Brucellosis Associated with Acute Cholecystitis
Ugur Ergun1*, Ömer Faruk Turan1, Burak Alp1, Merve Nur Ak1 and Sena Yılmaz2
1Department of Medicine, Division of Internal Medicine, Balikesir University School of Medicine, Turkey
2Department of Medicine, Division of Radiology, Balıkesir University School of Medicine, Turkey
Submission: August 25, 2019; Published: September 30, 2019
*Corresponding author: Ugur Ergun, Department of Medicine, Division of Internal Medicine, Balıkesir University School of Medicine, Cagis Yerleskesi, Balıkesir, 10145, Turkey
How to cite this article: Ugur Ergun, Ömer Faruk Turan, Burak Alp, Merve Nur Ak, Sena Yılmaz. Brucellosis Associated with Acute Cholecystitis. JOJ Int Med. 2019; 1(2): 555559.
Abstract
Brucellosis is the most common zoonotic infection around the world that is caused by direct contact or consumption of infected animals meat or products. It is a multisystemic disease with a wide range of clinical symptoms. The disease may present with broad spectrum manifestations and involves many systems. Other less frequent complications include intraabdominal abscesses, appendicitis, ileitis, colitis and cholecystitis. Acute cholecystitis is a very rare presentation of brucellosis. Here we report case of a 61 year-old male with acute cholecystitis caused by B. Melitensis.
Keywords: Brucella cholecystitis fever chronic infectious bacterial disease brucellosis infection
Abbrevations: STA: Standard tube agglutination; US: Ultrasound
Introduction
Brucellosis is a chronic infectious bacterial disease affecting various species of domestic and wild animals, as well as humans [1]. It is a zoonosis of a greatly varied clinical image, caused by small, aerobic, Gram-negative rods of the genus Brucella [2]. Brucella disease is endemic in many parts of the world. It is most prevalent in the countries which do not possess adequate standards developed in the area of public health and protection of animal health. The areas at high risk of brucellosis infection are the countries of the Mediterranean Sea Basin also countries of South and Central America, Asia and Africa. In humans, the disease may cause many symptoms varying from mild flu-like to severe complications on the part of the gastrointestinal system, nervous system, musculoskeletal system and the heart [3]. Cholecystitis is a rare complication of brucellosis. In this report, a patient who presented with a classical picture of acute cholecystitis and from whom Brucella was deteced from standard tube agglutination test (STA) is reported.
Case Report
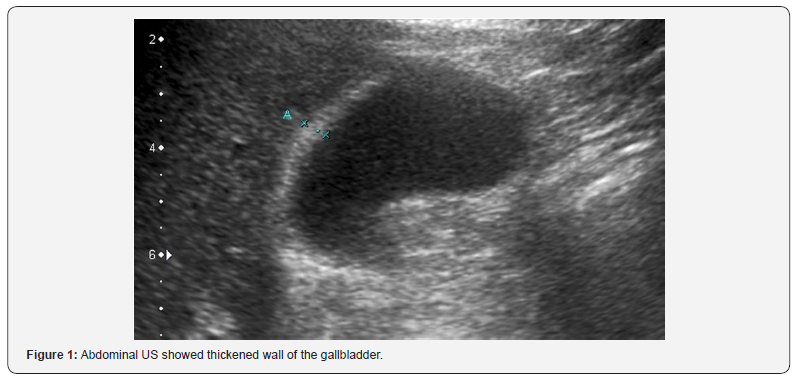
A 61-year-old male was admitted to the hospital with fever, abdominal pain and a 2 week history of weight loss of 10 kilogram. There was no history of trauma, vomiting, diarrhoea, and no family history of inflammatory disease. The abdominal pain started in the epigastric area and became localized to the right upper quadrant area for almost 1 month. Patient’s anamnesis was presenting history of type 2 diabetes mellitus and hypertension. On physical examination, his temperature was 38.80C, pulse rate was 112 beats/minute and respiratory rate was 22/minute. Abdominal examination showed tender right upper quadrant area and a positive Murphy’s sign. Laboratory data at the time of admission were as follows: hemogloubin 11.7 g/dL, leukocyte count 4.7x109/L, platelets 189x109/L, alanine aminotrasferase: 76 IU/L, aspartate aminotransferase: 90 IU/L, gama glutamyl transferase: 231 IU/L, alkaline phosphatase: 243 IU/L, total bilirubin: 109 μmol/L, direkt bilirubin: 46 μmol/L, amilaz: 32 IU/L, C reactive protein of 161 mg/L (0-3.2 mg/L), erythrocyte sedimentation rate of 88 mm/h (0-20 mm/h). The patient’s viral hepatitis serology was negative. Ultrasound (US) scan showed a thickened gallbladder wall with no evidence of stones (Figure 1). The patient was therefore managed as a case of acute cholecystitis. After blood cultures were obtained, intravenous seftriakson 2g and metronidazol 1g was commenced. On day 14 after admission, one blood culture was positive. It grew small colonies of Gram-negative bacili that were later identified as B. Melitensis. STA was 1/5120 respectively. The patient was treated with a combination of doxycycline 200 mg twice daily for six weeks and gentamycin 80 mg IV for a 1 week. He remained asymptomatic during a six week follow-up period with no evidence of relapse.
Discussion
Brucellosis is a zoonosis widely distributed around the world. In humans, brucellosis behaves as a systemic infection with a very heterogeneous clinical spectrum. The clinical features of brucellosis are not disease specific; almost every organ can be affected. The prevalence and pattern of complications depend on the strain of Brucella infecting the individual and the duration of the disease [4]. Focal forms of brucellosis are present in approximately 30% of patients. The most common gastrointestinal complication is reactive hepatitis with or without granulomas. Other less frequent complications peritonitis, intraabdominal abscesses, ileitis, colitis, pancreatitis and appendicitis. Case of acute cholecystitis occurring as a complication of brucellosis are rare [5-7]. As in our case, most reported cases are due to B. Melitensis and describe acalculous cholecystitis. All the patients had clinical symptoms of acute cholecystitis and had history of fever weeks prior to admission [8]. In our patient had acute cholecystitis clinic, brucellosis was not suspected at the time of admission. The diagnosis was reached only after blood culture were performed due to the patient’s fever. The result was confirmed by standard tube agglutination test. The most commonly used antibiotic combination was doxycycline-streptomycin or gentamycin. The duration of therapy ranged from one week to six months. All patients are observed clinical improvement. Brucella species are usually associated with bacteremia and systemic infection. They are intracellular and may cause latent infection with subsequent clinical symptoms years after their onset. Involvement of the gallbladder in such systemic infections may ocur via the lymphatic spread or as part of bacteremia [8]. In this case report, it is not clear whether acute cholecystitis brucellosis in our patient is a chronic latent infection complication or localized acute brucellosis.
In conclusion, brucellosis is a systemic infection in which any organ or system of the body can be involved. It should be considered in the differential diagnosis of acute cholecystitis in regions where brucellosis is an endemic disease.
Conflict of Interest
The authors declare that they have no conflict of interest
References
- Al Dahouk S, Tomaso H, Nockler K, Neubauer H, Frangoulidis D (2003) Laboratory-based diagnosis of brucellosis-a review of the literature. Part II: serological tests for brucellosis. Clin Lab 49(11-12): 577-589.
- (1996) Dziubek Z Bruceloza w: Dziubek Z. (red.): Infectious and parasitic diseases. PZWL Warszawa 137-139.
- Łapiński TW, Wierzbicka I, Prokopowicz D, Kot A (2001) Brucellosis in humans -new risk. 57(11): 800-802.
- Al-Nasir W, Lingaris MV
- Cervantes F, Bruguera M, Carbonell J, Force L, Webb S (1982) Liver disease in brucellosus: A clinical and pathological study of 40 cases. Postgrad Med J 58(680): 346-350.
- Williams RK, Crossley K (1982) Acute and chronic hepatic involvement of brucellosis. Gastroenterology 83(2): 455-458.
- Orte L, Teruel JL, Bellas C, Traver JA, Sanz-Guajardo D, et.al. (1979) Brucellosis of the kidney: description of three cases. Rev Clin Esp 152: 461-464.






























