Promoters and Obstructers of Hierarchical Treatment System
Min Zhou1,2*, Lindu Zhao2, Kathryn S Campy3 and Song Wang1
1Hunan University of Commerce, China
2Southeast University, China
3University of Pennsylvania, USA
Submission: July 28, 2017; Published: August 10, 2017
*Corresponding author: Min Zhou, Assistant Professor, School of Business Administration, Hunan University of Commerce, China, Tel: 086073188689006; Email: zhouminlaoshi@163.com
How to cite this article: Min Z, Lindu Z, Kathryn S C, Song W. Promoters and Obstructers of Hierarchical Treatment System. JOJ Nurse Health Care.2017; 3(1): 555601. DOI: 10.19080/JOJNHC.2017.03.555601
Abstract
The establishment of a scientific and orderly Hierarchical Treatment System (HTS) is an important way to improve the efficiency of medical and health resources and reduce medical expenses. Government health management officials and health insurance departments are the main promoters of the establishment of a hierarchical treatment system. Hospital managers and medical staff are the main obstacles to policy implementation because they are more likely to suffer damage in hierarchical treatment system.
Keywords: Hierarchical treatment system; Promoters; Obstructers; Health care reform
Introduction
The establishment of a hierarchical treatment system and strengthen the top design of it, and scientific design grass-roots first diagnosis system, two-way referral path and key links, will help optimize the allocation of medical resources and reduce medical expenses. The classification and treatment system is an effective measure for the reform of health care system.
China's hierarchical treatment system practice encountered numerous difficulties [1-4]. In China, large general hospital patients overcrowding, the problem is still grim. Medical services provided by medical institutions at all levels cannot achieve homogeneity. Because the lack of integration of medical resources, it is unable to form an effective linkage mechanism. Two-way referral system has not yet been completely established. In 2016, the number of outpatients in Changsha City transferred from the community hospital to the higher level hospital is more than 76,000, and the number of outpatients transferred from the higher hospital to the community hospital is less than 7,000; the number of inpatients transferred from the community hospital to the higher hospital referral is reached more than 8,000 people, and the number of inpatients transferred from the higher hospital to the community hospital is less than 500. It is easy to transfer from the community hospital to the higher hospital, but the reverse transfer is difficult [5].
Advanced experiences in developed countries
Britain is one of the earliest and most stringent Western countries in practice. After years of development and improvement, the British welfare system becomes the typical representative. As a «gatekeeper» for the health of citizens, general practitioners to guide patients with systematic orderly medical treatment, on-demand treatment. British law ensures the protection of community first visit. According to British law, a British citizen or a foreign citizen who has a visa for more than six months must register and sign with a family doctor, and in non-emergency situations, the community residents must first go to the general practitioner after illness and decide for follow- up treatment scheme [6]. The typical practitioner determines whether the patient is eligible for secondary or tertiary medical services, and the standardized pathways of various types of diseases in the UK contribute to the standardization of referral.
The United States is the sole country in the western developed countries, which do not achieve universal coverage, and its medical service model is based on private medical care and insurance. On this basis, the government supports social insurance for special groups. US medical institutions are organized in community health service agencies, secondary hospitals and tertiary hospitals. The three types of hospitals in the United States are clear and have a clear division of labor, which can effectively meet the medical needs of different patients and provide a solid foundation for good practice of grading clinics in the United States. Health care management in the United States ceases to be a two-way alternative between patients and doctors. It focuses more on monitoring the supply of health services, health service providers and managed health care organizations, and strictly controls the rights and interests of participants. Diagnostic-related groups, DRGs) provide an important basis for the management and reimbursement of various insurance. This payment method limits the standardized hospitalization indications and the time period. That is, a disease or surgery [7]. The patient is returned to a certain extent, Must go to the primary health care institutions or go home to accept the general practitioner treatment. Otherwise, the discharge of treatment costs discharged by the patients themselves. Years of practice shows that DRGs take into account the interests of the government, hospitals, patients, but also to restrict the patient's medical treatment behavior, facilitate the orderly conduct of a two-way referral.
Stakeholders of hierarchical treatment system
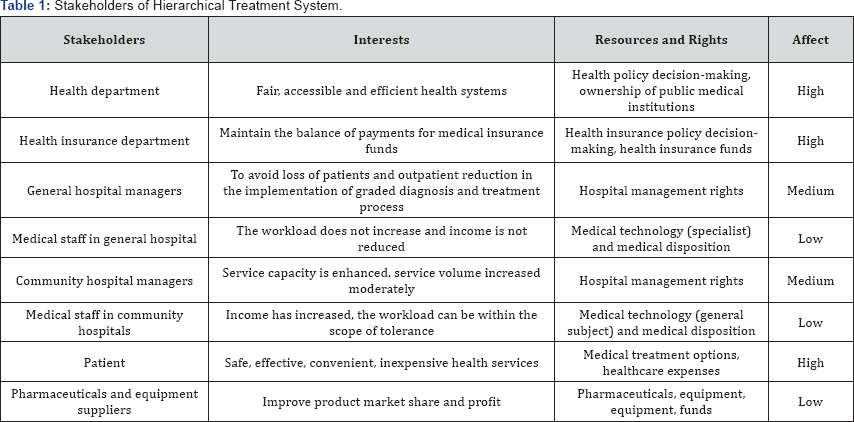
The construction and operation of the Hierarchical Treatment System involve the demand side, the supply side, the management side of the health service. The main participants and their interests are analyzed as showed in Table 1.
Discussion
From the perspective of stakeholders, hierarchical treatment has both a driving force and a hindrance factor. The final implementation of the classification can be achieved and whether policy expectations can be achieved, depending on the dynamic balance [8-10].
Health department and health insurance department are mainly promoters of hierarchical treatment system. The implementation of the hierarchical treatment system is conducive to optimizing the allocation of medical and health resources and to reduce the cost of medical treatment, control of medical and health costs. This is the fundamental duty and core interest of the health department and the health care department. In the construction of hierarchical treatment system, health department and health insurance department have a high degree of consistency: positive promoters. However, they differ in the implementation route. Built on the perspective of medical service providers, the health department generally advocates the rational allocation of remedial service resources through administrative means, and reasonable arrangements for all types of medical and health services. Then, the health department takes comprehensive measures to guide residents/ patients to adapt this institutional arrangements, and ultimately to achieve hierarchical treatment. On the contrary, based on the perspective of medical demanders, the health insurance department is inclined to establish a doctor based on practice or free practice of the family (general) doctor signing system [11,12]. The establishment of supporting health insurance payment reform can rationalize the income mechanism of doctors to achieve long-term stable relationship between patients and doctors, so as to provide patients with continuous medical services and full of health management services [13].
According to the basic principles of hierarchical treatment system, the general hospital should be mainly responsible for difficult diagnosis and treatment work and scientific research and education work, chronic diseases and common diseases gradually diverted to community hospitals. Therefore, for the general hospital, the implementation of hierarchical treatment system may mean that the reduction in outpatient. If there are no other compensation measures, it will result in a reduction in economic income, which is detrimental to both the hospital manager and the medical staff. In such circumstances, hospital administrators and medical staff on the classification of the conflict and obstruction will be exacerbated. To fundamentally reduce the general hospital's obstruction of the hierarchical treatment system, the government should take systematic and effective measures to improve its operational development model, in particular, to break interests chase mechanism of the general hospital.
The interests of managers and medical staff in community hospitals are the most likely to the expected effect of hierarchical treatment system. Therefore, both of them are happy to see the implementation of the policy, and are willing to actively participate in it. To further stimulate their enthusiasm, the government needs to address three key points. One is to improve the social reputation of community hospitals and general practitioners. The second is to ensure the status of general practitioners, and finally is to improve the income of community hospitals and general practitioners [14].
Patients are an important beneficiary of hierarchical treatment system, but they may also serve as the biggest obstacle. In the hierarchical treatment system, patients who need to receive the treatment of community doctors who they don't trust, and if not directly referral to a large hospital they will pay a higher fee, or only get a lower proportion of reimbursement. So whether it is from the medical habits or the subjective feelings, the patient may have resistance to the classification of treatment. Therefore, the government needs to educate patients to improve the patient’s understanding and approval of this policy.
Pharmaceuticals and equipment suppliers will be selectively involved in the process, and they are expected to become the driving force of hierarchical diagnosis and treatment. At present, under the active promotion of pharmaceuticals and equipment suppliers, applications which based on the Internet, Internet of Things, Big Data and Cloud Services are rapidly developing health care. Precision medical, wisdom, medical, mobile medical, digital medical, online medical and other concepts have gradually become a reality, and all kinds of doctors continue to rise in collaborative organizations. Online virtual medical institutions began to explore the establishment. These innovative models will significantly improve the efficiency of the use of medical resources, to provide technical support for the classification of hierarchical treatment system [15,16].
Acknowledgement
This work was supported by National Natural Science Foundation of China (Grant No. 71601043, 71671039, 71671040).
References
- (2015) National Health and Family Planning Commission of the People's Republic of China. The patient expenses of National two grade hospital and high level hospitals.
- Li WX (2015) Health implications of environmental and social resources for preadolescents in urban China. Habitat International 50: 347-353.
- Pietro AM, Andrea C, Zhao D (2016) Atrial fibrillation in first generation Chinese migrants living in Europe: A proof of concept study. Int J Cardiol 215: 269-272.
- Fan W (2016) Turning point or selection? The effect of rustication on subsequent health for the Chinese Cultural Revolution cohort. Soc Sci Med 157: 68-77.
- Chen SM, He LY (2014) Welfare loss of China's air pollution: How to make personal vehicle transportation policy. China Economic Review 31: 106-118.
- Fiona CG (2016) From SARS to avian influenza: the role of international factors in china's approach to infectious disease control. Annals of Global Health 82(1): 180-188.
- Merican AM (2014) Journalism as National Dialogue Platform: Celebrating the News and Opinion. Procedia - Social and Behavioral Sciences 155(6): 337-340.
- He J (2014) The doctor-patient relationship, defensive medicine and over-prescription in Chinese public hospitals: Evidence from a cross sectional survey in Shenzhen city. Soc Sci Med 123: 64-71.
- Anderson PF, Wescom E, Carlos RC (2016) Difficult doctors, difficult patients: building empathy. J Am Coll Radiol 13(12): 1590-1598.
- Hu J, Mossialos E (2016) Pharmaceutical pricing and reimbursement in China: When the whole is less than the sum of its parts. Health Policy 120(5): 519-534.
- Feng X, Pang M, Beard J (2014) Health system strengthening and hypertension awareness, treatment and control: data from the China Health and Retirement Longitudinal Study. Bull World Health Organ 92(1): 29-41.
- Pingping Li, Qin C (2014) The danger of being a doctor in China. Int J Cardiol 177(2): 15.
- Phillips MR, Zhang J, Shi Q, Song Z, Ding Z, et al. (2009) Prevalence, treatment, and associated disability of mental disorders in four provinces in China during 2001-05: an epidemiological survey.Lancet 373: 2041-2053.
- Yang X, XQ Y (2015) Peritoneal Dialysis in China: Meeting the Challenge of Chronic Kidney Failure. Am J Kidney Dis 65(1): 147-151.
- Guo X, Huang YG (2015) The development of alcohol policy in contemporary China. Journal of Food and Drug Analysis 23(1): 19-29.
- Bhargava S, Choubey S, Mishra S (2016) Vaccines against tuberculosis: A review. Indian J Tuberc 63(1): 13-18.






























