The Relation between Coping Strategies and Social Support among Patients with Schizophrenia
Eweida RS* and Maximos MH
Department of Psychiatric Nursing and Mental Health, Alexandria University, Egypt
Submission: November 02, 2017; Published: December 08, 2017
*Corresponding author: Eweida RS, Department of Psychiatric Nursing and Mental Health, Alexandria University, Egypt, Email: dr_rashapchsych@hotmail.com
How to cite this article: Eweida RS, Maximos MH, Sharaf AYH. The Relation between Coping Strategies and Social Support among Patients with Schizophrenia. JOJ Nurse Health Care. 2017; 5(4): 555669. DOI: 10.19080/JOJNHC.2017.05.555669
Abstract
Background: Schizophrenic patients have often been found to differ from healthy controls in how they react to and cope with stressful life events that occur in their daily lives. Perceived social support appears to directly decrease the use of these harmful coping strategies and to provide a basis for positive thinking and cognitive restructuring. So, schizophrenic patients need to mobilize their social support system to cope effectively with stressful life events and daily hassles.
Objective: This study aimed to identify the relation between coping strategies and social support among patients with schizophrenia.
Method: This study follows a descriptive correlational design. Subjects of the study comprised convenience sample of 150 schizophrenic outpatients of both sexes, who attended the psychiatric outpatient clinics of two hospitals in Alexandria namely EL-- Maamoura Hospital for Psychiatric Medicine and Ras--EL Teen General Hospital.
Results: The studied schizophrenic patients that used avoidance--oriented coping obtained the highest mean score of coping (48.07±10.20), while those using task-oriented coping obtained the lowest mean score (36.60±16.73).0nly half of the studied schizophrenic patients received social support with a total mean of 41.15±4.89.
Conclusion: The studied schizophrenic patients relied on avoidance and emotional--oriented coping more frequently than task-- oriented coping to negotiate their stressful life events. Social support was proved to be the independent predictor of the task-oriented coping strategy.
Keywords: Coping strategies; Social support; Schizophrenia
Introduction
Schizophrenia is a debilitating long term disorder characterized by episodes of acute psychotic symptoms and periods of remission often accompanied by alteration in social and psychological functioning [1-3]. It has been proposed that patients with schizophrenia often have stress-- prone life styles that generate surplus life events as a result of factors such as limited social support networks, coping abilities, and unemployment. In addition, people with schizophrenia often experience distressing mental symptoms such as hearing internal voices not heard by others, or believing that other people are reading their minds, controlling their thoughts, or plotting to harm them [3,4]. Research suggested that stressful life events that are psychosocial in nature, appear to play a major role in triggering schizophrenic episodes, increasing the likelihood of relapse rate, chronicity and prolong the duration of hospitalization of patients with schizophrenia [5-7].
Since the course of illness is considered a major source of stress in schizophrenia it raises the need for coping [8]. According to the cognitive--transactional theory of stress, coping has been defined as "a constantly changing one's cognitive and behavioral effort to manage the internal and external demands of a person-environment transaction that is considered taxing or exceeding one’s resources" [9]. Coping strategies are categorized into three main styles namely task, emotion, and avoidance-oriented [10].
Social support is known to be the greatest and most powerful force that facilitates successful coping, increases adherence to medical treatments, and improves recovery from illness [11]. The results of research into the social support networks for patients suffering from schizophrenia revealed that patients with schizophrenia, especially those who are chronically ill, have much worse social support networks in terms of quantity and quality [12]. Additionally, patients with schizophrenia find it particularly difficult to find emotional support. They feel that the support given to them in social rehabilitation systems is mostly formal in character. It has indicated that 60% of patients with schizophrenia reported the need for more emotional support, advice and trust- based relationships [13].
Coping styles among patients with schizophrenia is a critical problem in psychiatric nursing practice [14]. There appears to be widespread that the inability to manage and respond to stress is believed to be among the primary causes of relapse and reduced quality of life [15]. Moreover, disturbances in coping patterns and social support affect social functioning of patients with schizophrenia [16]. This link leads to an increased concern on studying the effect of social support on the enhancement of coping and assisting patients with schizophrenia to remain well in the community [17]. Accordingly there is a need for research that examines whether social support can contribute to a positive effect on the coping strategies with stress among schizophrenic patients seeking care on outpatient s level. Such knowledge can enable nurses to use strategies that help in improving the patient's coping styles and provide a kind of support necessary to integrate schizophrenic patients into the community.
The aim of the work
Identify the relation between coping strategies and social support among patients with schizophrenia.
Materials and Methods Design of the Study and Setting
The study follows a descriptive correlational design. It was conducted in the psychiatric outpatient clinics of two hospitals in Alexandria namely EL-- Maamoura Hospital for Psychiatric Medicine and Ras--EL Teen General Hospital. Both are affiliated to the Ministry of Health.
Subjects of the study comprised a convenience sample of 150 schizophrenic outpatients of both sexes, who attended the previously mentioned settings (75 from each), fulfilling the following criteria: Definite diagnosis of schizophrenia with no comorbidity, intellectual disabilities, organic brain disease, drug/ alcohol abuse or other psychiatric mental disorders, attending the outpatient clinics for follow up and being able to communicate in a coherent and relevant manner.
Tools of the Study
The data for this study were obtained using the following tools
Tool I: The Coping Inventory of Stressful Situations (CISS) scale, which was developed by Endler & Parker [18]. The CISS comprises 48- - self- -report items, measuring multidimensional coping styles used when individuals are faced with stressful, difficult or upsetting situations. The scale comprises three subscales, 16-- item in each subscale, that empirically assesses three basic dimensions of coping namely; task-oriented, emotion- oriented, and avoidance- -oriented coping style. Respondents were asked to answer the questions on a five point Likert--type scale ranging from (1) "Not at all" to (5) "Very much" [18]. For all of these subscales, a mean score will be calculated. The higher the score, the greater the levels of the measured construct.
Tool II: The Social Support Network Inventory (SSNI) is a 10- self-- report items which was developed by Flaherty & Gaviria [19] to measure the perceived social support. The scale comprises five dimensions that yield information on availability (items 1, 2), reciprocity (items 5, 7), emotional support (items 3, 6, 8, and 9), practical support (item 4) and event support (item 10). Each item is rated on a five point Likert--type scale ranging from 1 to 5, with higher score indicating greater level of social support [19].
In addition, a socio--demographic and clinical data tool was constructed by the researcher to elicit information about the patients' age, educational level, duration of illness, and number of hospitalizations etc.
Statistical Analysis
Data were coded, computerized and then analyzed using the Statistical Package for Social Sciences (SPSS) software package version 16.0. Descriptive statistics like number, percentage, minimum, maximum, means and standard deviations (SD) were used to describe and summarize data. An index of Socio-economic level was calculated using three variables namely: level of education, income and crowding index. It was divided into three levels according to the interquartiles range of the study subjects.
Results
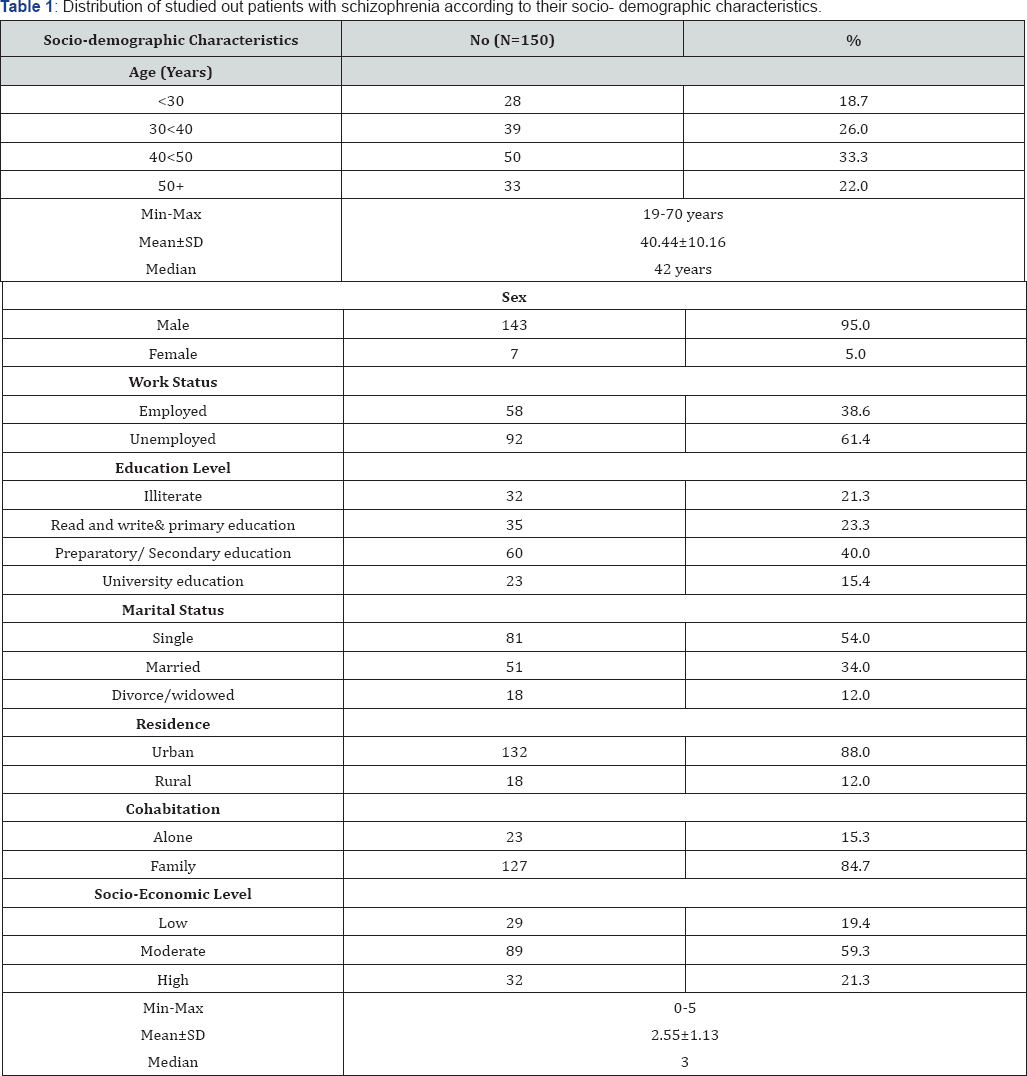
Table 1 shows the distribution of the studied outpatients with schizophrenia according to their socio-- demographic characteristics. It appears from this table that patients' age ranged between 19 and 70 years, with a total mean age of 40.44±10.16 years. In relation to sex, the majority of the studied sample (95.0%) was males. Unemployed patients represented 61.4% of the total sample. More than one third of the sample (40.0%) had preparatory or secondary education, while only 15.4% of patients had a university education.
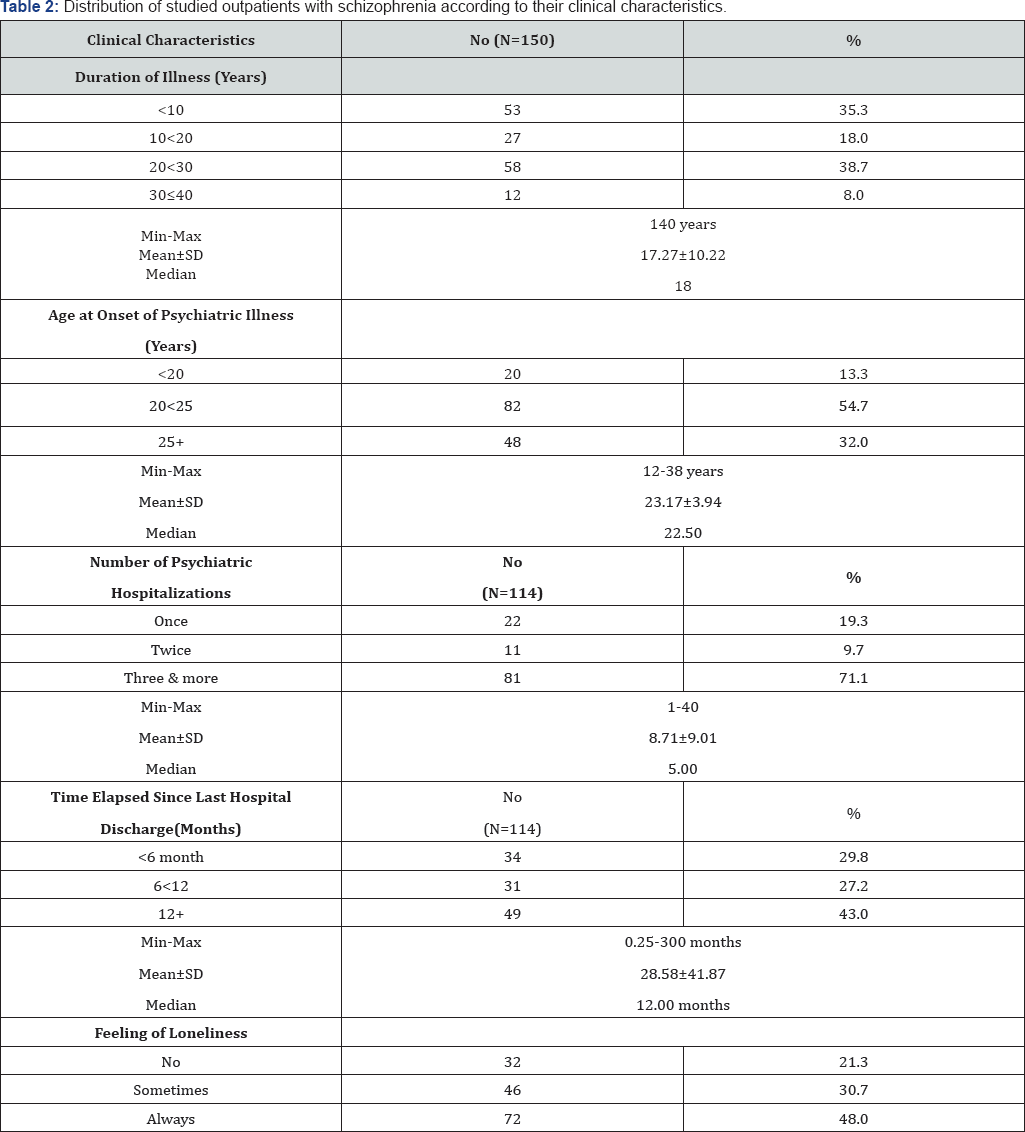
Table 2 presents the distribution of the studied outpatients with schizophrenia according to their clinical characteristics. It was found that the duration of illness ranged from 1 to 40 years with a total mean of 17.27±10.22 years. More than half of the patients (54.7%) had an onset of illness at an age ranging from 20 to less than 25 years, followed by those who had an onset of illness at an age starting from 25 years and more (32%). Nearly three quarters of the patients (71.1%) were admitted three times and more, with a median of 5.00 times. Forty-- three percent of the studied patients were discharged since one year and more with a median of 12.00 months. Nearly half of the schizophrenic patients (48.0%) were suffering from always feeling lonely, while only 21.3% of them were not.
Figure 1 presents the means and standard deviations of coping strategies used by outpatients with schizophrenia. It was observed that avoidance--oriented coping obtained the highest mean score of coping (48.07±10.20), while task--oriented coping obtained the lowest mean score of coping (36.60±16.73).
Figure 2 presents the distribution of outpatients with schizophrenia according to their perceived sense of social support. Fifty percent of the studied outpatients with schizophrenia reported having source(s) of social support in their life. The total mean score of perceived sense of social support was 41.15±4.89.
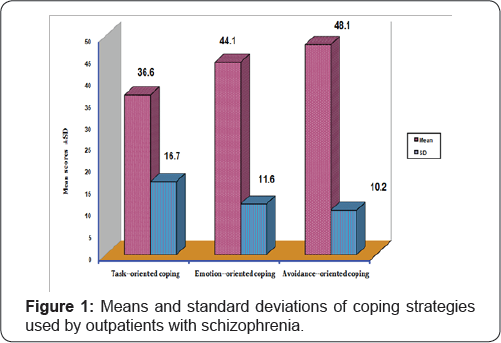
Table 3 shows the correlation between the total score of social support and coping strategies of outpatients with schizophrenia. It appears from this table that social support was highly significantly correlated with task- oriented coping (r=0.51, p=0.000). This means that the more social support is available, the higher the degree of using task-oriented coping strategy.
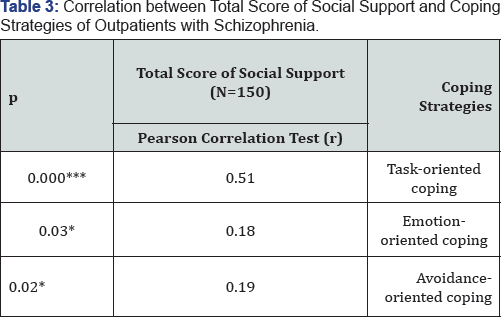
*P<0.05; **P<0.001; ***P=0.0001
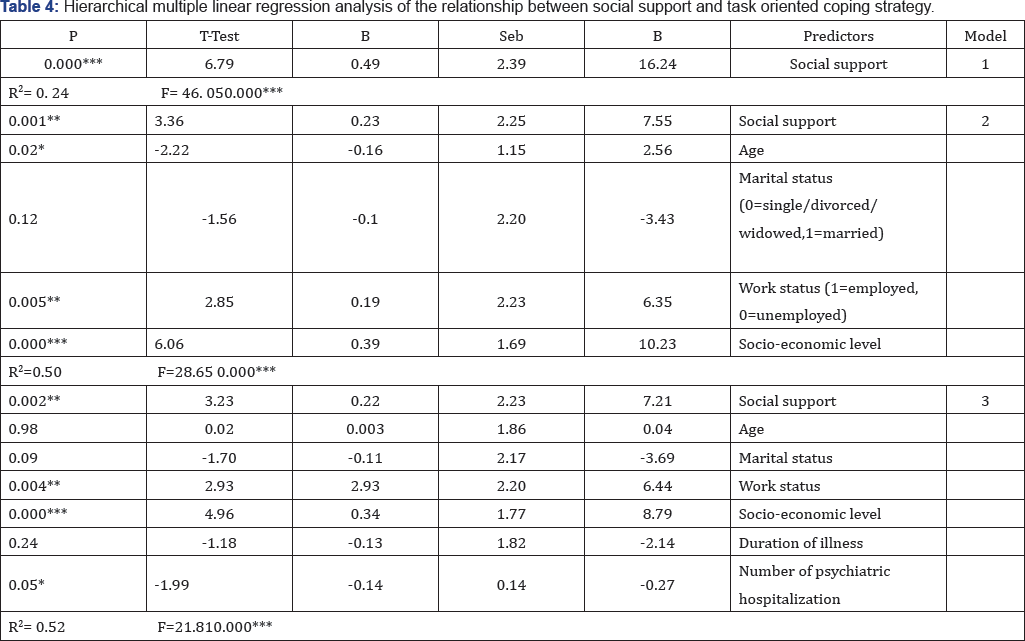
Table 4 summarizes results of three regression models used to examine the independent association of social support with task- oriented coping strategy when the effects of other covariates were accounted for. Model 1 indicates that social support was positively associated with task-- oriented coping strategy (B=16.24, p=0.49, t=6.79, P=0.000). Results of Model 2 and 3 reflect that the relationship between social support and task-- oriented coping strategy remained positively significant even after controlling the covariates (socio--demographic variables in model 2 and clinical variables in model 3). The increment in R2 was significant, across the three models, explaining 52% of the variance in task-oriented coping strategy, Fchange (7,142)=21.81, P=0.000. Conclusively,these models proved that social support has independent influence on task--oriented coping strategy.
Discussion
Based on the study results, it can be concluded that the studied schizophrenic patients relied on avoidance and emotional--oriented coping more frequently than task-- oriented coping to negotiate their stressful life events. This is especially true knowing that nearly half of the schizophrenic patients in the present study (46.7%) had a duration of illness ranging from 20 to less than or equal to 40 years, which reflects a prevalent high degree of chronicity among the studied sample. Negative symptoms, which are the prominent feature of chronicity of patients with schizophrenia, may influence how patients develop coping strategies to manage their life problems. In this respect, negative symptoms, that involve emotional withdrawal, affective blunting, and avolition, can limit patient's motivation to take action, when faced with stressors in daily life, and thereby a higher preference for ignoring or putting problems out of mind is ensued. In addition, Rollins et al. [20] speculated that patients with negative symptoms might not have the abstraction capability to perform a successful and accurate cognitive appraisal of the threat to their well--being, a factor that undermines the patient's ability to muster cognitive resources for dealing with stress.
Again, the chronicity and long term of the schizophrenic illness, manifested by a great sector of the studied patients, indicate that the disease occurs early in life. This might erode one's ability to employ effective coping strategies. Kao & Liu [21] documented that the early age of onset of psychiatric illness is usually accompanied by deteriorating effects that might fall in the domains of attention, perceptual, and executive functions of the adolescent and adult schizophrenic. These cognitive deficits might interfere with the patient’s ability to develop and access effective, flexible and adaptive coping strategies with stress. Wilder--Willis et al. [22] found that schizophrenic patients with more severe executive and verbal memory deficits are less likely to report using constructive coping mechanisms. Furthermore, they documented that problem solving skills, planning, abstract thinking and the ability to access stored knowledge and strategies, are necessary cognitive prerequisites for engaging in activities that help individuals to redefine their lives and cope with the stressors of having a mental illness. Thus, cognitive deficits may limit one's ability to effectively appraise and respond to stressors.
One of the most debilitating consequences of schizophrenia is the breakdown of interpersonal relationships. This can be confirmed by the results of the current study which revealed that half of the studied subjects reported that they didn't have social support in their life. A plausible reason to explain the smaller network sizes among the studied sample is that the schizophrenic patients impose a considerable burden on their caregivers. As mental disorders progress, mentally ill clients lose those members of their networks, probably due to caretakers’ burn--out, making the networks smaller and ultimately causing more networking crisis. In this respect, Harvey et al. [23] suggested that relatives of people with schizophrenia avoid frequent contact with their patients because they appraise this caring more distressing than relatives of patients with other psychotic diagnosis. Hence, one of the tasks of psychiatric nurses is to safeguard social relationships of young patients who develop a schizophrenic illness, before experiencing a network crisis or loss of social contacts.
The results of the present study revealed also that social support was the strongest predictor of the task--oriented coping strategy among the studied subjects. This finding supports the literature suggesting that better coping is associated with greater sense of social support [24--27]. This can be justified in the light of "interactive/buffering model" of schizophrenia which indicates that mobilization of social support resources, might dampen the overall stressors impact, as well as furnishes adaptive ways of coping strategies [28,29]. Having people to talk with, meeting demands for emotional solace, and sharing private feelings, might modify one's perception of the distressing nature of negative events. This may also influence problem solving coping, directed at changing or managing the stressful situation, by enhancing appraisal of one’s ability to handle the adversity. This lent further support to "rich get richer" model, which views the more and better social support one has, the higher chances for improving his/her psychological well-- being, through higher likelihood of selecting active coping strategies, having more confidence, and more control over his/her situation [30].
Collectively, social support had a salient effect on increasing the employment of task--oriented coping strategy among the studied schizophrenic patients. Future psychosocial and cognitive-behavioral interventions, with the dual aims of enriching the schizophrenic patients' social networking and improving their coping skills, should be enhanced to help patients with schizophrenia cope with the negative aspects of daily challenges in a constructive manner and to find benefit in adversity related to their severe mental illness.
Conclusion
According to the findings of the present study, it can be concluded that studied outpatients with schizophrenia resort to endorse emotional-- focused and avoidance-- focused coping strategies more frequently than task--focused coping strategy to deal with stressful life events. Social support was proved to be the independent predictor of the task--oriented coping strategy.
References
- Barkur S (2002) Schizophrenia: A genetic perspective. International Journal of Molecular Medicine 9(3): 207-212.
- Awad AG (1992) Quality of life of schizophrenic patients on medications and implications for new trials. Hosp Community Psychiatry 43(3): 262-265.
- Stip E, Caron J, Renaud S, Pampoulova T, Lecomte Y (2003) Exploring cognitive complaints in schizophrenia. Compr Psychiatry 44(4): 331 -340.
- Adeb S (2007) The relation between quality of life and locus of control among schizophrenic out patients. Unpublished Master thesis. Faculty of Nursing, University of Alexandria, Egypt.
- Horan WP, Vtura J, Nuechterlein KH, Subotink KL, Hwang SS, et al. (2005) Stressful life events in recent onset schizophrenia: Reduced frequencies and altered subjective appraisal. Schizophr Res 75(2-3): 363--374.
- http://www.anxietypanic.com/schizophrenia.html
- Norman RM, Malla AK (1993) Stressful life events and schizophrenia: A review of the research. Br J Psychiatry 162(2): 161-166.
- Singh G, Sharan P, Kulhara P (2002) Coping with hallucinations in schizophrenia: A correlational study. Hong Kong Psychiatry 12(3): 5--11.
- Amirkhan J, Auyeung B (2007) Coping with stress across the lifespan: Absolute vs. relative changes in strategy. Journal of Applied Developmental Psychology 28(4): 298-317.
- Strous RD, Ratner Y, Gibel A, Ponnizovsky A , Ritsner M (2005) Longitudinal assessment of coping abilities at exacerbation and stabilization in schizophrenia. Compr Psychiatry 46(3): 167-175.
- Chan C, Chi Hon H, Chien W, Lopez V (2004) Social support and coping in Chinese patients undergoing cancer surgery. Cancer Nurs 27(3): 230-236.
- Mccorkle BH, Rogers ES, Dunn EC, Lyass A, Wan YM (2008) Increasing social support for individuals with serious mental illness: Evaluating the compeer model of intentional friendship. Community Ment Health J 9(5): 359-366.
- Bronowski P, Zaiuska M (2008) Social support of chronically mentally ill patients. Archives of Psychiatry and Psychotherapy 2: 13-19.
- Rudnick A, Martins J (2009) Coping and schizophrenia: A re-analysis. Arch Psychiatr Nurs 23(1): 11-15.
- Lysaker PH, Louanne WD, Lightfoot JB, Hunter N, Stasburger A (2005) Association of neurocognition, anxiety, positive and negative symptoms with coping preference in schizophrenia spectrum disorders. Schizophr Res 80(2-3): 163-171.
- Muller B, Nordt C, Louler C, Rueesch P, Roessler W (2006) Social support modifies perceived stigmatization in the first years of mental illness: A longitudinal approach. Soc Sci Med 62(1): 39--49.
- Huang CY, Sousa VD, Tsai CC, Hwang MY (2008) Social support and adaptation of Taiwanese adults with mental illness. J Clin Nurs 17(13): 1795-1802.
- Endler NS, Parker JD (1990) Multidimensional assessment of coping: a critical evaluation. J Pers Soc Psychol 58(5): 844-854.
- Flaherty J, Gaviria FM, Pathak DS (1981) The measurement of social support: the social support network inventory. Compr Psychiatry 24(6): 521-529.
- Rollins AL, Bond GR, Lysaker PH, John H, McGrew (2010) Coping with positive and negative symptoms of schizophrenia. American Journal of Psychiatric Rehabilitation 13(3): 208-223.
- Kao YC, Liu YP (2010) Effects of age of onset on clinical characteristics in schizophrenia spectrum disorders. BMC Psychiatry 10: 63.
- Wilder-Willis KE, Shear PK, Steffen JJ, Borkin J (2002) The relationship between cognitive dysfunction and coping abilities in schizophrenia. Schizophr Res 155(3): 259-267.
- Harvey K, Burns T, Sedgwick P, Higgitt A, Creed F, et al. (2001) Relatives of patients with severe psychotic disorders: factors that influence contact frequency. Report from the UK700 trial. Br J Psychiatry 178: 248-254.
- Macdonald EM, Pica S, Mcdonald S, Hayes RL, Baglioni AJ (1998) Stress and coping in early psychosis. Role of symptoms, self-efficacy, and social support in coping with stress. Br J Psychiatry Suppl 172(33): 122--127.
- Lakey B, Lutz CJ (1996) Social support and preventive and therapeutic interventions. Handbook of Social Support and the Family, pp. 435-465.
- Hultman CM, Wieselgren IM, Ohman A (1997) Relationships between social support, social coping and life events in the relapse of schizophrenic patients. Scand J Psychol 38(1): 3--13.
- Berry K, Barrowclough C, Byrne J, Purandare N (2006) Coping strategies and social support in old psychosis. Soc Psychiatry Psychiatr Epidemiol 41(4): 280-284-.
- Cohen S, Wills TA (1985) Stress, social support, and the buffering hypothesis. Psychol Bull 98(2): 310-357.
- Crits-Christoph K (1985) Dimensions of social support, stress, and symptomatology among chronic schizophrenics: an examination of the buffering hypothesis. Published Doctoral Dissertation. University of Fordham, New York, USA.
- Kim J, Han JY, Shaw B, McTavish F, Gustafson D (2010) The roles of social support and coping strategies in predicting breast cancer patients’ emotional well-being: testing mediation and moderation models. J Health Psychol 15(4): 543--552.






























