Giant Cumulated Condyloma: Tumor of Buschke Lõwenstein
Juan Francisco Rodríguez Reyes1, Jorge Agustin Satorre Rocha1, Pedro Rolando López Rodríguez1,3*, José Antonio Hernández Varea2 and Olga Caridad Leòn Gonzalez1
1Department of General Surgery, Auxiliary Researcher General Teaching Hospital, Cuba
2Department of Surgery, Cuba
3Consultant Professor in Surgery, Cuba
Submission: June 26, 2019; Published: August 21, 2019
*Corresponding author: Pedro Rolando López Rodríguez, Consultant Professor In Surgery, Auxiliary Researcher General Teaching Hospital, Havana Cuba
How to cite this article: GJuan F R R, Jorge A S R, Pedro R L R, José A H V, Olga C L G. Giant Cumulated Condyloma: Tumor of Buschke Lõwenstein. JOJ Int Med. 2019; 1(2): 555557.
Abstract
The condylomata acuminata or genital warts are produced by the human papillomavirus. Infection typically occurs when host basal cells are exposed to viral infection through a damaged epithelial barrier, such as during sexual intercourse or as a product of other minor skin abrasions. In few occasions they can evolve with a marked growth and cause the well-known Buschke-Löwenstein syndrome or Giant Condiloma Acuminado. We present a patient with Giant Condyloma Accumulated in the inguinal and anal regions that was surgically treated with exeresis of the inguinal lesions and electrofulguration of the annals with satisfactory evolution, without tumor recurrence at three months.
Keywords: Giant condiloma accuminado Warty carcinoma Papillomavirus Electrofulguration Giant condiloma Sexually transmitted diseases
Introduction
Condylomata acuminata or genital warts are one of the most common sexually transmitted diseases. They are produced by the human papillomavirus. Infection typically occurs when host basal cells are exposed to viral infection through a damaged epithelial barrier, such as during sexual intercourse or as a product of other minor skin abrasions [1,2]. The presence of other associated factors is necessary to produce the disease such as: sexual promiscuity, poor nutrition, smoking, depression of the immune system and prolonged use of oral contraceptives [1-4]. On rare occasions they can evolve as an invasive tumor with local malignancy, although without metastasis, equivalent to a verrucous carcinoma and it is when they are diagnosed as Buschke-Löwenstein syndrome or tumor.
Presentation of the Case

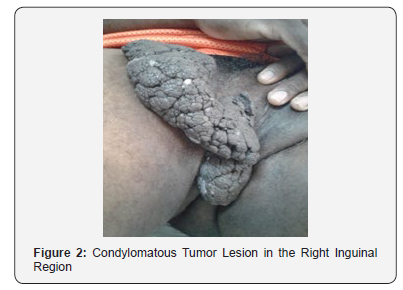
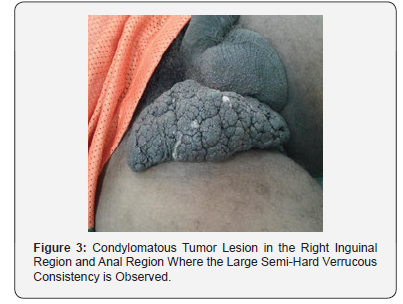
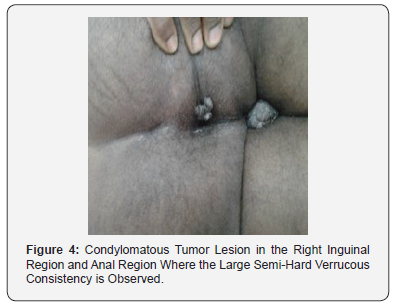
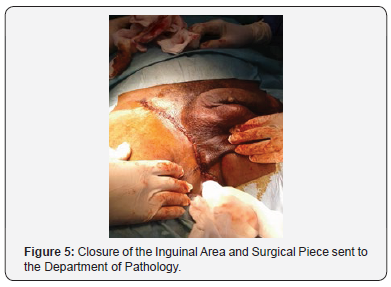
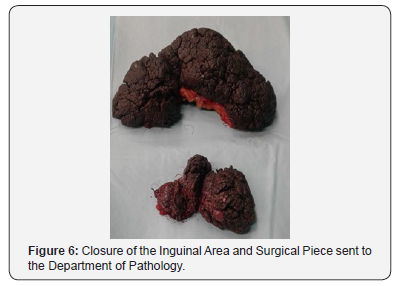
Male patient I.K.M. 47 years old, Bahamés, who attended the surgery clinic of the Central Clinic “Cira García” for presenting skin lesions in the inguinal and anal region of 5 years of evolution that have been growing progressively. It started as a “little ball” until it reached the size of a tumor lesion approximately 20 cms. high, of semi-hard consistency. Therefore, their admission is decided for study and surgical treatment. Upon entry. Physical examination: verrucous lesion of exophytic growth located in the scrotum and perineum of 10 cm in diameter, without presence of suppuration or signs of ulceration (Figure 1) and another verrucous lesion in right inguinal region, pedunculated approximately 20x15cm in diameter. 5 years of evolution. Hematological and serological check was carried out: Hemoglobin 13.5g/l, Hto. 0.45 leukogram 7.5x10/l Erythro 18, blood glucose 5.54mml, Cituria Negative, HIV negative, Serology, non-reactive, platelet count 321x10g/l. Thorax Rx Normal. Normal nasal and pharyngeal exudate. Rectosigmoidoscopy: No internal injury, no anal canal involvement was observed. He underwent a complete excision of the lesion of the inguinal region and electro-fulguration of the perianal lesion. It was not necessary to perform the plastic reconstruction given the pedunculated characteristic of the inguinal lesion that was completely resected (Figures 2-6).
Histological Study
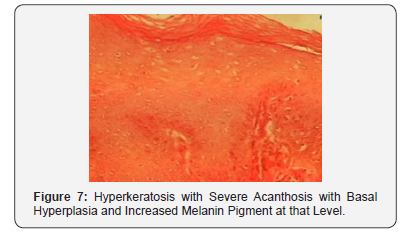
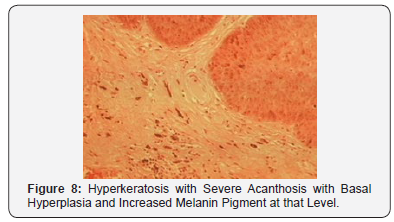
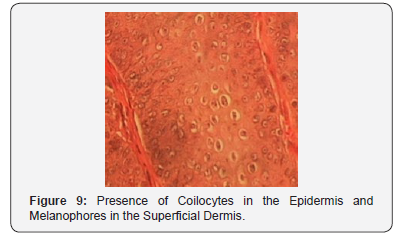
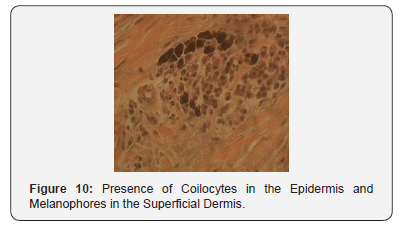
Histologically (Figures 7-10) there was marked hyperkeratosis and acanthosis and areas of parakeratosis with moderate spongiosis and areas of basal hyperplasia with increased melanin pigment in the basal cells with malignant cells and nucleoli prominent rosés with inclusion bodies in the epidermis. Severe papillomatosis with increased vascularizationand the presence of giant cells of the foreign body type with the presence of melanoforos and chronic inflammatory infiltrate in the superficial and middle dermis. The diagnosis was concluded as a giant Condilomatosis or Buschke-Lowenstein tumor. The patient progressed satisfactorily and remains in follow-up by Surgery. There have been no recurrences after three months of surgery.
Discussion
The Buschke-Lowenstein tumor is a rare variant genital condyloma associated with infection by HPV strains 6 and 11. The average age of presentation is under 50 years, with a predominance of men in a 3:1 ratio. It is a pre-malignant lesion, considered anatomopathologically between condyloma acuminatum and perianal squamous cell carcinoma, which explains its high morbidity and mortality. It is characteristically bulky (more than 10cm in diameter) and slow-growing and exophytic with a tendency to invade and destroy the tissues on which it sits [5,6]. Among the risk factors that predispose to suffer from this pathology we can find: immuno suppression (mostly with HIV positive), homosexuality, promiscuity, poor genital hygiene, chronic genital infections, malnutrition and alcoholism. Freed to its free evolution, this tumor can spread intraanally, fistulize, become infected, recur once it is operated (66%) or undergo malignant transformation (56%) [7,8]. The Buschke-Lowenstein tumor does not present cellular atypia, it is a benign tumor, but in 30% of cases it can be malignant; nevertheless, due to the great power it has of recurrence, it is considered by some authors as a malignant tumor [9,10]. The differential diagnosis of Buschke-Lowenstein tumor will be made with other pathologies of genital location among them: Bowen’s disease in its condylomatous form, pseudo-epitheliomatous balanitis caused by fungi, spinocellular epitheliomas, warty carcinomas, syphilis, lymphogranulomatosis venereum (Nicolás disease) Favre).
The difference of the giant acuminate condyloma is that it is more proliferating and penetrates deeper tissues than squamous cell tumors, respects the basement membrane and does not metastasize. Of the rest of the pathologies raised is discarded by serology and other complementary. [8,11,12]. Regarding treatment, the most appropriate option is the radical surgical excision of the lesions and their anatomopathological study. Some cases may even require abdomino-perineal amputation. Other treatments that have been used in some cases are chemo and radiotherapy, as well as topical treatments although the available bibliographic evidence is not conclusive regarding the systematic use of them, tending in general terms to be ineffective. [12-14].
Conclusion
a. Definitive diagnosis: Tumor of Buschke Lõwenstein or Condiloma Accuminado Gigante.
b. Surgical treatment: Excision of inguinal lesions and electrofulguration of anal lesions.
c. Evolution: Satisfactory: There have been no recurrences in the assessmen
References
- Gearhart PA, Randall TC, Buckley RM (2006) Human Papillomavirus.
- Quyen D Chu, Michael P Vezeridis, Peter Libbey N, Harold J Wanebo (1994) Giant Condyloma Acuminatum (Buschke-Lowenstein Tumor) of the Anorectal and Perianal Regions. Analysis of 42 Cases. Dis Colon Rectum 37(9): 950-951.
- Sukru Tas, Muhammet Kasim Arik, Faruk Ozkul, Oztekin Cikman, Yilmaz Akgun (2012) Perianal Giant Condyloma Acuminatum-Buschke-Lowenstein-Tumor: A Case Report. Case Reports in Surgery 1-3.
- W Gardner Rhea, Brian M Bourgeois, Daniel R Sewell (2017) Condyloma acuminata: a fatal disease? Am Surg 64(11): 1082-1087.
- Ruiz de la Hermosa A, Hurtado Caballero E, Zorrilla Ortúzar J, Del Valle Hernández E, Muñoz Jimenez F (2011) Caso clínico:Tumor de Buschke-Lowenstein asociado a condilomatosis nasofarí Revista de Gastroenterología de México 76(3): 275-278.
- Alexander Kreuter, Ulrike Wieland (2011) Giant Condyloma Acuminatum of Buschke and Lö Case Report. The New England Journal of Medicine 365(17): 1624.
- Rodríguez González D, Pérez Piñero J, Sarduy Nápoles M (2014) Infección por el virus del papiloma humano en mujeres de edad mediana y factores asociados. Rev Cubana Obstet Ginecol 40(2): 218-232.
- Genaro Vega-Malagón, Javier Ávila-Morales, Pablo García-Solís, Nicolás Camacho-Calderón, Alma Becerril-Santos, et al. (2017) Infección por el virus del papiloma humano. biología molecular European Scientic Journal 10(18): 352-362.
- Pennacchiotti G, Sáez R, Martínez MJ, Cárcamo M, Montes R, et al. (2016) Prevalencia del virus papiloma humano en pacientes con diagnóstico de carcinoma escamoso de la cavidad oral. Rev Chil Cir 68(2): 137-142.
- Fernández Isai Arturo Medina, Ruth Magdalena Gallegos-Torres, María Eugenia Cervera-Baas, Rudy Antonio Cob-Tejeda, Jenny Jiménez-Laces, et al. (2017) Conocimiento del virus del papiloma humano y su vacuna por parte de mujeres de una zona rural de Querétaro, Mé Revista Enfermería Costa Rica 22(1): 1-14.
- García Lia Barrios, Patóloga, Paola Andrea Lecompte Osorio, Rodolfo Alberto Leones Castillo, Francisco Rafael López Custode, et al. (2016) Factores de riesgo presentes en pacientes con lesiones intraepiteliales escamosas del cérvix en la Clínica Maternidad Rafael Calvo en la ciudad de Cartagena (Colombia): estudio descriptivo. Artículo de Investigación 16(1): 109-117.
- Morales L Liliana A, Rincón R Diego F, Rincón Orozco Bladimiro (2016) Avances en el desarrollo de nuevas vacunas profilácticas y terapéuticas contra el Virus del Papiloma Humano. Rev Univ Ind Santander 48(3): 385-391.
- Pinto Bustamante Boris Julian (2016) La vacuna contra el Virus del Papiloma Humano: estado de la cuestión, principio de proporcionalidad y consentimiento informado. Acta bioeth 22(2): 251-261.
- González Martínez G, Núñez Troconis J (2015) Tratamiento de las verrugas genitales: una actualizació Rev Chil Obstet Ginecol 80(1): 76-83.






























