Exploring the role of health care providers in referring to community based informal psychosocial support centres for cancer patients and their relatives
Adriaan Visser*
*Director and researcher at PRO-health.org, Rotterdam, The Netherlands
Submission: October 02, 2020; Published: October 23 , 2020
*Corresponding author: Dr. Adriaan Visser, PRO-health.org; Abraham Kuyperlaan 91A, 3038 PG, Rotterdam, The Netherlands
How to cite this article: Adriaan V. Exploring the role of health care providers in referring to community based informal psychosocial support centres for cancer patients and their relatives. JOJ Nurse Health Care. 2020; 11(5): 555822. DOI:10.19080/JOJNHC.2020.11.555822.
Abstract
The psychosocial support for cancer patients in the mental health care is often limited and/or expensive for patients. In the Netherlands is there for the informal regional support developed Community Based Psychosocial Support Centres for Cancer patients and relatives (CBPSC), offering easily accessible and financially not charged support. Patients can participate in supporting complementary activities and/or further professional psychological help. We studied the number of visits by cancer patients and the amount of references by health care professionals to CBPSCs.
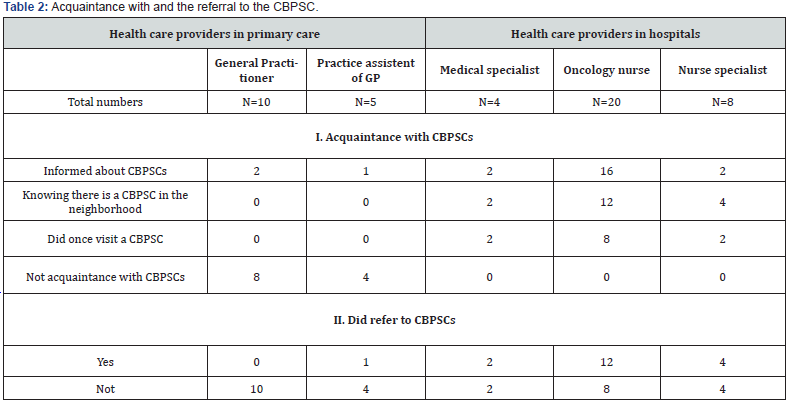
Visitors filled-out a web-based questionnaire (study I), covering 701 cases from 25 CBPSCs with questions about how they contacted CBPSCs and who did refer them to the CBPSCs. The second study (II) aimed at ten GPs, five professional practice assistants of GPs, four medical specialist, twenty oncology nurses, and eight nurse specialists from the extended region of Rotterdam, the Netherlands. They filled out a questionnaire and/or were interviewed by trained students about their knowledge and referral of cancer patients to CBSPCs.
Most patients in study I did not know what CBPSCs are and where to find it. A quarter was alerted by family, friends, and acquaintances, or informed about CBPSCs by hospital oncology nurses and by leaflets. References by GPs and medical specialists were hardly mentioned. The second study (II) shows that oncology nurses play the most important role in the reference of patients to CBPSCs. GPs and their practice assistances are often not informed about CBPSCs, but health care providers in hospitals were much better informed about CBPSCs, referring about half of the patients to CBPSCs.
The study confirms the value of this type of informal support. CBPSCs need to improve their position in the health care by more public campaigns and education of patients as well as health care providers. More countries should introduce this type of easily accessible cheap, effective, and highly valued supportive care with the aid of public funds in cooperation with hospitals.
Keywords: Cancer; Community-based support centres in cancer; The Netherlands; Evaluation; Mental health care; Psychosocial support; Health care providers
Introduction
Countries are since decades confronted with a growing number of people with cancer due to a higher life expectancy and aging populations [1]. In 2017 there were 347.121 (prevalence) Dutch people with cancer [2]. The diagnosis cancer and its treatment interfere with life in practical, physical, emotional, social, and philosophical terms, which stresses the importance of psychosocial care and aftercare for cancer patients [3-5].
Offer of supportive care
Cancer patients and their relatives may receive support in hospitals from e.g. oncologists and oncology nurses, however, they are often limited accessible by overload of their work. The secondary care offers support by e.g. GPs, social workers, psychologist, and psychiatrists. Due to waiting lists and the financial requirements these forms of supportive care are often not easily accessible for cancer patients. Therefore, patient organisations and health care providers in several countries took the initiative to found patient-oriented support centres. Examples of these institutes are the Maggie’ centres in the UK, Barcelona and Hongkong; in the USA the MD Anderson Cancer Centre (Houston) and the Memorial Sloan Kettering Cancer Center (New York) offer support groups; in Germany psychological support is offered by the Lebenswert Institute (Koeln) and the Bayerische Krebsgesellschaft (München). Comparable initiatives exist in Australia, Belgium, Canada, Denmark, Norway, and Israel [6,7]. The Netherlands took the initiative to found CBPSCs: Community based psychosocial support centres for cancer patients [8].
Community based psychosocial support centres for cancer patients
The CBPSCs are private initiatives, and are independent social initiatives funded from several sources: local and country policy, sponsorship, grants, donations, and activities organized by themselves. Nowadays more than 40.000 cancer patients visit the CBPSCs {note 1} These institutes are mostly led by a part time and paid professional director/coordinator, beside the support of specialized trained volunteers. The support that CBSC’s offer to their visitors can be participation in ‘social activities’ and in less cases also receiving ‘therapeutic psychosocial support’ [8].
Social activities are low-threshold psychosocial support facilities, offering contacts with fellow patients who have (had) cancer and dealing with their illness, treatment, and care. It may include personal meetings with fellow patients (e.g. mornings to have a cup of coffee together), discussion groups; informal talks, creative expression (painting, photography) and bodymind activities for relaxation (meditation, singing). Therapeutic support includes therapies given by in principle professionals inor outside the CBSCs, but in close collaboration with the CBPSCs: cognitive behaviour therapy (CBT), yoga, and forms of individual therapy.
The offer by CBPSCs should in fact fit within the whole of the psychosocial oncology care, as the lowest level of support in a stepped-care model [8]. This may lead to a more convenient offer of informal care and support to the patients, close to their homes [9]. This requires a fitting communication with the health care and an adequate reference of patients. Lacking information about these conditions was the impetus for two studies.
Aims of the studies
At the start of the development and founding of CBPSCs, there was not much information available about how and by whom cancer patients will/need to be informed about CBPSC’s. The CBPSCs are not a part of the official and formal health care organisations, like the mental healthcare institutions and the professional Dutch psychosocial oncology institutes. They did often not recognize the CBPSCs as professional organisations to help cancer patients. We will describe the use and the reference process to CBPSCs from the view of cancer patients as well from health care providers. In study I we analysed how and by whom cancer patients are informed about CBPSCs. In study II we answer the questions what several health care providers know about CBPSCs and if they refer cancer patients to CBPSCs.
Material and methods
Visits of cancer patients to CBPSCs (part I) In this part I we studied the CBPSCs services of 25 CBSCs by filling-out a web-based questionnaire. To include approximately half of the 60 available and willing to participate CBSPCs; 30 centres were included in this study, based on the visitors from eight years ago. Five CBPSCs could not participate due to practical reasons. Patients were invited by email, post, and flyers. In total of 3,134 invitations were sent off: 2,436 by e-mail and 698 by regular mail. In totally 701 visitors of 790 participants decided to participate in this part of the study (non-response 11%). The questions, approved by members of the advisory board and the scientific committee of the Dutch Cancer Society, are about the information patients received about CBPSCs, who did they contacted about visiting a CBPSC and by which health care professional they were referred. The validity of these question was proved in former studies [8,10,11].
Study among health care providers (part II)
We questioned cancer health care providers in surveys and interviews: general practitioners, professional assistants of GPs , medical specialist in hospitals, oncology nurses, nurse specialists {note 2}, and health care practitioners. They were recruited in the greater area of Rotterdam, the Netherlands. Only a few of them did not response or could not be reached (one hospital, three general practitioners) due to practical causes. The final sample did contain ten GPs, five professional assistants of GPs, 2 four medical specialists, twenty oncology nurses, and eight nurse specialists. They filled in a questionnaire, often completed by interviews about their knowledge of CBPSPs, their tasks, and the referral of patients to CBPSPCs [9].
Statistical analysis
We used frequencies, means, crosstabs, construction of sum scores for scales, correlations, and Anova’s to analyze the data, applying SPSS.
Ethical approval
To guarantee ethical procedures both the members of the advisory board and the scientific committee of the Dutch Cancer Society approved our research protocol.
Results
The visits to CBPSCs
Most referred cancer patients to a CBPSC did not know what a CBPSC is and where not informed how to find a CBPSC in their region. Table 1 shows how patients contacted a CBPSC (Table 1). The largest group of visitors did answer that they were alerted by family, friends and acquaintances (22%). Further, information from hospital oncology nurses (21%) and by written information (21%) did educate them about the existence of a CBPSC. References by two type of health care professionals from primary and secondary health care were hardly mentioned: medical specialists (6%) and general practitioners (5%).

The role of health care providers
In Table 2 we give an overview of the role of health care providers in primary care and hospitals concerning their acquaintance with and the referral to CBPSCs (Table 2).The results show that GPs and their practice assistants are mainly not informed about CBPSCs in their area. The health care providers in hospitals are better informed about CBPSCs and refer in about half of the cases in this study to a CBPSC. Especially oncology nurses play the most important role in the reference of cancer patients to CBPSCs.
Discussion
Cancer patients are frequently struggling to find fitting psychosocial oncological care, within the often instrumental and not psycho-social oriented medical care [12,13]. The Dutch psychosocial cancer care did solve this problem by the founding of communitys support centres for cancer patients (CBPSCs). We explored in quantitative exploring studies how cancer patients encountered CBPSCs and how the reference pattern in the health care is functioning. Study I show that the main number of the visitors are mostly not referred by the health care, but by own informal contacts of the patients, because CBPSCs are rather unknow. The patients participate in a lot supportive social activities and used therapeutical activities with a broad range of therapies. Study II shows that oncology nurses play the most important role in the reference of patients to CBPSCs, but GPs and their practice assistants are not so much informed about CBPSs in their area.
This is the first extensive study on CBPSCs in the Netherlands. It confirms the results of earlier smaller studies [10]. The number of participants was lower than expected, because we intend to include the number of visitors, while the CBPSCs often count the number of visits. The sample is possible biased by the participation of a high number of women with breast cancer and a low number of men with prostate cancer, as compared to national statistics [2]. The limitations of the cross-sectional survey method in part I is compensated by study II on the factual reported supplied care by oncological providers. The reference to CBPSCs is rather limited in the health care, especial references by medical doctors and GPs. Other and recent studies show that this situation is not much improved [14, 15]. An effective PR on CBPSCs should be especially concentrated on hospitals and the primary care. In the meantime, the number of Dutch CBPSCs is raising, but the finance is still limited.
The study implies also lessons for other countries, because only a few other countries did fund and implement comparable organizations like CBPSCs. There is a growing tendency to found comparable support centers in other countries [6,7]. The organization of the health care and the position of CBPSCs differ between countries. In the Netherlands, the CBPSCs are independently functioning from hospitals. In a few European countries and the USA, UK, Canada, and Australia, is that not the case [6,7]. Therefor they may refer more cancer patients to the affiliated hospitals. Further comparative international studies are necessary on the reference, use, and effect of several types of CBPSCs.
Words of thanks
The Dutch Cancer Foundation KWF did provide a grant for these studies. We thank the participants in the studies and the involved staff member of the CBPSCs Also thanks to my former colleagues Dr. Anne Loes van Staa (lecturer Dr. Heleen van der Stege en Monique Vahedi Nikbakht-van de Sande MSc (MVH), parttime researchers at the Rotterdam Applied University, Centre of Expertise for Innovations in Care, Rotterdam, the Netherlands; Rosella den Hollander and Anne van den Brom (RHAB) studied Policy and Management in de Health Care, Erasmus University Rotterdam, the Netherlands. for their appreciated contributions to the execution and reporting of the study about Community Based Psychosocial Support Centers for Cancer Patients and relatives (CBPSCs) in the Netherlands.
Notes
From here on we only mention patients but includes too relatives.
i. In the Dutch health care work practice professionally trained nurses to support the
ii. GP with somatic and mental problems of patients, and to refer them.
References
- Siegel RL, KD Miller, A Jemal (2020) Cancer statistics 2020. CA: A Cancer Journal for Clinicians 70(1): 7-30.
- Integraal Kankercentrum Nederland (IKNL), 2017. Detecteren behoefte Psychosociale zorg. Landelijke richtlijn, versie 2.0. (Dutch: Integral Cancer Center the Netherlands (IKNL). (Dutch; Detection of need psychosocial care. National Directive, version 2.0].
- Holland JC (1998) Psycho-oncology. Oxford University Press, New York, USA.
- De Haes H, Gualtherie van Wezel L, Sanderman R (2017) Psychologische patiëntenzorg in de oncologie (Dutch; Psychological patiënt care in oncology). Gorcum BV, Assen, the Netherlands.
- Kreitler S (2019) Psycho-oncology for the clinician: The patient behind the disease. Springer, Cham, Switzerland.
- Visser A, Wildenbeest M, Nieuwenhuizen L (2012) Evaluation of psychosocial support for people with cancer. Med. Encount 26(2): 19-21.
- Brom A van den, R den Hollander, AP Visser (2014). Onderzoek naar Inloophuizen in het buitenland voor mensen met kanker en hun naasten (Dutch; Walking-in homes in foreign countries for people and their relatives). Psychosoc. Oncol 23(4): 26-27.
- Visser A (2020) Community based psychosocial support centres for cancer patients: use, evaluation and effect. Report. Concept manuscript, in press.
- VWS, Ministry of Health, Welfare and Sport Netherlands, Psychosociale zorg bij somatische problematiek. Werkgroepkostenenbekostiging. [Dutch; Psychosocial care in somatic problems. Working group costs and funding]. [Adviesrapport].
- Visser A, Geluk W, Breed W, Leeuwen N van, Liempt H van, et al., (2009) De betekenis van inloophuizen voor mensen met kanker en hun naasten: ontstaan, gebruik, behoefte en waardering (Dutch; The meaning of walking-in homes for people with cancer and their relatives). Tijdschr. Oncol 6:248-255.
- Visser AP (2018) Influence of visiting walking-in homes for cancer patients on their well-being. Hogeschool Rotterdam, Kenniscentrum Zorginnovatie Rotterdam, the Netherlands.
- Skirbekk H, Korsvold L,Finset A (2018) To support and to be supported: A qualitive study of peer support centers in cancer in Norway. Patient Educ Couns 101(4): 711-716.
- Harrison JD, Slomon MJ, Young JM, Price PN, Buttow MJ (2009) What are the unmet supportive care needs of people with cancer? A systematic review. Support Cancer Care17(8): 1117-1128.
- IPSO, Sinzer (2018) Effectonderzoek: De maatschappelijke waarde IPSO-inloophuizen (Dutch; Effect study: the social value of walking-in homes), IPSO, Almere, the Netherlands.
- Ouden J den, Stoopman T Verhagen (2014) De waarde van inloophuizen (Dutch; The value of walking-in homes). RSM, Erasmus University, Rotterdam, the Netherlands.






























