Malaria Data Analysis in Menge District, Assa zone, Benishangul Gumuz,Ethiopia, 2017
Seid Ali Mohammed* and Yaregal Animut
College of Medicine and Health Science, Institute of public Health,Department of Biostatistics and Epidemiology,University of Gondar,Ethiopian
Submission: June 20, 2019; Published: July 03, 2019
*Corresponding author: Seid Ali Mohammad, college of medicine and health science, Institute of public health,Department of Biostatistics and Epidemiology, University of Gondar, Ethiopian
How to cite this article: Seid Ali Md, Yaregal A. Malaria Data Analysis in Menge District, Assa zone, Benishangul Gumuz,Ethiopia, 2017. JOJ Int Med. 2019; 1(1): 555555.
Abstract
Background: Malaria is a protozoan disease caused by plasmodium species. Malaria remains to be a serious public health problem causing very large mortality, and morbidity. It is also one of the major challenges to socio-economic development leading to poverty. Malaria transmission is largely unstable in Ethiopia and all age groups are at risk of malaria. Ongoing malaria surveillance data analysis is useful for assessing incidence and Monitoring disease trends over time and evaluating the effectiveness of disease control programs. The aim of this surveillance data analyze was to assess the magnitude and trend of malaria in the district to proposed possible recommendations useful for control and Prevention activities.
Methods: Descriptive cross-sectional study was conducted in Menge Woreda. The data on malaria indicators were collected from Public Health Emergency Management core process (PHEM) database from May 25 to June 30/2017. The four years malaria data was collected; organized; processed and analyses by using Microsoft excel 2010.
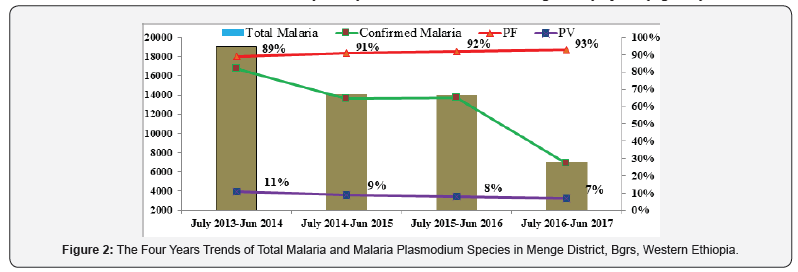
Results: A total 54197 malaria cases and 7 deaths were reported from July 2013-june 2017. An average malaria cases reported to PHEM per year were 13605; it ranges from 19085 in 2013/2014 to 7043 in 2016/2017. During the same period; average total malaria prevalence rate of the district was 265 per 1000 population. The four years period the Annual parasitic index (API) of malaria was decreased from 341 to 125per 1000 population. Clinical malaria treatment rate was decreased from 19%in 2013/2014 to 2.70% in2016/2017.The four years proportion of plasmodium falciparum and Vivax were 91:9respectivly. The incidence of both malaria inpatients and malaria case fatality rate were increase with inconsistent trend, both were decreased from July 2013-june 2016 and both were increased in July 2016- June 2017.
Conclusion: Even though different malaria control strategies were designed to roll back to its minimum level, still malaria cases were not decreased as expected level. Malaria continued to be a major cause of health problem in Menge woreda. Malaria inpatient and CFR were increased with inconsistence trend. Therefore, the district health office should strength malaria prevention and control activity.
Limitations data: The poor handling of data by kebele; it is difficult to know the trend of dominance parasite species at kebele level. There was no aggregated data by sex and age at PHEM data base. The documented data were not in the form of electronic database, it needs more time to compile and analysis disease trend easily.
Keywords: Surveillance Data analysis Malaria Menge district Benishangul gumuz region
Introduction
Backgrounds
Malaria is a protozoan disease caused by plasmodium species. The five Plasmodium species (Plasmodium falciparum, P. Vivax, P. ovale, P. malaria, P. Knowlesi) were recognized as the only etiological agents of human malaria. Plasmodium falciparum is found in most tropical regions throughout the world and is the most dangerous of the five in terms of both its lethality and morbidity [1]. All undergo two forms of replication: sexual and asexual. The parasites mature in the vector but cease developing at temperatures 16 °C or below. High humidity prolongs the life of the vector and transmission is extended under these conditions [2]. Malaria is one of the most severe public health problems in the world, which kills approximately 429000 people and causes disease for 212million people annually. In most endemic area of the world, pregnant women and under five children are more susceptible to malaria. According to world health organization 2015 report, an estimated 303000 under-fives children killed by malaria worldwide [3,4]. Malaria is a leading cause of disease and death in many developing countries. Sub-Saharan Africa carries the bulk of the global malaria burden, with 90% of cases and 92% of global deaths. Over 800 million people in 47 malaria endemic countries of Africa are at risk of infection with malarias. a person in Africa dies of malaria every 10 second [3,5]. It is also a major socio-economic problem for Africa. In high endemic countries of Africa malaria has been estimated to account for an average annual reduction of 1.3% in economic growth
Malaria endemic countries are known to have lower economic growth [6]. Ethiopia is one of the few countries with unstable malaria transmission. Consequently, malaria Epidemics are serious public health emergencies. Approximately 58 million people (68%) live in malaria endemic areas, mainly at altitudes below 2,000 meters. The main malaria parasites are Plasmodium falciparum and Plasmodium Vivax, accounting for 60% and 40% of all cases, respectively. Anopheles arabiensis is the main vector; Anopheles Pharoensis is also widely distributed in the country and is considered to play a secondary role in Malaria transmission [7]. Malaria transmission varies among communities due to environmental factors, such as proximity to breeding sites, temperature, rainfall and humidity. Water resources development and management projects can also attribute for malaria transmission by increasing the number of breeding sites, by extending breeding season and longevity of mosquitoes [2]. In Ethiopia Major malaria transmission happened from September to December following the main rainy season from June to August and minor malaria transmission happened from April to May, following a short rainy season from February to March, which is called Bimodal type transmission [8]. In Benishangul Gumuz Region, Malaria has been reported as one of the leading causes of morbidity and mortality. Approximately 99percent of people live in malaria-endemic areas of the region. Plasmodium falciparum and Plasmodium Vivax are also the two dominant malaria species in the Region. Plasmodium falciparum accounts 78% reported malaria cases of the region between July 2013-June 2017 [9].
Public health surveillance plays great important roles in reduction of morbidity and mortality of Malaria by ongoing, systematic collection, analysis, interpretation and dissemination of data regarding to health-related event for use in effective and efficient Decision-making purpose in Public health action to enhance the sustainable development of the country. Continuous analysis of surveillance data is important for detecting outbreaks and unexpected increases or decreases in disease occurrence, monitoring disease trends, and evaluating the effectiveness of disease control programs and policies [10]. The main source of information for malaria surveillance in the control phase is reports of Confirmed malaria cases, malaria inpatients and malaria deaths obtained from all or selected public sector health facilities. This Malaria surveillance data analysis is useful for assessing the general trend of Malaria morbidity and mortality by place, person and Time in the district.
Rationale of the Study
Malaria is one of the epidemic prone diseases tracked by PHEM surveillance system. The district is one of high malaria endemic area of the region and experienced a high rate of outpatient consultation from June 2013- July 2017. This data analysis will to know the epidemiology and Trend of Malaria in the district and to evaluating the effectiveness of malaria prevention and control activities to improve the future interventions against the disease
Objectives
General Objectives
To assess four years Malaria morbidity and mortality trend by person, place and time in Menge district, Asossa zone, Benishangul Gumuz Region, Western Ethiopia, June 2017.
Specific Objectives
a. To assess four years malaria morbidity and mortality trends by persons.
b. To assess four years malaria morbidity and mortality trends by time.
c. To assess the four years magnitude of malaria trends by place from July 2013-june2017.
Materials and Method
Study Area
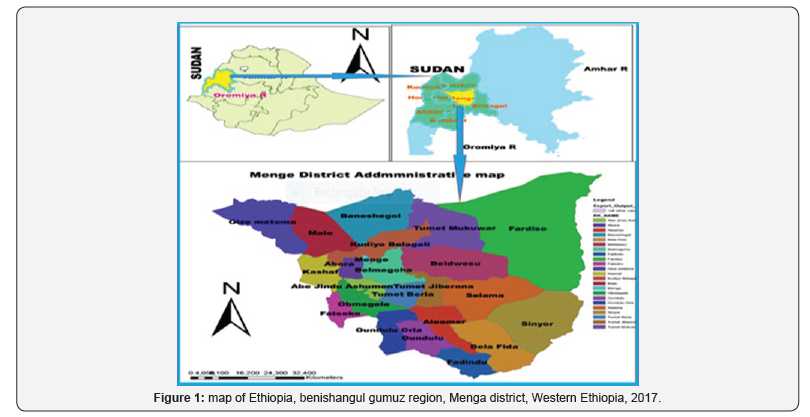
Menge district is one of the 20 districts found in Benishangul Gumuz Regional stat of west Ethiopia. It is located 703Km from Addis Ababa and 58Km far from Asossa town. It is bordered with Asossa district in south west, Sherkole in the North, kamahi zone in North East and Oda Buldiglu district in the east. It is found at an altitude 1550-1570 Meter above sea level. The district Contains 23 rural and 1 urban kebele. Based on 2016/2017 population projection the estimated population of the district was 54683; from which 26795(49%) were men. 93%of the population were rural dwellers. Based on the physical health facility counting the potential health service coverage of the district was 91.7%. The average annual temperature of the district was 20.28 co and average rainfall ranges 39.5 to 163 mm/year. It has two climatic zones; ‘Kola’ encompasses 90%; ‘Weinadega’ encompasses 10% (Figure 1).
Study Design and Period
Descriptive retrospective cross-sectional studies were used to assess four years malaria data of Menge district. The study was conducted from May 25 to June 30/2017.
Study Population
Four years (july2013-june2017) malaria suspected and confirmed patients, inpatients and deaths with different malaria species were reported in weakly PHEM surveillance report.
Case Definitions
Suspected case: -Any person with fever or fever with headache, back pain, chills, rigor, sweating, muscle pain, nausea and vomiting diagnosed clinically as malaria.
a. Confirmed Case: suspected case confirmed by rapid diagnosis test or microscopy for plasmodium parasites.
b. Presumed Malaria (Clinical Malaria): Suspected malaria case without confirmatory test for malaria clinician diagnosed as malaria
c. Populations’ High Risk for Malaria: Are those people living in areas where the number of reported cases is ≥1 per 1000 per year.
d. Populations Low Risk for Malaria: Are those living in areas with <1 case of malaria per 1000 per year.
e. Malaria Action Threshold Level: Malaria cases crossing the norm line or doubling of cases compared to the same week of the previous year.
f. Malaria Epidemic Threshold Level: A situation when the number of malaria cases is in excess of the normal number at a specific period and place. Therefore, the “normal” expected number must be estimated, by using a third quartile (second largest number) of the past five year’s weekly data.
Data Processing and Analysis
Four years Malaria data (july2013-june 2017) were collected, Organized, analyzed and interpreted accordingly Using Microsoft excels 2010.
Data Dissemination
Witten report of hard and soft copies will be prepared and shared to university of Gondar institute of public health, Ethiopia Field Epidemiology Training program, Benishangul Gumuz Regional Health Bureau, Asossa zone health Department and Menge woreda health office.
Ethical Consideration
The data were collected after having written consent letter from Benishangul Gumuz Regional health bureau to Menge Woreda to get ethical clearance. After discussing the purpose and method of the study, permission was sought from the woreda health department head before the data collection.
Results
Malaria Surveillance Data Analysis by Time
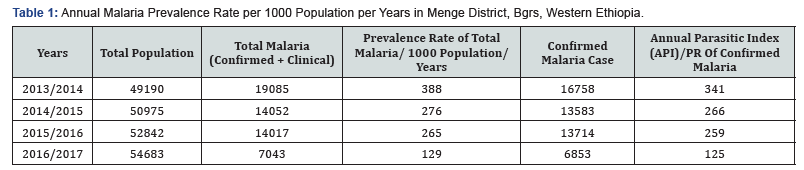
A total of 130730 suspected fever cases were examined by RDT/ microscopy/clinically from which total 54197 malaria cases (clinical (6%) + parasitological confirmed (94%) and 7 deaths were reported from July 2013-june 2017. The average number of malaria case reported to PHEM per year was 13605; it ranges from 19085 in 2013/2014 to 7043 in 2016/2017. During the same period, the average annual malaria prevalence rate of the district was 265 per 1000 population. The annual parasitic index (API) of malaria was decreased from 341 to 125/1000 population. In the four years period Malaria was decrease by 63.3% from the baseline 2013/2014. The average annual malaria reduction rate was 25.4% per years; with this trend or progress the district may need 4 to7 years to eliminate malaria in the woreda (Table 1). According to four years PHEM data, the highest case of Malaria was registered from July 2013-June 2014. From a total of laboratory confirmed malaria cases, plasmodium falciparum accounts 91% and the rest 9% were plasmodium Vivax. Even if the total malaria cases decrease from year to years, the sever form of malaria species (Plasmodium Falciparum) were increase from year to years (Figure 2). The cases treated with laboratory diagnosis using microscope and the rapid diagnostic kit were increases from year to years. From a total of 54,197 malaria cases reported within the four years period, 93.9 percent of cases were treated by using either of microscopic or RDT test results while 6.1 percent of malaria patient were treated with clinical sign and symptom (Figure 3).
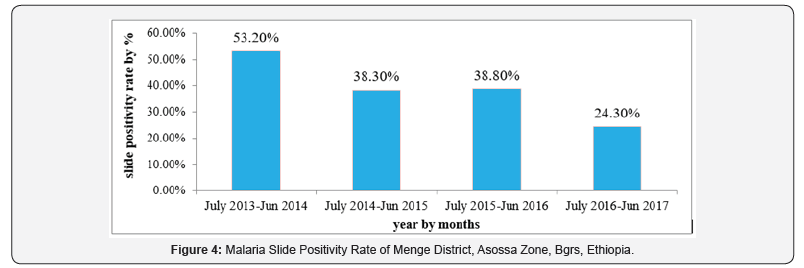
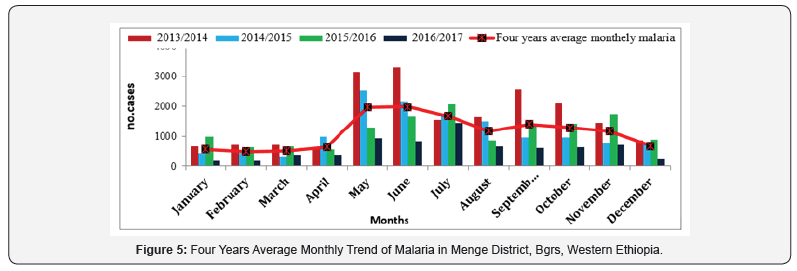
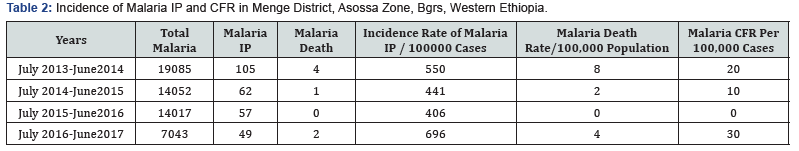
From a total of 130730 suspected fever cases examined by RDT or Microscopic, 50907 patients were positive for plasmodium species from July 2013 to June 2017; with average malaria positivity rate of 38.9%. Malaria positivity rate was decrease from 53.2% in 2013/2014 to 24.3% in 2016/2017. The positivity rate attains its maximum point (53%) from July 2013- June 2014 (Figure 4). In the district Malaria transmission starting to rise from September to December and again it starts to risefrom April to May. The highest malaria cases were reported from May to July and again from September to November or during kremt season. The lowest malaria case reported from the month of January to March (during dry season). The average monthly malaria cases of the past 4 consecutive years were reached around 1163. According to four years weekly PHEM data basis, in the district Malaria cases started to rise from WHO week 17 until WHO week 29 and again the cases start to rise at WHO week 40 (Figure 5). A total of 273 malaria inpatients and 7 deaths were reported from July 2013-june 2017, with case fatality rate (CFR) of 13per 100,000 cases. The incidences of both malaria inpatients and case fatality rate were increase with inconsistent trend, both were decreased from July 2013 to Jun 2016 and both become increased in July 2016- june2017. Even if malaria IP and CFR increased in inconsistent trend, Malaria death rate (from the total population) were decreases by half from (8/100,000 population in 2013/2014 to 4/100,000 population in 2016/2017 (Table 2).
Malaria Surveillance Data Analysis by Person
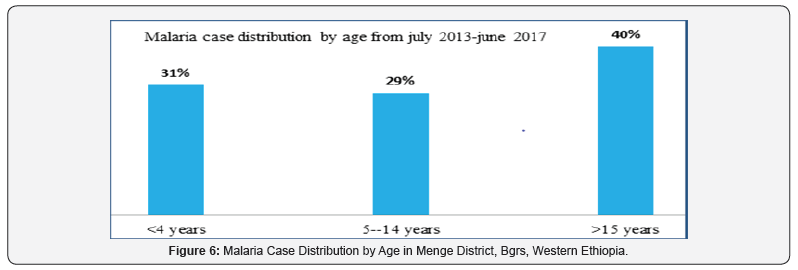
There was lack of same personal variables on weekly PHEM report format like sex and age to analysis the data by person. Due to this limitation I extract this data from HMIS report to show disease burden by sex and age. According to four years HMIS data Malaria was reported in all age groups and both sexes. The data also shows 52% of malaria cases were reported on Male sex and 40 % of the cases seen on above 15 age group of the population (Figure 6).
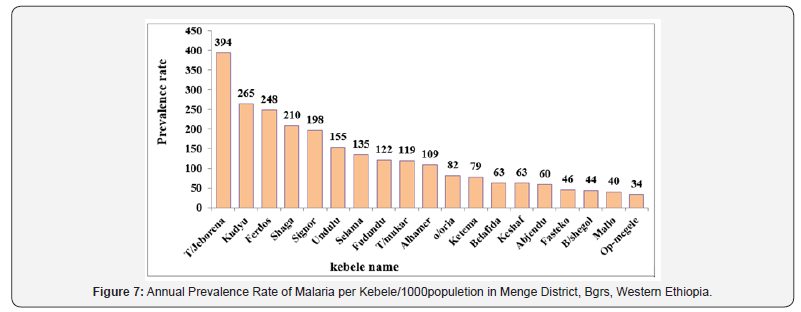
Malaria Surveillance Data Analysis by Place
The collected data verified that all kebele in the district were affected by malaria. From 24 kebele found in the district; kudyu; T/Jeborena; kudyu; Ferdos; shaga debazin; signor and undulu reported the high malaria over the past four years. The smallest malaria cases were reported from Op-Megele, Mallo, B/Shegol, Fasteko and Abjendu. The four years report completeness andtimelines of the district was above the standard (80%) (Figure 7).
Discussion
The finding of this analysis showed that malaria occurred throughout the year in all kebele in the Woreda with varying incidence between kebele. The average annual prevalence rate of malaria, from the overall population was 265 per 1000 risk population which is higher than Benishangul Gumuz region malaria prevalence rate 264 cases per 1000 population and national malaria prevalence rate 37 cases per1000 risk population according to 2015/2016 Ethiopian federal minister annual performance report [11,12]. In the four years period Malaria was decrease by 63% from the baseline of 2013/2014; Which has quite difference with the national strategic plan objective by 2020, to reduce malaria cases by 75% from baseline of 2013 [13]. This might be due to the climatic condition of the area which satisfied for mosquito replication and weak malaria prevention and control activity in the woreda. The cases treated with laboratory diagnosis using microscope and the Rapid Diagnostic kit increased from 81% in 2013/2014 to 97.3% in 2016/2017; this might be due to the change of malaria case treatment approach and availability of RDT & accessibility of electric power in lower health facilities become increasing time to time. Even if parasitological confirmed treatment rate were increased from year to years the four years average clinical malaria treatment rate was above 5%,which had differ from the national malaria guideline recommended that Patients who test negative by malaria RDT or microscopy do not need anti-malarial medications and Clinical treatment rate should not exceed 5% and also WHO recommends universal parasitological diagnosis of malaria to ensure targeted use of anti-malarial drugs for those individuals who actually have malaria [14]. This might be due to lacks RDT or reporting error that was done by health profession
Regarding to malaria slide positivity rate (SPR), it was decreases from 66% in 2013/2014 to 22% in 2016/2017, which might be associated with the decrement of the incidence rate or case in the population. The proportion of plasmodium Falciparum and Plasmodium Vivax were 91% and 9% respectively. However, other studies report also indicates the consistent dominance of Plasmodium falciparum [15,16]. This proportion is varying from the national malaria species proportion of Plasmodium falciparum and plasmodium Vivax were 60:40 respectively [7,8]. This variation might be due to the altitude and climate difference of the district. In the four years period; malaria death rate was decreased from 8 to 4 per 100,000 cases with inconsistent trend, which were lower than the national malaria strategic plan of elimination phase objectives by 2020, to achieve near zero malaria in Ethiopia. The incidences of both malaria inpatients and case fatality rate were increase with inconsistent trend, both were decreased from July 2013- Jun 2016 but both were increased from July 2016 to June 2017. The average malaria case fatality rate (CFR) were 13per 100,000 cases, which were less than the regional malaria case fatality rate (20 per 100000 cases) but greater than national malaria case fatality rate, which was 4 per 100,000case [11].The increments of malaria inpatient, and CFR might be associated with the increment of sever form of plasmodium falciparum malaria species, late detection and treatment of malaria cases and yearly difference of seasonal climate change which is suitable for malaria breading and inconsistent malaria prevention strategy and intervention performance.
In the district malaria transmission starting to rise from September to December and again start from April to May. which were similar to the major and minor malaria transmission season in the region and the nation which occur between September and December, after the main rainy season and in Certain areas, largely in the western and eastern parts of the country experience a second “minor” malaria transmission period from April to May, following a short rainy season [17]. Malaria cases predominantly high during the month of May to September during Kermit season, the result is similar to the assessment conducted in benishangul gumuz region, malaria transitions are high during Kermit season of May, June, July, august and September [18,19].This might bedue to the situation of rainfall, humidity and temperature were satisfied the approach over all kebele of the Woreda. The highest Malaria cases and incidence were recorded in kudyu, Ferdos, signor, T/Jeborena, and shaga. This might be due to presence of malaria birding site near to the kebele, high population flow for agricultural investment and minerals, and presence of irrigation projects may be influencing malaria transmission. The smallest malaria cases were reported from op-Megele, Fasteko, ketema, Mallo, Banishegol, and Abjendu. The district health office and the health professions should closely follow malaria trends in this kebele because they are more prone to epidemics.
Conclusion
Malaria continued to be a major health problem in the district; it causes high morbidity and mortality. The four years PHEM data suggested that the scale up of interventions had considerable positive impact on malaria outpatient cases, it decreases malaria outpatients’ cases by 63% from the baseline 2013/2014. Parasitological confirmatory malaria treatment rate was increased from year to year and on the contrary clinical malaria treatment rate were decreases. Plasmodium falciparum malaria species was very high (91%) and increased from year to years. The incidence of both malaria inpatients and malaria case fatality rate were increase with inconsistent trend, which is difficult to forecast the futurity. Malaria transmission starting to rise from September to December and again it starts to rise from April to May. Malaria is predominantly higher during kremt season in the months of May, June July and September. All kebele in the district were endemic for malaria throughout the year. The highest incidence of malaria cases was recorded in kudyu, T/ Jeborena, Ferdos, shaga and signor kebele.
Recommendations
a. The district health office and health professions should strengthen the malaria prevention and control programmed, particularly in the geographical areas of highest incidence to keeping the current achievements especially on outpatient’s cases and to roll back the disease.
b. The woreda heath office, health workers, HEWs and the community should strength early detection and treatment of malaria cases at all level to decrease malaria IP and CFR.
c. The woreda health office should asses the cause of high prevalence of clinical treatment rate in the district and solve accordingly
d. The Regional health bureau and the district should plan to do further study to know the cause of high prevalence of plasmodium PF malaria species, Malaria IP and malaria case fatality (MCFR) rate for prevention and control of malaria to come to elimination.
e. The Regional health bureau should be incorporate personal variable such as age and sex in PHEM reporting format.
f. The PHEM officers at district and health facility level should strength documentation and handling of malaria data by species in all kebele of the district and analysis the data and alert the community before occurrence of outbreak during pick transition seasons.
References
- White NJ (2008) Plasmodium knowlesi: the fifth human malaria parasite. Clin Infect Dis 46(2): 172-173.
- Delenasaw Y, Worku L, Wim VB, Solomon G, Kloos H, et al. (2009) Malaria and water resource development: the case of Gilgel-Gibe hydroelectric dam in Ethiopia. Malaria journal 8: 21.
- WHO (2016) Trends of malaria control and elimination across the globe World Malaria Report.
- Reuben R (1993) Women and Malaria RR - Special Risks and Appropriate Control strategy. Soc sci Med 37(4): 473-80.
- Ministry of Health (2012) Summary proceedings 3rd annual malaria control program review Ethiopia and Nigeria Held on February September.
- Barofsky J, Chase C, Anekwe T, Farzadfar F (2011) The economic effects of malaria eradication: Evidence from an intervention in Uganda.
- MOH (2012) National Malaria guideline Final, Effect of Antimalarial Interventions. Addis Ababa, Ethiopia.
- Hwang J, Jima D, Getachew A, Bilak H, Steketee RW, et al. (2007) Malaria Indicator Survey Working Group. Malaria related health behaviors associated with women’s knowledge of malaria. Malaria Indicator Survey, Ethiopia.
- Yaregal G, (2015) B/G/R/S malaria surveillance data analysis.
- Back R (2005) World Malaria Report Malaria Monitoring and Evaluation. Ethiopia.
- MOH E (2006) Health sector transformation plan annual performance report EFY 2008. p. 37-38.
- WHO (2015) Achieving the malaria MDG target: reversing the incidence of malaria.
- National Malaria Program Monitoring and Evaluation Plan 2014 - 2020, Addis Ababa June 2014.
- Federal Democratic Republic of Ethiopia MOH (2012) Malaria diagnosis and treatment Guidelines for Health Workers in Ethiopia, Addis Ababa, Ethiopia.
- Tesfaye S, Belyhun Y, Teklu T, Mengesha T, Petros B (2011) Malaria prevalence pattern observed in the highland fringe of Butajira, Southern Ethiopia: a longitudinal study from parasitological and entomological survey. Malar J 10:153.
- Abebe Alemu, Dagnachew Muluye, Mikrie Mihret, Meaza Adugna, Melkamu Gebeyaw (2012) Tenyear trend analysis of malaria prevalence in Kola Diba, North Gondar, Northwest Ethiopia. 5:173.
- Karunamoorthi K, Bekele M (2009) Prevalence of malaria from peripheral blood smears examination: a 1-year retrospective study from the Serbo Health Center, Kersa Woreda, Ethiopia. 2(4): 171-6.
- Sena L, Deressa W, Ali A (2015) Correlation of Climate Variability and Malaria: A Retrospective Comparative Study, Southwest Ethiopia. Ethiopian journal of health sciences 25(2): 129-138.
- Agence M (2016) Assessment and outlook of malaria Transmission During kiremt in terms of climate Suitability in benishangul gumuz region.






























