Low Health Literacy: Treacherous Foe of Patient Compliance in Developed Countries
Remie Chrabieh1, Nohad Masri2, Zeina Tannous3, Hady Ghanem4 and Elie Saliba5*
1Remie Chrabieh, MD Department of Dermatology, Gilbert, and Rose Marie Chagoury school of medicine, Lebanese American University, Beirut, Lebanon, Email: remie.chrabieh@lau.edu
2Nohad Masri, MD Department of Hematology and Oncology, Lebanese American University Medical Center - Rizk Hospital, Beirut, Lebanon, Email: nohad.masri@lau.edu
3Zeina Tannous, MD Department of Dermatology, Gilbert, and Rose Marie Chagoury school of medicine, Lebanese American University, Beirut, Lebanon, Email: zeina.tannous@lau.edu.lb
4Hady Ghanem, MD Associate professor, Department of Hematology and Oncology, Lebanese American University Medical Center - Rizk Hospital, Beirut, Lebanon, Email: hady.ghanem@lau.edu.lb
5Elie Saliba, MD department of dermatology, Lebanese American University Medical Center - Rizk Hospital, Beirut, Lebanon, Email: elie.saliba01@lau.edu
Submission: April 06, 2023; Published: April 20, 2023
*Corresponding author: Elie Saliba, Department of Dermatology, Lebanese American University Medical Center, Beirut, Lebanon, USA
How to cite this article: Remie C, Nohad M, Zeina T, Hady G, Elie S. Painful Subcutaneous Nodules in A Patient with Acute Myeloid Leukemia. JOJ Int Med. 2023; 1(4): 555567. DOI:10.19080/JOJIM.2023.01.555567
Abstract
Subcutaneous sweet syndrome (SSS) is a rare variant of sweet syndrome (SS) in which the subcutaneous fat is primarily involved. Clinically, SSS is characterized by deep-seated nodules and plaques which may be erythematous and tender and affects mainly the extremities. We report a case of a 62-year-old man with acute myeloid leukemia (AML) who presented to the Emergency Department with multiple tender indurated nodules involving the trunk and thighs and was found to have AML-related SSS. Histopathologic analysis revealed predominantly lobular neutrophilic panniculitis without dermal or epidermal involvement. SSS is a diagnosis of exclusion; thus infection, erythema nodosum, leukemia cutis, and other entities presenting with neutrophilic panniculitis should be considered in the differential diagnosis. Systemic corticosteroids are the mainstay of therapy in patients with frequent relapses.
Keywords: Subcutaneous sweet syndrome; Acute myeloid leukemia; Neutrophilic panniculitis
Abbreviations: AFB: Acid-Fast Bacilli; SSS: Subcutaneous Sweet Syndrome; ESR: Erythrocyte Sedimentation Rate; AML: Acute Myeloid Leukemia; MDS: Myelodysplastic Syndrome; SS: Sweet Syndrome
Introduction
Neutrophilic panniculitis denotes inflammation of the subcutaneous fat involving primarily neutrophils [1]. Clinically, almost all panniculitides are present as vague, erythematous deep-seated nodules and a careful histopathological examination is required for appropriate diagnosis. Subcutaneous Sweet Syndrome is diagnosed according to pertinent clinical and histologic results and after ruling out other major causes of neutrophilic panniculitis such as leukemia cutis, erythema nodosum and infectious panniculitis. We herein report a case of acute myeloid leukemia related subcutaneous sweet syndrome that responded to systemic steroids.
Case Report
A 62-year-old man initially presented with the incidental finding of pancytopenia on routine laboratory tests. Bone marrow aspirate and biopsy studies revealed acute myeloid leukemia with 64% blasts. He started induction chemotherapy with Cytarabine and Idarubicin. He then presented to the Emergency Department with multiple tender indurated nodules involving the trunk and thighs. There was no previous personal or family history of skin diseases. His hospital course was complicated by neutropenic fever for which he received several antibiotic courses with no improvement in his skin lesions that persisted, spontaneously appearing, and resolving since his AML diagnosis. Physical examination showed deep tender subcutaneous nodules with overlying non-scale ill-defined erythema present over the right lateral inferior chest and right medial thigh (Figure 1).
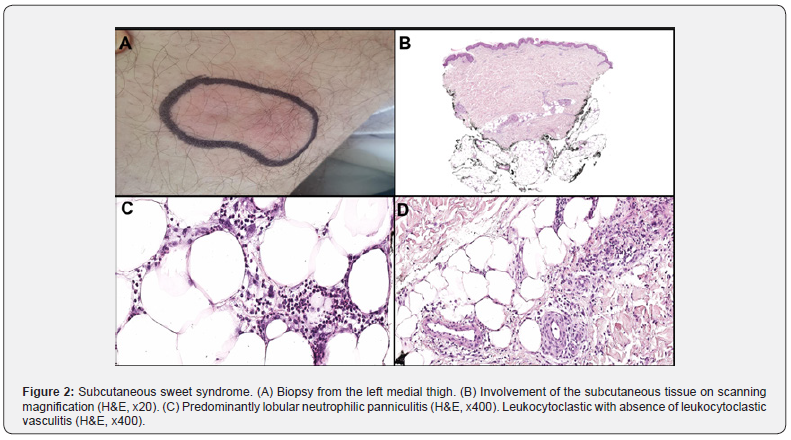
Histological examination from the left medial thigh punch biopsy revealed predominantly lobular neutrophilic panniculitis without dermal infiltrate, papillary dermal edema, or vasculitis. No myeloid blasts were identified on hematoxylin-eosin stain, or on CD117 or CD34 immunotoxins (Figure 2). Periodic Acid-Schiff, Acid-Fast Bacillus and Gram stains were negative for microorganisms. Tissue and blood cultures produced negative findings. A diagnosis of subcutaneous sweet syndrome was made. Treatment with systemic corticosteroids along with systemic chemotherapy for the underlying leukemia resulted in rapid clinical response with no relapse at last follow-up.
Discussion
Myeloid disorders such as myelodysplastic syndrome (MDS) and acute myeloid leukemia (AML) are known to be associated with neutrophilic dermatosis [2]. Sweet syndrome is the prototype of neutrophilic dermatosis and is typically accompanied by fever, neutrophilia, and increased erythrocyte sedimentation rate (ESR) [3]. However, neutrophilic panniculitis has rarely been described in association with myeloid disorders [4]. Subcutaneous sweet syndrome (SSS) is a rare variant in which the subcutaneous fat is primarily involved.

The male-to female ratio is 4:5 with a median age of onset of 56 years [1,4]. Clinically, patients are present with deep-seated tender nodules and erythematous plaques involving mainly the extremities [1,4]. Additionally, skin lesions are frequently accompanied by systemic symptoms, including fever and malaise.
The etiology of SSS is complex as it might be idiopathic or associated with hematologic malignancies, drugs, or other conditions [5]. The most common diseases associated implicated with SSS are acute myelogenous leukemia, multiple myeloma, breast carcinoma, salmonella enteritidis infection and myelodysplastic syndromes [6].
The most common histopathologic pattern in SSS is that of neutrophilic lobular panniculitis with absence of vasculitis [5,6]. Nuclear hyper segmentation or hypo segmentation of neutrophils may be seen in cases associated with myeloid disorders. This phenomenon is considered evidence of continued dysgranulopoiesis secondary to the underlying myeloid disorder [6,7]. Additional findings include mild edema in the reticular dermis, and mild perivascular inflammation. However, papillary dermal edema which is found in classic sweet syndrome is typically mild [8,9].
The histologic differential diagnosis is broad and includes infective panniculitis, erythema nodosum, pancreatic panniculitis, alpha-1-antitrypsin deficiency, drug related neutrophilic panniculitis and leukemia cutis. Tissue cultures for bacteria, fungi, and mycobacteria should be performed when infectious panniculitis is considered and histology also reveals abscesses, granuloma formation and vasculitis. Additionally, in most situations special stains such as periodic acid Schiff (PAS), gram and acidfast bacilli (AFB) are necessary [8,9]. In panniculitis id reaction, an infection at a distant site is identified and leukocytoclastic and granulomatous vasculitis are also seen in histology. Erythema nodosum represents the prototype of septal panniculitis. It is characterized by a combination of findings including vascular change, septal inflammation, hemorrhage, and variable degree of acute or chronic inflammation with Miescher radial granulomas [8,9]. Pancreatic panniculitis is characterized by enzymatic fat necrosis with ghost adipocytes and occasional calcification of the fat tissue [10]. The changes in alpha1-antitrypsin deficiency are those of “free-floating” fat with splaying of neutrophils between collagen bundles of the deep reticular dermis [11]. Neutrophilic drug-related panniculitis is suspected in the setting of BRAF and Tyrosine kinase inhibitors10. Leukemia cutis is diagnosed by identifying leukemic cells with CD34 and CD117 immunotoxins in histology [12]. Finally, rheumatoid arthritis panniculitis and Behçet disease should be considered in the appropriate clinical setting [10]. Systemic corticosteroids are the mainstay of therapy and lead to complete resolution of symptoms within a short period of time [5,8,9]. Dapsone was used successfully in one case while several reported cases resolved spontaneously without treatment [3,11,12].
The relationship between neutrophilic dermatoses and myeloid disorders is well established, but neutrophilic panniculitis in the same setting has rarely been described. To our knowledge, this is the seventh reported case of SSS associated with AML [7]. All patients were presented with many erythematous subcutaneous nodules and some of them had fever. White blood cell counts, or blast did not show a relationship with the presence of the nodules. The most common location of the lesions was the lower extremities with or without simultaneous upper extremity association as in our patient. None of the reported cases included had additional factors that predispose to neutrophilic panniculitis. Our patient is approximately sixth months post bone marrow transplantation and developed cutaneous graft versus host disease but continues to be in remission. The course of his rash is like the cases published in the literature where resolution was achieved spontaneously or by administration of systemic prednisone [7]. We herein highlight a rare case of acute myeloid leukemia related subcutaneous sweet syndrome that should be included in the differential diagnosis of neutrophilic panniculitis.
References
- Chan MP (2014) Neutrophilic Panniculitis Algorithmic Approach to a Heterogeneous Group of Disorders. Archives of Pathology & Laboratory Medicine 138(10): 1337-1343.
- Cohen PR, Kurzrock R (2003) Sweet’s syndrome revisited: a review of disease concepts. Int J Dermatol 42(10): 761-768.
- Cooper PH, Frierson HF, Greer KE (1983) Subcutaneous neutrophilic infiltrations in acute febrile neutrophilic dermatosis. Arch Dermatol 119(7): 610-611.
- Guhl G, García-Díez A (2008) Subcutaneous Sweet Syndrome. Dermatologic Clinics 26(4): 541-551.
- Morioka M, Otsuka F, Nogita T, Igisu K, Urabe A, et al. (1990) Neutrophilic dermatosis with myelodysplastic syndrome: nuclear segmentation anomalies of neutrophils in the skin lesion and in peripheral blood. J Am Acad Dermatol 23(2): 247-249
- Becherer K, Golda N, Feldman M, Diaz-Arias A, Caldwell C, et al. (2009) Neutrophilic panniculitis associated with myelodysplastic syndrome with abnormal nuclear forms. J Cutan Pathol 36(9): 1024-1026.
- Chan MP, Duncan LM, Nazarian RM (2013) Subcutaneous Sweet syndrome in the setting of myeloid disorders: A case series and review of the literature. J Am Acad Dermatol 36(6): 1006-1015.
- Cullity J, Maguire B, Gebauer K (1991) Sweet’s panniculitis. Australas J Dermatol 32(2): 61-64.
- Matsumura Y, Tanabe H, Wada Y, Ohta K, Okamoto H (1997) Imamura S Neutrophilic panniculitis associated with myelodysplastic syndromes. Br J Dermatol 136(1): 142-144.
- Llamas-Velasco M, Fraga J, Sánchez-Schmidt JM (2020) Neutrophilic Infiltrates in Panniculitis: Comprehensive Review and Diagnostic Algorithm Proposal. Am J Dermatopathol 42(10): 717-730.
- Vignon Pennamen MD, Wallach D (1991) Cutaneous manifestations of neutrophilic disease. A study of seven cases. Dermatologica 183(4): 255-264.
- Carvalho P, Cordel N, Courville PH (2001) Cutaneous aseptic abscesses, manifestations of neutrophilic diseases. Ann Dermatol Venereol 128(5): 641-643.






























