Impacting Nurse’s Knowledge of Delirium and Management of Respiratory Depression through an Interprofessional, Patient-Centered Simulated Case Scenario
Cassandra Vonnes, Jo Ellen Warnke, Janelle Brown, Tina M Mason
H. Lee Moffitt Cancer Center and Research Institute in Tampa, Florida, United States
Submission: April 2, 2021; Published: April 14, 2021
*Corresponding author: Cassandra Vonnes, DNP, GNP-BC, APRN, AOCNP, CPHQ, FAHA, H. Lee Moffitt Cancer Center and Research Institute in Tampa, Florida, United States
How to cite this article: Cassandra V, Jo Ellen W, Janelle B, Tina M M. Impacting Nurse’s Knowledge of Delirium and Management of Respiratory Depression through an Interprofessional, Patient-Centered Simulated Case Scenario. JOJ Nurse Health Care. 2021; 12(1): 555828. DOI: 10.19080/JOJNHC.2021.12.555828.
Abstract
Introduction: Cancer patients experience delirium. It is critical to identify delirium early but also to distinguish the hypoactive presentation from respiratory depression. Inappropriate assessment may result in administration of high-risk reversal agents such as naloxone. Methods: To increase learning in nurse residents, simulation-based learning using standardized patients experiencing mixed delirium and respiratory depression augmented traditional didactic methods. The scenario included assessment, intervention, and psychomotor learning in administration of naloxone utilizing practice guidelines. Results: Delirium knowledge scores between traditional learning groups and oncology nurse residents enhanced with stimulation were compared. The Geriatric Institutional Assessment Profile knowledge score of oncology nurse residents who participated in simulation (5.91) was statistically significant (p<0.05) compared to all peer bed size, all peer teaching status, and all hospital groups. Oncology nurse residents scored higher than nurses receiving only the traditional delirium education. the appropriate use of naloxone was increased from 38% to 53% and the appropriate dosing went from 21% to 53%. Conclusions: Knowledge acquisition, as reflected by test score, does not always translate into clinical practice; however, simulation can provide application exercises for improving patient outcomes.
Key Points
Keywords:Delirium, GIAP, Nurse resident, Simulation, Naloxone
i. It is critical for oncology nurses to identify delirium early and intervene appropriately to reduce and prevent delirium-associated complications. ii. Simulation added to tradition teaching methods can enhance knowledge acquisition. iii. GIAP survey is a useful tool to assess attitudes, knowledge of guidelines and best practice, and perceived institutional strengths and barriers to best practice for care of older adult. iv. Oncology nurse residents participating in simulation learning scored higher on the GIAP than medical and surgical unit nurses on delirium dementia knowledge. v. Broadening the scope of simulation learning experiences to nurses, while utilizing patient outcome measures, may provide evidenced-based opportunities.
Introduction
Delirium is not uncommon in cancer patients during an acute hospitalization or in the terminal stages of cancer [1-3]. Iatrogenic delirium can complicate hospital stays for over 2.6 million older persons by increasing fall risk, restraint use, increased length of stay, and increased post-acute placement and costs [4]. Hypoactive delirium can be misdiagnosed and may be treated with reversal agents such as naloxone [5]. Added post-acute hospital costs due to an increased need for institutionalization, rehabilitation, and home care estimates are from $16,303 to $64,421 per patient [6-8].
Within the last 2 years, 19% to 28% of patients discharged from our center experienced at least one episode of delirium during their hospitalization. It is critical that nurses learn to assess for and identify delirium early and intervene appropriately to reduce and prevent delirium-associated complications [9- 12]. Use of naloxone [5,13-15] as a reversal agent is indicated in opioid overdosing. Evaluation of the utilization of naloxone at the center included inappropriate administration and inappropriate dosing [16,17]. In the presence of hypoactive subtype and patientcontrolled analgesia, delirium can be overlooked or misdiagnosed as respiratory depression when assessment is incomplete [18]. Initially at the cancer center, it was determined from chart review and occurrence reporting that 77% of the inappropriate naloxone use was for altered mental status possibly a hypoactive presentation of delirium. The purpose of this nurse resident simulation was to enhance knowledge and assessment of delirium in a postoperative standardized patient, to provide a venue to identify and to administer naloxone appropriately according to guidelines.
Oncology Nurse Residency Program
To facilitate a smooth transition from novice to competent clinician and to promote adoption of oncology as a specialty practice, an Oncology Nurse Residency Program was developed in February 2013. Goals include providing an environment that prepares newly licensed nurses to function safely and accurately. A formal residency program can enhance critical thinking and clinical decision-making skills [19]. Newly licensed nurses complete a classroom orientation prior to moving to the clinical area to begin unit orientation with their preceptors. The length of time in unit orientation is generally completed in 12 to 16 weeks. For the first twelve months of practice, oncology nurse residents participate in programs outside of their unit for one day each month. In addition to time in the classroom and simulation, the oncology nurse residents meet with their residency group monthly to reflect on collective experiences and challenges. This reflective practice leads to developmental insight and assists in closing the gap between theory and practice.
Simulation
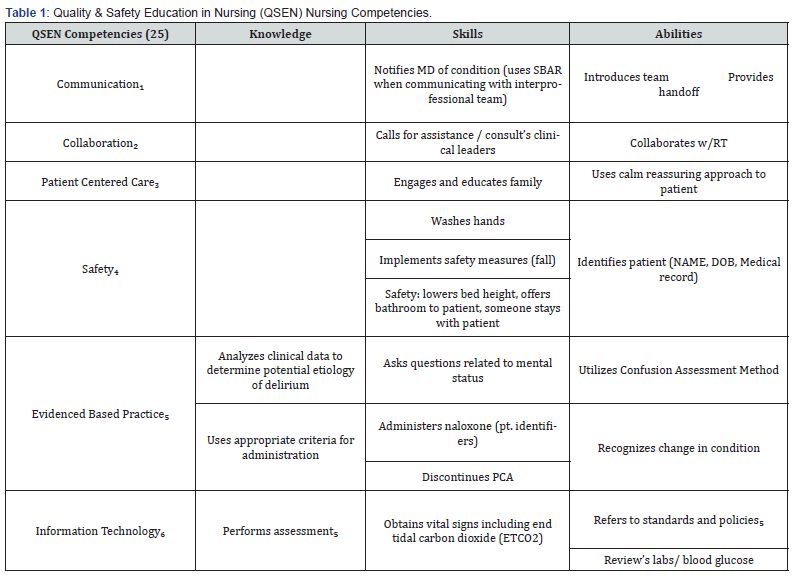
Research validates that learners are more likely to retain content when it is grounded in clinical experiences such as simulation rather than more traditional learning methods. Simulation is a multi-modal type of experiential learning that creates a safe environment for the leaner to practice and enhance critical thinking skills with the goal of improving patient outcomes [20]. Simulation learning has been demonstrated to improve [21] mastery of assessment and standardized patient feedback of scenario [22] A method of simulation can include standardized patients [23] Quality and Safety Education for Nurses (QSEN) [24] identifies key concepts that are included in this simulation such as collaboration, communication, patient centered care, and safety [25]. In the case of naloxone as a reversal agent for the cancer patients, care must be taken to correctly identify opioid toxicity [5,26,27] Nurse residents have an opportunity to calculate dose and administer in a simulated environment non urgent setting [28,29] Naloxone guidelines were developed for administration per hospital policy [30-32].
The use of simulation promotes communication among participants, development of a heightened skill set, and the opportunity for making decisions based in the moment [33,34]. Promotion of critical thinking occurs in this type of environment, as nurses must be able to put theory into practice [35]. Delirium education is enhanced with implementation of assessment and intervention techniques [36]. Utilization of a scripted unfolding case discussion of delirium with debriefing facilitated learning [37] (Table 1).
Geriatric Institutional Assessment Profile
The Geriatric Institutional Assessment Profile (GIAP) is a selfcompleted survey for health care team members [38]. It consists of 133 items and requires approximately 15 minutes to complete. This survey assesses attitudes regarding care of the older adult; knowledge of guidelines for care of the older adult; knowledge of best practice for common geriatric issues (i.e., pressure injuries/ ulcers, medications, sleep, pain, restraints, falls, functional decline, incontinence, dementia, delirium, nutrition, and hydration); and perceived institutional strengths and barriers to best practice for care of older adults [39,40]. Nurses and patient care technicians completed the GIAP as a baseline assessment (response rate 43.3%) requirement for our center in achieving Nurses Improving Care for Healthsystem Elders (NICHE) [41] designation. The NICHE program imbeds evidenced-based practice models in a system targeting geriatric syndromes such as delirium [42,43]. The GIAP was subsequently repeated two years later (response rate 79.1%). These results assisted in targeting priorities for education in our NICHE program [38].

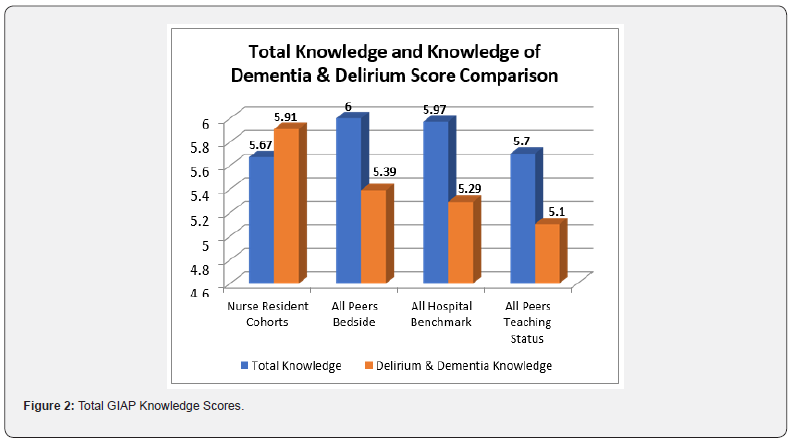
Knowledge domain was only administered to RN participants. RNs were instructed to identify their primary patient care area when completing the GIAP with the exception of the oncology nurse residents who were directed to classify an independent cohort. This provided a separate knowledge comparison with those cohorts who experienced the delirium simulated learning activity. Knowledge of best practices related to mentation includes both delirium and dementia. In the initial GIAP, mean knowledge scores on delirium/dementia (n = 237, 5.1) for registered nurses (RNs) were significantly lower than the mean scores of a benchmarked hospital of similar size and teaching status (n = 4,785, 5.36). A self-study module on delirium in the older cancer patient was subsequently created by the geriatric clinical specialist for all nurses as part of mandatory yearly education. Traditional learning methods such as self-study modules provide content in an asynchronous fashion requiring the learner to review content and complete a post-test to validate learning. Although this is a self-directed strategy it is less effective when not accompanied by another teaching strategy. It has been reported that eighty percent of content in this format is forgotten one day later and eighty percent of remainder fades in one month [44]. The purpose of this project was to compare knowledge scores on delirium in traditional learning groups and scores in a sample enhanced by delirium clinical stimulation. Support and approval were provided by nursing leadership and the department’s Nursing Research & Innovation Council (Figure 1).
Methods
Setting: The project took place at an NCI-designated and Magnet-designated comprehensive cancer center located in the southeastern United States providing inpatient and outpatient care adult oncology care. There are 204 designated inpatient beds with an annual daily census of 160 and 5800 patient days. Twenty-seven ambulatory units provide 250,000 clinic visits yearly. There are approximately 9,500 surgical procedures annually. Forty percent of total discharges are over the age of 65. The project agency achieved NICHE designation in 2014, NICHE exemplar status in 2017.
Sample: This organization piloted the delirium simulation case study in addition to the didactic lecture on a cohort of newly licensed registered nurses as a part of the nurse residency curriculum. This dyad of learning activities was included in the next two cohorts of oncology nurse residents. All three cohorts (n = 44) self-identified in their combined cohorts instead of their home nursing unit during the GIAP reassessment. This allowed for the direct comparison of knowledge acquisition and learning activities in the nurse resident participating in the delirium simulation.
Design
Prior to the simulation the nurse residents participated in passive and active learning strategies. The cost-effective teaching method of lecture aids students in understanding foundational concepts and main ideas [45]. The topic of the first lecture is delirium in older adult oncology patients and includes content on causes, subtypes, screening tools, and pharmacological interventions. The topic of the second lecture is respiratory failure. Nurse residents learn how to interpret arterial blood gases (ABGs) and engage in problem solving through the active learning strategy of case studies. Next, didactic lecture is delivered on opioid toxicities and includes content on end-tidal carbon dioxide (CO2) monitoring, Naloxone administration, safety, and side effects.
Finally, the nurse residents synthesize the knowledge previously obtained through concept mapping. One group is given the concept of delirium and asked to map the pathophysiology, subtypes, sign and symptoms, and treatments. The other two groups are given the concepts of hypercapnic respiratory failure and hypoxic respiratory failure and asked to map the pathophysiology, compensation, signs and symptoms, and treatments. The multimodal content is delivered and facilitated by clinical experts including the Critical Care Clinical Specialist, Geriatric Nurse Practitioner/NICHE Coordinator, and Patient Education Specialist in preparation for the simulation. Standardized Patient Simulation: Post-op delirium and respiratory depression outline displayed in Table 2.

An inter-professional simulated case study utilizing standardized patients was developed. This case study involves a primary nurse, a provider, a respiratory therapist, and a standardized patient, played by a patient advisor. These are patient volunteers trained in patient-and-family centered care with the goal of compassionate care [46]. The delirium simulation enhanced learning scenario was introduced after the geriatric clinical specialist provided a didactic presentation to the oncology nurse residents [47].
Results
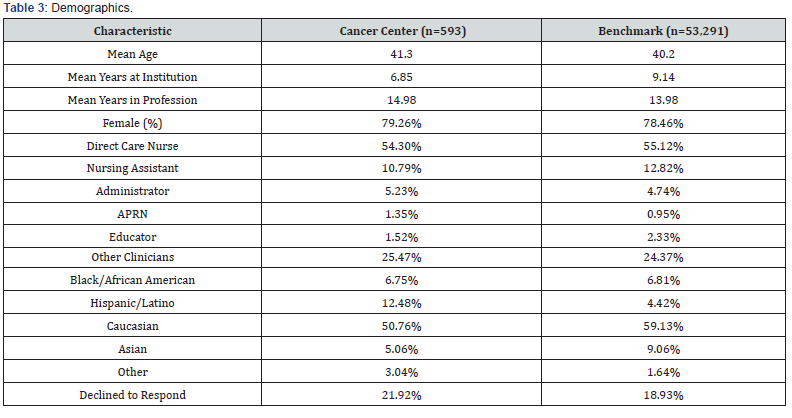
A total of 593 team members completed the survey benchmarked against 53,291 respondents in all hospitals completing the GIAP. This sample represented a 79.1% response rate. Females comprise 79.2 % of those surveyed (Table 3). Direct care team members included 54.3% nurses and 10.79% nursing assistants with an approximate 15 years in the profession and 6.85 years at the study institution. The demographics of the study center respondents were similar to all hospital staff surveyed with the exception of those identified as Hispanic and those who declined to answer. As part of a system quality and safety initiative related to medication safety, the appropriate use of naloxone was increased from 38% to 53% and the appropriate dosing went from 21% to 53%. The GIAP dementia and delirium knowledge score of the oncology nurse residents who participated in simulation (5.91) was statistically significantly higher (p<0.05) that the allpeer bed size, all peer teaching status, and all hospital comparison groups (Figure 2).
Discussion
The primary purpose of this project was to enhance nurse residents’ knowledge and assessment of delirium in a postoperative standardized patient via simulation. Nurse residents within one year of graduation from nursing school may be anticipated to score higher on all knowledge compared to experienced nurses removed from standardized tests. Our findings partially support this. Oncology nurse residents participating in simulation learning scored higher on the GIAP than medical and surgical unit nurses on delirium dementia knowledge. There was not a significant difference in mean total knowledge of medical surgical nurses within the study agency. Evaluating the impact of the intervention resulting in the higher score is demonstrated in the lower overall total knowledge score of the oncology nurse residents in relation to the comparison groups. This leads the educator to believe that the simulation-based learning model improved the delirium scores exclusively and not simply overall intelligence or more recent nursing school graduation [48].
A secondary purpose of this project was to provide a venue for oncology nurse residents to identify a need for and to administer naloxone appropriately according to guidelines. Providing an opportunity to assess indications for, prepare/dilute, calculate dosage, dilute, and administer naloxone in a simulated environment prepares a newly graduated nurse to act safely and confidently in what is often an emergent patient situation [49,50]. In addition to the psychomotor confidence in administration of a high-risk medication, the changing presentation of the patient with delirium in simulation will hopefully translate into selfassurance in recognition and response to clinical deterioration in the unit setting [51,52]. This project is not without limitations. It was performed at one cancer center making it not generalizable to other settings or specialties. Three consecutive cohorts of oncology nurse residents were included and compared to a baseline of GIAP scores of all inpatient oncology nurses including the oncology nurse residents. The GIAP has not been readministered at this time to determine sustainability.
Simulation affords an opportunity to learn and make mistakes without direct patient contact [53]. Using live or computer-based simulated patients presents opportunities for education beyond the traditional classroom setting to augment preceptorship experiences [54]. Using live standardized patients is affordable and can easily be incorporated into hospital and ambulatory care settings for centers without low- or high-fidelity manikins. Conducting needs assessment from nurse residents and preceptors and examining safety occurrences can direct nurse educators in the design of meaningful simulated scenarios with the ultimate goal of improving patient safety.
Conclusion
Knowledge acquisition as reflected by a test score does not always translate into clinical practice. Simulation learning experiences utilize resources of time and labor both for the facilitators and the nursing service. The patient and caregiver outcomes of iatrogenic delirium including falls, restraint use, increased post-acute placement, and increased length of stay can be an impactful metric. Broadening the scope of simulation learning experiences to all direct care team members, while utilizing patient outcome measures, may provide evidencedbased opportunities.
References
- Breitbart W, Alici Y (2008) Agitation and delirium at the end of life: "We couldn't manage him". Jama 300(24): 2898-2910.
- LaFever S, Bory A, Nelson J (2015) Delirium in patients with cancer: what nurses need to know to improve care. Clinical journal of oncology nursing 19(5): 585-590.
- Lawlor PG, Bush SH (2015) Delirium in patients with cancer: assessment, impact, mechanisms and management. Nature reviews Clinical oncology 12(2): 77-92.
- Reston JT, Schoelles KM (2013) In-facility delirium prevention programs as a patient safety strategy: a systematic review. Annals of internal medicine 158(5 Pt 2): 375-380.
- Howlett C, Gonzalez R, Yerram P, Faley B (2016) Use of naloxone for reversal of life-threatening opioid toxicity in cancer-related pain. Journal of oncology pharmacy practice: official publication of the International Society of Oncology Pharmacy Practitioners 22(1): 114-120.
- Witlox J, Eurelings LS, de Jonghe JF, Kalisvaart KJ, Eikelenboom P, et al., (2010) Delirium in elderly patients and the risk of postdischarge mortality, institutionalization, and dementia: a meta-analysis. Jama 304(4): 443-451.
- Leslie DL, Marcantonio ER, Zhang Y, Leo-Summers L, Inouye SK (2008) One-year health care costs associated with delirium in the elderly population. Archives of internal medicine. 168(1): 27-32.
- Leslie DL, Inouye SK (2011) The importance of delirium: economic and societal costs. Journal of the American Geriatrics Society 59 Suppl 2(Suppl 2): S241-3.
- de la Cruz M, Fan J, Yennu S, Tanco K, Shin S, et al., (2015) The frequency of missed delirium in patients referred to palliative care in a comprehensive cancer center. Supportive care in cancer: official journal of the Multinational Association of Supportive Care in Cancer 23(8): 2427-33.
- Rice KL, Bennett M, Gomez M, Theall KP, Knight M, et al., (2011) Nurses' recognition of delirium in the hospitalized older adult. Clinical nurse specialist CNS 25(6): 299-311.
- Steis MR, Fick DM (2008) Are nurses recognizing delirium? A systematic review. Journal of gerontological nursing 34(9): 40-48.
- Edelstein A, Alici Y (2017) Diagnosing and Managing Delirium in Cancer Patients. Oncology (Williston Park, NY) 31(9): 686-692.
- Connors NJ, Nelson LS (2016) The Evolution of Recommended Naloxone Dosing for Opioid Overdose by Medical Specialty. Journal of medical toxicology: official journal of the American College of Medical Toxicology 12(3): 276-281.
- Dahan A, Aarts L, Smith TW (2010) Incidence, Reversal, and Prevention of Opioid-induced Respiratory Depression. Anesthesiology 112(1): 226-238.
- Gordon DB, Pellino TA (2005) Incidence and characteristics of naloxone use in postoperative pain management: a critical examination of naloxone uses as a potential quality measure. Pain management nursing: official journal of the American Society of Pain Management Nurses 6(1): 30-36.
- Neil K, Marcil A, Kosar L, Dumont Z, Ruda L, et al., (2013) Retrospective analysis of opioid medication incidents requiring administration of naloxone. Can J Hosp Pharm 66(5): 280-288.
- Palfrey J, Mandel M, Caulkin R (2020) Inappropriate use of naloxone in a hospital setting compromising patient safety: a quality improvement project. Future Healthc J 7(Suppl 1): s62.
- Fong TG, Tulebaev SR, Inouye SK (2009) Delirium in elderly adults: diagnosis, prevention and treatment. Nature reviews Neurology 5(4): 210-220.
- Scoville R LK (2014) Comparing Lean and Quality Improvement. Cambridge, Massachusetts: Institute for Healthcare Improvement.
- Bliss M, Aitken LM (2018) Does simulation enhance nurses' ability to assess deteriorating patients? Nurse education in practice 28: 20-26.
- Kirkman MA, Sevdalis N, Arora S, Baker P, Vincent C, et al., (2015) The outcomes of recent patient safety education interventions for trainee physicians and medical students: a systematic review. BMJ Open 5(5): e007705.
- Safety AfHQa (2018) Health Care Simulation to Advance Safety. Rockville, MD.: Agency for Healthcare Quality and Safety.
- Dickter DN, Stielstra S, Lineberry M (2015) Interrater Reliability of Standardized Actors Versus Nonactors in a Simulation Based Assessment of Interprofessional Collaboration. Simulation in healthcare: journal of the Society for Simulation in Healthcare 10(4) :249-255.
- Cronenwett L, Sherwood G, Barnsteiner J, Disch J, et al., (2007) Quality and Safety Education for Nurses. Nursing outlook 55(3): 122-131.
- Jarzemsky P, McCarthy J, Ellis N (2010) Incorporating quality and safety education for nurses’ competencies in simulation scenario design. Nurse educator 35(2): 90-92.
- Smith LH (2007) Opioid safety: is your patient at risk for respiratory depression? Clinical journal of oncology nursing 11(2): 293-296.
- Services CfMaM (2014) Requirements for hospital medication administration, particularly intravenous (IV) medications and post-operative care of patients receiving IV opioids. Baltimore, MD: CMS.
- Torrie J, Cumin D, Sheridan J, Merry AF (2016) Fake and expired medications in simulation-based education: an underappreciated risk to patient safety. BMJ quality & safety 25(12): 917-920.
- Raemer D, Hannenberg A, Mullen A (2018) Simulation Safety First: An Imperative. Simulation in healthcare: journal of the Society for Simulation in Healthcare 13(6): 373-375.
- Jungquist CR, Pasero C, Tripoli NM, Gorodetsky R, Metersky M, et al., (2014) Instituting best practice for monitoring for opioid-induced advancing sedation in hospitalized patients. Worldviews on evidence-based nursing 11(6): 350-360.
- Jungquist CR, Smith K, Nicely KL, Polomano RC (2017) Monitoring Hospitalized Adult Patients for Opioid-Induced Sedation and Respiratory Depression. The American journal of nursing 117(3 Suppl 1): S27-s35.
- Meisel M, Meisel S (2007) Best-practice protocols: reducing harm from high-alert medications. Nursing management 38(7): 31-39.
- Ford DG, Seybert AL, Smithburger PL, Kobulinsky LR, Samosky JT, et al., (2010) Impact of simulation-based learning on medication error rates in critically ill patients. Intensive care medicine 36(9): 1526-1531.
- Crowe S, Ewart L, Derman S (2018) The impact of simulation-based education on nursing confidence, knowledge and patient outcomes on general medicine units. Nurse education in practice 29: 70-75.
- Kuhrik NS, Kuhrik M, Rimkus CF, Tecu NJ, Woodhouse JA (2008) Using human simulation in the oncology clinical practice setting. Journal of continuing education in nursing 39(8): 345-355.
- Grealish L, Todd JA, Krug M, Teodorczuk A (2019) Education for delirium prevention: Knowing, meaning and doing. Nurse education in practice 40: 102622.
- Page JB, Kowlowitz V, Alden KR (2010) Development of a scripted unfolding case study focusing on delirium in older adults. Journal of continuing education in nursing 41(5): 225-230.
- Tavares JP, da Silva AL (2013) Use of the Geriatric Institutional Assessment Profile: an integrative review. Research in gerontological nursing 6(3): 209-220.
- Boltz M, Capezuti E, Kim H, Fairchild S, Secic M (2009) Test--retest reliability of the Geriatric Institutional Assessment Profile. Clinical nursing research 18(3): 242-252.
- Boltz M, Capezuti E, Kim H, Fairchild S, Secic M (2010) Factor structure of the geriatric institutional assessment profile's professional issues scales. Research in gerontological nursing 3(2): 126-134.
- Boltz M, Harrington C, Kluger M (2005) Nurses Improving Care for Health System Elders (NICHE). The American journal of nursing 105(5): 101-112.
- Mezey M, Kobayashi M, Grossman S, Firpo A, Fulmer T, et al., (2004) Nurses Improving Care to Health System Elders (NICHE): implementation of best practice models. The Journal of nursing administration 34(10): 451-457.
- Fulmer T, Mezey M, Bottrell M, Abraham I, Sazant J, et al., (2002) Nurses Improving Care for Healthsystem Elders (NICHE): using outcomes and benchmarks for evidenced-based practice. Geriatric nursing (New York, NY) 23(3): 121-127.
- Bradshaw ML AJ (2011) Innovative teaching strategies in nursing and health professions 5th Boston, MA: Jones& Bartlett.
- Bastable SB (2019) Nurse as education: Principles of teaching and learning for nursing practice. 5th ed. Sudbury, MA: Jones & Bartlett.
- Cohen BS, Boni R (2018) Holistic Nursing Simulation: A Concept Analysis. Journal of holistic nursing: official journal of the American Holistic Nurses' Association 36(1): 68-78.
- Davis KD, Nye C (2017) Care of the Older Adult with Postoperative Delirium: An Interprofessional Simulation for Undergraduate Nursing Students. Nursing education perspectives 38(2): 103-115.
- Buykx P, Cooper S, Kinsman L, Endacott R, Scholes J, et al., (2012) Patient deterioration simulation experiences: impact on teaching and learning. Collegian (Royal College of Nursing, Australia) 19(3): 125-129.
- Stirling K, Smith G, Hogg G (2012) The benefits of a ward simulation exercise as a learning experience. British journal of nursing (Mark Allen Publishing) 21(2): 116-118.
- Ashley J, Stamp K (2014) Learning to think like a nurse: the development of clinical judgment in nursing students. The Journal of nursing education 53(9): 519-525.
- Hogg G, Miller D (2016) The effects of an enhanced simulation programme on medical students' confidence responding to clinical deterioration. BMC medical education 161 (16): 8.
- Wayne DB, Didwania A, Feinglass J, Fudala MJ, Barsuk JH, et al., (2008) Simulation-based education improves quality of care during cardiac arrest team responses at an academic teaching hospital: a case-control study. Chest 133(1): 56-61.
- Aebersold M, Titler MG (2014) A simulation model for improving learner and health outcomes. The Nursing clinics of North America 49(3): 431-439.
- Aebersold M (2018) Simulation-based learning: No longer a novelty in undergraduate education. Online Journal of Issues in Nursing 23(2).






























