The Extent of Midwives' Knowledge and Practices during the Provision of Immediate Postnatal Care in Swaziland
Bongani Robert Dlamini1*, Peter T Sandy2 and Wendy P Gule3
1Program specialist-SRH, Swaziland
2Lecturer for Public Health, University of South Africa, South Africa
3Lecturer, Southern African Nazarene University, Swaziland
Submission: July 20, 2017; Published: August 18, 2017
*Corresponding author: Bongani Robert Dlamini, Program specialist-SRH, HIV & Youth at UNFPA for the Swaziland Country Office, Swaziland, Tel: +268-76176844; Fax: 268-24049974; Email: bonganidlamini.bd@gmail.com
How to cite this article: Bongani R D, Peter T S, Wendy P G. The Extent of Midwives' Knowledge and Practices during the Provision of Immediate Postnatal Care in Swaziland. JOJ Nurse Health Care. 2017; 3(4): 555616. DOI: 10.19080/JOJNHC.2017.03.555616
Abstract
The purpose of this study was to determine midwives’ knowledge and practices during the provision of immediate postnatal care (PNC) interventions within 24 hours of after birth. Quantitative descriptive cross-sectional design study was used. Eighty eight (88) midwives participated in the study. The study highlighted that midwives have the relevant qualification; 70.5% were state certified midwives with a second registered certificate in midwifery, 27.3% had bachelor’s degrees, while 2.3% had Advanced Midwifery certificate. However, serious gaps were identified in their knowledge and practices. About 42.0% (n=37) of respondents were not measuring maternal pulse during this postnatal period. Whilst 43.2% of the respondents reported that they had monitored maternal respiratory rate, 56.8% did not see the importance of maternal respiratory rate monitoring at discharge. Uterine contraction assessment on every mother before discharge from hospital is vital, however, 44.5% (n=39) of the midwives did not include uterine contraction assessment in the package of care they offer to mothers on discharge. About 26.1% (n=23) reported that they did not conduct physical examination on mothers at discharge. These findings call for urgent attention on the competencies of midwives and the provision of quality immediate PNC in Swaziland.
Keywords: Postnatal care; Midwives; Mothers; Postpartum
Introduction
Every day, approximately 800 women die from preventable causes related to pregnancy and childbirth, due to negligence and inadequate healthcare [1]. The majority (99%) of these deaths occurs in developing countries, sub- Saharan Africa region alone accounts for 62% (179 000) of maternal deaths [2]. Of note is that postpartum deaths account for 60% of all maternal deaths, compared to only 15.5% for intrapartum and 23.9% for antepartum [3,4]. This might mean that provision of quality care or attendance by skilled birth attendant during this time could prevent or at least reduce maternal deaths.
These women die from known, preventable and medically manageable causes, such as severe bleeding, hypertension, infections and obstructed labor. The major contributing factors to these deaths from this global problem are delays in making decision to go to the health facilities and being offered quality and appropriate care [4]. Although women may sometimes seek help from health facilities on time, the quality of the services offered in these facilities in the developing world are in the main substandard. This is reflected in the high (99%) maternal mortality ratio in developing countries, like Swaziland and Lesotho [3]. If quality PNC in the postnatal period, particularly during the first 24 hours after childbirth could reach 90% of mothers and their babies, about 4% to 27% infant mortality could be averted in Sub-Saharan Africa [5].
Whilst the risk of dying in pregnancy is a concern in Sub- Saharan Africa, the majority of maternal deaths (60%) occur during the postnatal period. Although this is the case, this critical time is the most neglected period of the maternal newborn- health continuum of care [6]. In Swaziland, maternal mortality ratio remains high (593/100 000) despite the high skilled birth attendance at 88% [7]. Swaziland has well performing maternal health related indicators, such as high (88%) skilled birth attendance, 82% hospital delivery rate, 98% and 77% ANC attendance by pregnant women at least once and or four times respectively as well as high (89%) coverage of prevention of mother to child transmission of HIV program [8]. The question now arises, why the country still has high maternal mortality ratio?
Some researchers Shongwe R et al. [9] noted in their study that midwives are generally not consistent in measuring maternal vital signs like blood pressure, temperature, pulse and respiration. If changes in vital signs are noted early, postnatal complications can be managed before they become life threatening [10]. Unfortunately, changes in maternal vital signs are sometimes not identified by midwives in Swaziland during the postnatal period [11]. Such lapses in clinical practice have been reported to result in maternal deaths from complications, such as postpartum bleeding, particularly among HIV-positive mothers [12]. Midwives form an important part of the healthcare workforce in the provision of maternal newborn child healthcare worldwide, including the critical immediate postnatal periods [13]. In Swaziland, midwives attend to a huge number of mothers during pregnancy, labor and delivery, including postnatal periods. So, the quality of care offered to mothers depends largely on the knowledge and skills of this professional group. Taking this into account and the view that about 60% of these deaths occur within 24 hours of post-delivery, it is assumed that if skilled birth attendance could be provided during this time, the high maternal mortality ratios thus far highlighted could be reduced.
Materials and Methods
Design
The present study utilized a quantitative cross-sectional design to investigate the competencies of midwives during the provision of immediate PNC services to mothers and their newborns.
Sample
A simple random sampling approach was used to select the study sites. The researcher established a sampling frame and the elements of this sampling frame were the all the 11 maternities, which were numbered to facilitate random selection. A table of random numbers was used to select the study sample. The result of this exercise was the selection of a total of six maternities. These are in the four regions (Hhohho, Manzini, Lubombo and Shiselweni) of the country. Regarding the sampling of the respondents; a systematic random sampling technique was used to select respondents of the study. This approach was adopted to minimize sampling bias as each respondent had an equal chance of being selected. There were 114 midwives in the study sites (6 maternities) and the desired sample size for the study was 88, based on table of minimum sample size for quantitative studies. The level of statistical significance for the sampling of respondents was set at p<0.05. This sample size was representative of the midwifery population in maternity units and results could be generalized back to the midwifery population in maternity units in Swaziland.
Data collection
Data were collected using structured questionnaires, which contained open-ended questions at the end. Face-to-face structured interviews were conducted between January 2014 and June 2014 in the selected study sites. The questionnaires were divided into a number of sub-sections: Section A included demographic information, such age, marital status, and level of education about the respondents. Section B included clinical immediate PNC interventions to be offered to HIV-positive mothers and section C included open-ended questions.
Data management and analysis
Collected data were securely kept in a locked cupboard and only accessible to the researcher. Trained research assistants captured data into the computer. Captured data were exported and analysed using IBM SPSS Statistics, version 22.0. Descriptive and inferential statistics were the two approaches to data analysis used in this study.
Ethical considerations
Ethical approval was sought from the Ministry of Health in Swaziland. The University of South Africa Higher Degrees Committee of the Department of Health Studies approved the protocol. Lastly, the participants who took part in the study; their consent was sought verbally and written before each interview. The researchers adhered to all ethical issues related to human research.
Results
Characteristics of respondents
A majority (43.2%, n=38) were within the age range of 3039 years, 33.0% (n=29) were in the range of 29 years and below, and 19.3% (n=17) in the range of 40-49 years. About 4.5% (n=4) of the respondents were 50 years and above. This means that a majority of the workforce in these facilities was within the productive age.
Experience and education
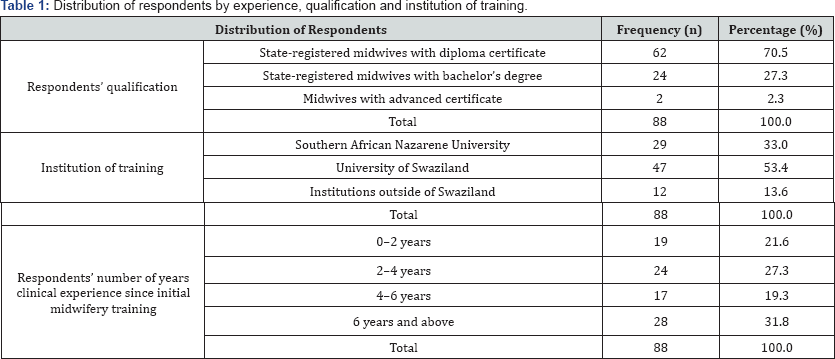
Table 1 depicts the midwives' years of experience, institution of training, and qualifications. All respondents were licensed to practice midwifery in Swaziland, 67.0% (n=62) had a Postgraduate Diploma in Midwifery qualification, 27.3% (n=24) had a Bachelors degree with a midwifery speciality, and only 2.3% (n=2) had Advanced Midwifery Certificate (higher qualification midwifery in the country). Of the 88 respondents, 31.8% (n=28) had more than 6 years of experience of midwifery practice, 27.3% (n=24) had 2-4 years, 19.3% (n=17) had 4-6 years and 21.6% (n=19) had 0-2 years of experience.
In-service capacity building: attendance, frequency and types of trainings
All the respondents (100%, n=88) in this study reported that they attended in-service trainings. The most attended training that respondents reported was prevention of mother-to-child transmission (78.4% (n=69), followed by HIV testing and counseling (46.6%, n=41), Emergency Obstetric and neonatal care (30.7%, n=27), and PNC (8.0%, n=7).
Midwives' knowledge and practices of maternal immediate postnatal care interventions
Respondents reported that mothers generally stay for a short period in health facilities post childbirth. They went on to state that mothers are usually discharged from hospital within the critical immediate postnatal period (within 24 hours of postdelivery). According to respondents this indicated the need for midwives to provide quality interventions and comprehensive services to mothers and infants following discharge from health facilities.
Maternal vital signs assessment
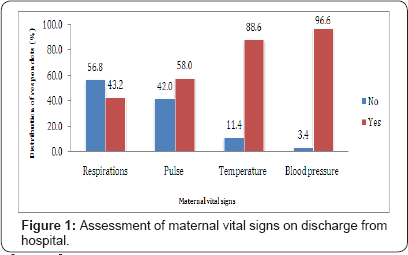
About 80% (n=78) of respondents mentioned that they measured the temperature of mothers on discharged from the health facilities. Respondents stressed that maternal pulse is another parameter they claimed should be measured when discharging mothers from health facilities. About 58.0% (n=51) of respondents claimed that they measured maternal pulse of mothers during the postnatal period. Forty two percent (n=37) of respondents did not do so. Measurement of maternal blood pressure was identified as another critical intervention. The majority of the respondents (96.6%, n=85) reported that they measured the blood pressure of mother during the postnatal period. Whilst 43.2% of the respondents reported that they had monitored maternal respiratory rate, 56.8% did not see the importance of maternal respiratory rate monitoring. Uterine contraction assessment on every mother before discharge from hospital is important. However, 44.5% (n=39) of the midwives did not include uterine contraction assessment in the package of care they offer to mothers on discharge. Figure 1 shows maternal vital assessment by midwives during the time of discharge from health facilities.
Physical examinations
The respondents reported that physical examination was critical during the immediate postnatal period, particularly for HIV-positive The majority of the respondents (73.9%, n=65) reported to provide or offer this intervention to mothers in the postnatal period. About 26.1% (n=23) reported that they did not conduct physical examination on mothers. Respondents talked about pelvic examination, and 87.5% (n=77) of them reported that they conducted this examination. However, 12.5% (n=11) of the respondents did not report anything on pelvic assessment.
Drug administration
It was noted from respondents that mothers on antiretroviral therapy and or antiretroviral prophylaxis should take their prescribed medications on time. Doing so would not only prevent drug resistance, but it would also reduce the risk of mother-to-child transmission of HIV. However, 51.1% (n=45) of the respondents did not offer these medications nor counseling to HIV-positive mothers on discharge from the postnatal wards. Mothers sometimes sustain injuries during childbirth on the nerve endings of traumatized vaginal tissue. Respondents claimed that this might require the provision of oral analgesics. But 67.0% (n=59) of the respondents reported that they have not provided analgesics to postnatal mothers even to those with these injuries.
Immediate postnatal care counseling provision within the 24 hours of discharge
It was noted by respondents of this study that the discharge of HIV-infected mothers within 24 hours of post-delivery means that women should be provided with comprehensive information. The provision of information would empower mothers, and subsequently enable them to take care of themselves and their babies. In addition, it would enable mothers to be aware of danger signs. Therefore, midwives should provide information on adherence to antiretroviral drugs, maternal danger signs, prophylaxis and family planning.
Maternal danger signs
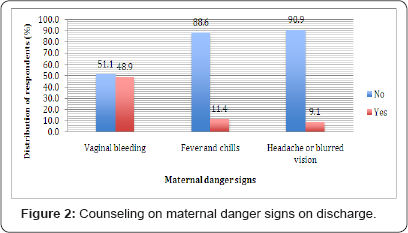
About 50% (n=45) of the midwives who participated in this study mentioned that they were not routinely teaching mothers on the dangers of vaginal bleeding. The majority of respondents (88.6%, n=78) reported that they did not offer counseling to HIV-positive mothers on fevers and chills. Lastly, 90.9% (n=80) respondents reported that they did not offer information on indication of headache and or blurred vision. Figure 2 shows the proportions of maternal dangers counseling when discharging mothers from hospitals.
Adherence to antiretroviral drugs
According to respondents, the aim of antiretroviral drugs administration to breastfeeding mothers is to prevent mother- to-child transmission of HIV, and promote the physical wellbeing of the HIV-positive mothers. Most of the respondents (87.5%, n=77) reported that they were routinely offering adherence counseling to HIV-positive mothers at discharge from hospital. However, about 12.5% (n=11) of the respondents did not offer such vital information.
Family planning
Respondents reported that educating HIV-infected mothers on family planning was important. Even though this was the case, the majority of the respondents (63.6%, n=56) did not provide information on family planning to HIV-positive mothers when discharged from the postnatal wards.
Summary of Findings
Maternal postnatal care intervention offered within 24 hours of discharge. Lack of space in maternity units makes mothers to be discharged within 24 hours post-delivery from health facilities. This study revealed that on average mothers were discharged from health facilities within 12-24 hours after childbirth. This does not allow midwives to adequately observe mothers and newborns to ascertain whether they are recovering well [5]. Therefore on discharge mothers, particularly HIV- infected mothers have to be provided with quality immediate PNC services. Midwives have to effectively measure and record vital signs, conduct physical examination, provide prophylaxis and counseling.
Maternal vital sign assessment
Vital signs monitoring is a fundamental component of midwifery care during the immediate PNC period [14]. It is the professional responsibility of midwives to assess these so as to diagnose or identify problems early as well as manage such complications promptly. Mothers with body temperature of about 38 degrees Celsius should be provided with prophylactic antibiotics, especially on discharge from health facilities. Such body temperature is an indication that the body is waging a war against infection [15]. Another critical parameter to be assessed on discharge is the maternal pulse. Pulse assessment could help in early identification of blood circulation problems, such as fast thread pulse which could indicate hypovolemia. Therefore, pulse assessment is essential and form an integral part of the discharge plan for mothers within the first 24 hours post-delivery. Hypertensive disorders are the third major contributing factors to maternal deaths. Blood pressure assessment could help in the early identification of such disorders. Respiration variation from the normal range could indicate a severe derangement in many body systems, not just the respiratory system [16]. This study revealed that 56.8% of the midwives who participated did not report that they routinely assess this vital sign. This confirms that the respiratory rate is an important indicator but most neglected vital sign.
The above mentioned reasons for vital sign assessment among mothers during the postnatal care period are integral and forms the backbone of care to be rendered on discharge. Regarding the assessment of vital signs, this study revealed that of the 88 midwives who were part of the study, 88.6% mentioned that they measure temperature for their postnatal mothers on discharge from the health facility. About 58.0% mentioned to be routinely assessing pulse rate among mothers on discharge. A majority (96.6%) mentioned that they routinely measure blood pressure for postnatal mothers on discharge. The latter confirms that the vital signs are important indicators of postnatal mothers' health status but most neglected [14]. This gap could result to unidentified maternal complications.
Maternal physical assessment
Clinicians state that a general physical assessment provides a quick overall review or first impression of the postnatal mother. This includes alertness and orientedness; signs of acute distress, body structure/mobility (such as standing erect, sits comfortably; gait is coordinated; walk is smooth and well balanced etc) and behavior (maintains eye contact with appropriate expressions; comfortable and cooperative; looks clean and fit; appears clean and well-groomed etc.) [12]. Information from this assessment in postnatal mothers could help in early identification of postpartum complications such puerperal psychosis, poor hygiene, and dizziness. There were 88 respondents that were involved in this study, 73.9%, of them mentioned that they routinely perform such an assessment. The remaining percentage (26.1%) shows that some mothers could leave health facilities with unidentified puerperal complications. Another vital assessment to be performed by midwives on discharge of mothers during the immediate PNC period is uterine contraction assessment. This is because the major common cause of postpartum bleeding is uterine atony [17]. This is very important, knowing that postpartum bleeding is the global and national leading cause of maternal deaths. One diagnostic maneuver for postpartum bleeding is palpation of the uterus, to ascertain the extent of its contraction [17,6].
Midwives should know the rationale; have the knowledge and skills to perform such interventions to postnatal mothers. However, of the 88 midwives who participated in this study 44.5% did not mentioned that this was a vital and critical intervention to be routinely performed to mothers on discharge during the PNC period. This professional gap in the practice of midwives is very detrimental to the health of mothers, especially immune compromised mothers. This is because mothers are at risk of complications during the PNC period, due to the perineum physiologic process that occurs during birth. These could result to bleeding. Midwives are to conduct pelvic and vaginal examination to postnatal mothers on discharge, to help identify puerperal complications like vaginal tears. A significant percentage (13%) of the midwives who participated in this study reported not offering or performing such an important postnatal examination. Whilst [18] state that perineum examination is a diagnostic maneuver for diagnosing postpartum bleeding. Failure to perform perineum examination could lead to mothers dying from undiagnosed post-delivery vaginal bleeding.
Immediate postnatal care counseling provision within 24 hours of discharge
The fact that mothers are discharge within 24 hours post-delivery, this requires that women be provided with comprehensive information. This will enable these mothers to be on guard for danger signs. It is the professional role of the midwives to offer counseling to HIV-infected mothers on discharge. Comprehensive information on maternal danger signs and family planning is critical.
Maternal danger signs
If midwives could create awareness about health issues surrounding postpartum care among mothers; this could result to improved health status of the mothers [19]. It is estimated that 15% of pregnant women who experience complications are at risk of developing poor, yet preventable, postpartum outcomes [19]. Enabling postpartum women to recognize early signs and symptoms of postpartum complication is a primary step toward seeking timely obstetric care before lives of mothers or their babies are endangered [20]. Research has shown that puerperal complications may not be regarded as abnormal by most women, owing to a lack of understanding regarding important early danger signs [20].
Many early signs and symptoms of the leading causes of maternal deaths, such as thromboembolic disease, eclampsia, and sepsis, are not recognized by a large proportion of mothers and their families [20]. Failures to identify these signs may lead to delayed decision in seeking care, which is reported to be a contributing factor in 30%-77% of all maternal deaths [20]. Several studies conducted in obstetrics indicate that health education about postpartum danger signs and symptoms targeting women of reproductive age, increase awareness and recognition of complications, motivate women to seek timely support, and improve referral to health services [21].
Midwives are to counsel mothers on postpartum danger signs. However, this study reported that 48.9% of the 88 midwives did not mention that they were routinely teaching mothers on the dangers of vaginal bleeding. A majority (88.6%) reported not educating HIV-infected mothers upon discharge from hospital on indication of fever and chills. About 90.9% reported not offering information on indication of headache and or blurred vision. This study confirms a Burkina Faso study, which found that 55% of all maternal deaths were due to lack of awareness about danger signs and symptoms [20]. This gap may contribute to delayed decision in seeking care, which is reported to be a contributing factor in 30%-77% of all maternal deaths [20].
Family planning
Provisions of accessible and affordable family planning services, skilled birth attendants as well as provision of emergency neonatal and obstetric care are the key strategies to reduce maternal deaths. It is estimated that provision of family planning methods alone can reduce maternal deaths by 30% [22]. Unmet need among HIV-positive mothers in Swaziland is very high at 63% [8]. This provides an additional rationale for midwives to educate mothers, especially HIV-infected mothers on family planning methods during postnatal care. These services are almost free in public health facilities. This intervention could enhance the country towards the achievement of Sustainable Development Goal 3. Of the midwives (N=88) who participated in this study 63.6% did not mentioned that they regularly provided information on family planning services to HIV- positive mothers. This could be the reason the country has high unmet need for family planning services among mothers living with HIV. This study confirms a study conducted by Dlamini B [11] which reported that as many as 34.1% of the respondents (N=372) were put at risk of unplanned pregnancies and HIV reinfection, because midwives did not advise and educate them on available and accessible family planning options.
Strengths and limitations of study
Although some qualitative data was collected, inclusion of a Q-methodological approach, in other words, the adoption of a mixed methods approach in the study could have helped in refining the guidelines that were adapted, as this approach could help in generating more insight into this area of study. Despite the above limitations, the study could revealed the gaps on the competencies of midwives during the provision of immediate PNC revealed gaps in the provision of immediate PNC to mothers and their infants.
Conclusion
The findings on the competencies of midwives during the provision of immediate PNC revealed gaps in the provision of immediate PNC to mothers and their infants. The gaps revealed by the study se findings call for urgent attention on the competencies of midwives and the provision of quality immediate PNC in Swaziland. Strategic inventions need to be undertaken; these involve adaptation of internationally approved evidence- based guidelines and conceptual framework. Globally, there are evidence-based guidelines available that reputable agencies, such as the WHO and the National Institute for Health and Care Excellence have published to guide midwives’ practice during the provision of immediate PNC.
Acknowledgment
The authors are grateful to the Swaziland Ethics Review Board as well as the University of South Africa Higher Degrees Committee of the Department of Health Studies for the ethical approval approved the protocol and to all midwives who voluntarily participated in the study.
Sources of Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- World Health Organization (2014) Maternal Mortality, Geneva, Switzerland.
- (2014) World Health Organization, United Nations Children Emergency Fund, United Nations Population Fund, World Bank & United Nations Population Division. Trends in maternal mortality: 1990 to 2013. Estimates by WHO UNICEF UNFPA the World Bank and the United Nations Population Division Geneva WHO, Geneva, Switzerland.
- World Health Organization (2010) Maternal mortality, Geneva, Switzerland.
- Jacobson N (2011) Postnatal care.
- Warren CDP, Toure L, Mongi P (2006) Postnatal care.
- World Health Organization (2014) WHO recommendations on postnatal care of the mother and newborn. Geneva: WHO. Geneva, Switzerland.
- Kingdom of Swaziland Central Statistical Office (2015) Swaziland 2012 Demographic and Housing Survey Key finding results. Mbabane Central Statistical Office, Swaziland.
- Central Statistical Office (2016) Swaziland Multiple Indicator Cluster Survey 2014. Final Report. Mbabane Central Statistical Office and UNICEF, Swaziland.
- Shongwe R, Warren C (2010) Practices and experiences of postnatal women in Swaziland. Mbabane Webster Print, Swaziland.
- Leifer G (2008) Maternity nursing: An introductory text (10th edn), Saunders Elsevier, Philadelphia, USA.
- Dlamini B (2013) An evaluation of postnatal care rendered to HIV- positive women and their infants. Pretoria University of South Africa.
- London M, Ladewig PW, Ball JW, Bindler RC (2007) Maternal and child nursing care (2nd edn), Philadelphia PA Pearson Prentice Hall, USA.
- United Nations Population Fund, Internal Confederation of Midwives & World Health Organization (2014) The state of the world's midwifery 2014: A universal pathway. A woman's right to health New York United Nations, USA.
- Rose L, Clarke SP (2010) Vital signs no longer a nursing priority? Am J Nurs 110(5): 11.
- Murray SS, McKinney ES (2006) Foundations of maternal-newborn nursing (4th edn), Saunders Elsevier, Philadelphia, USA.
- Elliott M, Coventry A (2012) Critical care: The eight vital signs of patient monitoring. Br J Nurs 21(10): 621-625.
- Hofmeyr GJ, Abdel-Aleem H, Abdel-Aleem MA (2013) Uterine massage for preventing postpartum haemorrhage. Cochrane Database of Syst Rev 7: CD006431.
- Hodgins S, Pradhan YV, Khanal L, Upreti S, Naresh PKC (2013) Chlorhexidine for umbilical cord care: Game-changer for newborn survival? Glob Health Sci Pract 1(1): 5-10.
- Okour A, Alkhateeb M, Amarin Z (2012) Awareness of danger signs and symptoms of pregnancy complication among women in Jordan. Int J Gynaecol Obstet 118(1): 11-14.
- Kabakyenga JK, Ostergren P, Turyakira E, Pettersson KO (2011) Knowledge of obstetric danger signs and birth preparedness practices among women in rural Uganda. Reprod Health 8: 33.
- Pembe AB, Urassa DP, Carlstedt A, Lindmark G, Nystrom L, et al. (2009) Rural tanzanian women's awareness of danger signs of obstetric complications. BMC Pregnancy Childbirth 9: 12.
- Smith R, Ashford L, Gribble J, Clifton D (2009) Family planning saves lives (4th edn), Washington Population Reference Bureau, USA.






























