID-19) is suspected or confirmed: Interim guidance, World Health Organization.
- Fernandez M, Lotta G, Passos H, Cavalcanti P, Corrêa MG (2021) Condições de trabalho e percepções de profissionais de enfermagem que atuam no enfrentamento à covid-19 no Brasil. Saúde e Sociedade 30.
- Fernandes FS, Toniasso S de CC, Leitune JCB, Brum MCB, Leotti VB, et al. (2021) COVID-19 among healthcare workers in a Southern Brazilian Hospital and evaluation of a diagnostic strategy based on the RT-PCR test and retest for SARS-CoV-2. European review for medical and pharmacological sciences. Rome 25(8): 3365-3374.
- Coelho M de MF, Cavalcante VMV, Cabral RL, Oliveira RM, Nogueira PSF, et al. (2022) Work context and clinical manifestations of COVID-19 in health professionals. Acta Paulista de Enfermagem 35: eAPE0163345.
- Püschel VA de A, Fhon JRS, Nogueira L de S, Poveda V de B, Oliveira LB de, et al. (2022) Factors associated with infection and hospitalization due to COVID-19 in Nursing professionals: A cross-sectional study. Rev Lat Am Enfermagem 30: e3571.
- de Oliveira Neto GC, Tucci HNP, Godinho Filho M, Lucato WC, da Silva D (2022) Moderating effect of OHS actions based on WHO recommendations to mitigate the effects of COVID-19 in multinational companies. Process Saf Environ Prot 159: 652-661.
- Maier MDR, Kanunfre CC (2021) Impacto na saúde mental e qualidade do sono de profissionais da enfermagem durante pandemia da COVID-19. Revista Enfermagem UERJ 29: e61806.
- Tomaszewska K, Majchrowicz B, Snarska K, Telega D (2022) Stress and occupational burnout of nurses working with COVID-19 patients. Int J Environ Res Public Health 19(19): 12688.
- Noh EY, Park YH, Chai YJ, Kim HJ, Kim E (2022) Frontline nurses’ burnout and its associated factors during the COVID-19 pandemic in South Korea. Appl Nurs Res 67: 151622.
- Ribeiro WS, Grande AJ, Hoffmann MS, Ziebold C, McDaid D, et al. (2022) A systematic review of evidence-based interventions for child and adolescent mental health problems in low-and middle-income countries. Compr Psychiatry 121: 152358.
- Cedrone F, Buomprisco G, Nicola M, La Torre G, Nieto H, et al. (2022) Alcohol Use during COVID-19 Pandemic: A Cross-Sectional Survey among Healthcare and Office Workers in Italy. Int J Environ Res Public Health 19(19): 12587.
- Zhou ZQ, Yuan T, Tao XB, Huang L, Zhan YX, et al. (2022) Cross-sectional study of traumatic stress disorder in frontline nurses 6 mo after the outbreak of the COVID-19 in Wuhan. World J Psychiatry 12(2): 338.
- Harari YN (2020) The world after coronavirus. Financial times 20(3): 2020.
- Martínez Pajuelo AR, Irrazabal Ramos JE, Lazo-Porras M (2022) Anxiety, Depression, and Post-Traumatic Stress Disorder (PTSD) Symptomatology According to Gender in Health-Care Workers during the COVID-19 Pandemic in Peru Shortened Title: Psychological Impact of the Pandemic on Women. Int J Environ Res and Public Health 19(19): 11957.






























