Effects of Occupational Health Nurses and Staff on the Performance of Occupational Health Physicians in the Workplace
Togita Y, Sano Y and Yano E*
Teikyo University Graduate School of Public Health, Japan
Submission: April 13, 2017; Published: May 25, 2017
*Corresponding author: Yano E, Teikyo University Graduate School of Public Health, Japan, Tel: 81-3-3964-5822; Email: eyano@med.teikyo-u.ac.jp
How to cite this article: Togita Y, Sano Y Yano E. Effects of Occupational Health Nurses and Staff on the Performance of Occupational Health Physicians in the Workplace. JOJ Nurse Health Care. 2017; 1(4): 555566. DOI: 10.19080/JOJNHC.2017.01.555566
Introduction
In Japan, Industrial Safety and Health Law 1) requires that workplaces employing 50 or more workers appoint an occupational health physician (OHP) to protect and promote the workers' health. 2) When a workplace has 1,000 or more workers, an OHP is appointed to operate exclusively in a single workplace. For smaller workplaces, most OHPs are on part-time contracts and visit the workplace only once, or a few, times a month. In Japan, it is also mandatory for all employers to provide regular health check-ups for their employees at least once a year. 3) Consequently, the majority of the time that the OHP spends in the workplace is absorbed by dealing with check-up data, which makes it difficult for the OHP to provide the health and safety services expected, such as inspecting the workplace or planning ways to improve workers' health in the workplace. Unlike OHPs, there is no requirement under Japanese legislation for workplaces to appoint occupational health nurses (OHNs). However, to provide sufficient occupational health services, many workplaces employ registered or public health nurses, in addition to an OHP. To implement a program to improve the occupational health services provided by OHPs in the workplace, we conducted a questionnaire survey of the workplaces of a large company group.
In this study, we focused on the effect of OHNs and occupational health staff (OHNs/staff) on the degree of active engagement occupational health services (versus medical data handling) of OHPs in the workplace.
Methods
A questionnaire survey was administered to a large company group with more than 200 member companies, and employing nearly 300,000 workers, in 2013. The questionnaire comprised 38 items related to how health check-up data were handled by, and the performance of OHPs, in terms of whether they were assisted by health and safety staff. Most of the workplaces of the company that have at least 1,000 workers also have a full-time OHP, whereas those with fewer workers have part-time OHPs. The actual services by the OHP were expected to perform (listed in the first column of Table 2 were analyzed), adjusting for the number of hours that they work per monthly. The degree of engagement of the OHP with occupational health services was assessed according to whether health check-up data were processed by OHNs/staff [1,2].
Results
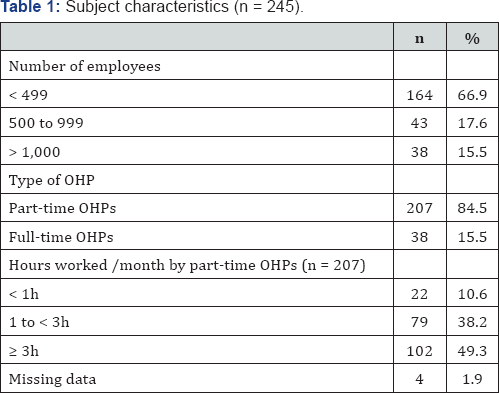
Table 1 shows the characteristics of the workplaces studied. The questionnaire was completed by 245 member companies, of which 15.5% had a full-time OHP and 84.5% had a part-time OHP. Full-time OHPs attended workplace Occupational Health and Safety Committee meetings more frequently, conducted walk-through inspections more often, and performed all services related to the work environment, working practices, and healthcare more frequently than did part-time OHPs (Table 2A).
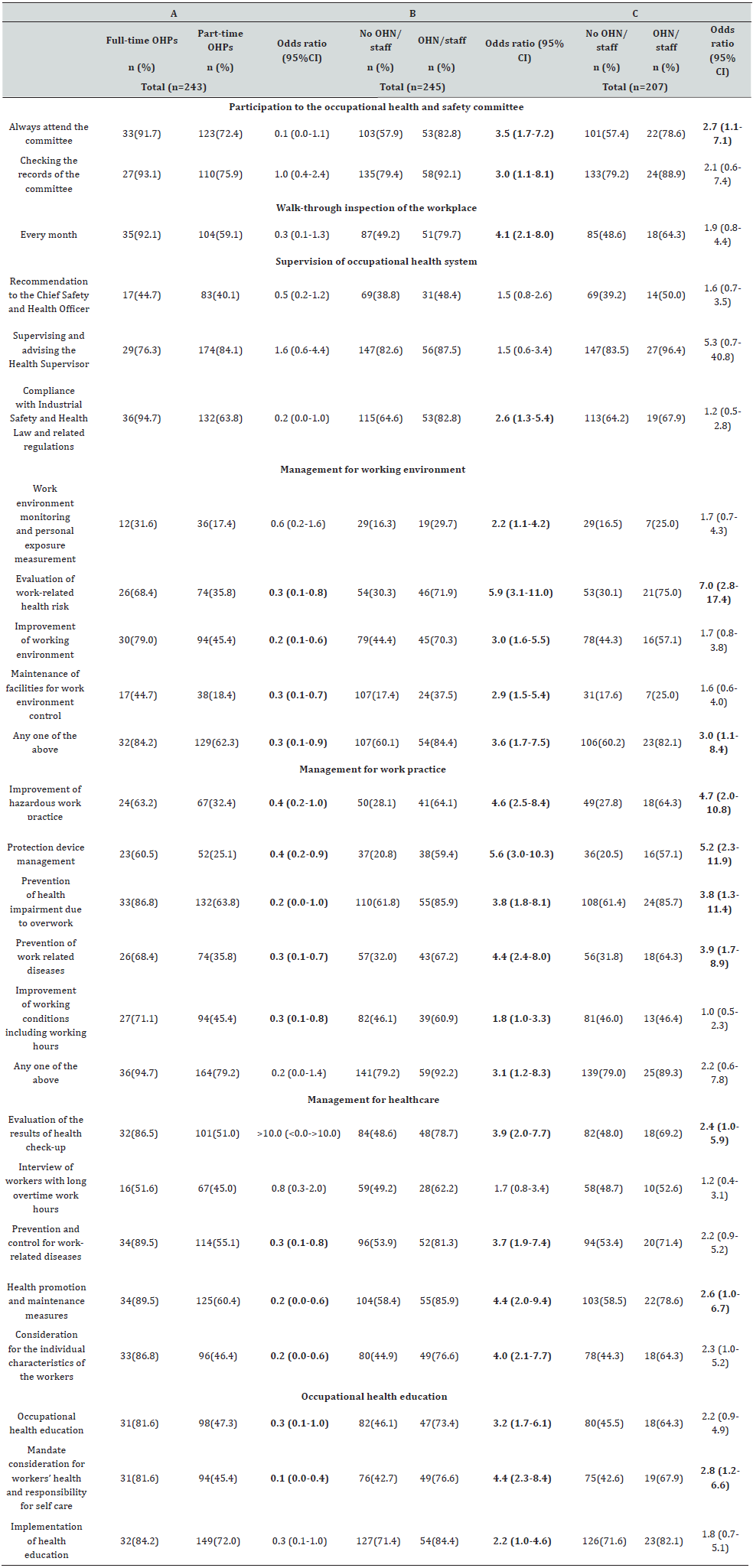
A: Comparison of the occupational health services provided by part-time and full-time OHPs.
B: Services performed by OHPs with and without assistance from occupational health nurses (OHNs)/staff.
C: Services performed by part-time OHPs with and without assistance from OHNs/staff (all adjusted for hours worked by OHPs per month) , * Odds nation were statistically significant (p<0.05).
Discussion
Table 2B shows that for certain services supported by OHNs/ staff, part-time OHPs performed as well as full-time OHPs. When we examined only the results for part-time OHPs, more OHP engagement in the workplace was seen when the OHNs/staff helped to process the health check-up data. Our results suggest that the full-time OHPs provided a higher level of service than the part-time OHPs. This difference was not due to the difference in amount of time spent in the workplace, because the data in Table 1 were adjusted for engagement time. However, some services were provided equally effectively by part-time OHPs when they were assisted by OHNs/staff (Table 2B). The effect of assistance from OHNs/staff persisted when we limited the analysis to the part-time OHPs (Table 2C). Although this study was performed on a single large company with several hundred thousand workers, we need to be cautious when generalizing the results [3]. The definition and classification of occupational health services and support from an OHNs / staff need to be specified further to obtain more reliable findings. Nevertheless, keeping these limitations in mind, we suggest that occupational health services in the workplace can be improved as follows.
For managing workplace health in Japan, the OHP is a key individual who makes plan for and delivers occupational health services, and evaluates the results to prevent work-related disease and promote workers' health. In Japan, more than 140,000 workplaces are legally required to appoint an OHP, but there are only 80,000 physicians who are certified to be an OHP, most of whom are predominantly engaged in clinical practice. The vast majority of OHPs have part-time contracts and their time in the workplace is generally limited. Therefore, to achieve better occupational health services in the workplace, OHPs must use their time in the workplace more efficiently. Our results suggest that OHNs/staff improve the performance of OHPs, which in turn improves occupational health in the workplace [4].
Acknowledgment
This study was approved by the Internal Review Board of Teikyo University.
References
- (1991) Industrial Safety and Health Law and Related Legislation of Japan Industrial Safety and Health Association Japan. Tokyo, Japan.
- Yano E (1995) Occupational Health in Japan. In: Yano E (Ed.) Environment, Health and Medical Care for the 21st Century. Harvard University Press, Cambridge, USA, pp. 190-199.
- Yano E (1999) Evidence Based Medicine in occupational health: Evaluation of the workplace health examinations in Japan. In: Yano E (Ed.) Evaluation in Medicine and Health Care. Toward Evidence Based Medicine, Nankodo, Tokyo, Japan, pp. 135-146
- WHO Regional Office for Europe (2001). The Role of the Occupational Health Nurse in Workplace Health Management. WHO Regional Office for Europe Copenhagen EUR/01/5025463.






























