A Rare Case of Infective Endocarditis Presenting with Acute ST-Segment Elevation Myocardial Infarction and Aortic Root Abscess
Jafar Alzubi1*, Ahmad Jabri1 and David Hedrick2
1Department of Internal Medicine, Cleveland Clinic Akron General, USA
2Department of Cardiovascular Medicine, Cleveland Clinic Akron General, USA
Submission: June 13, 2019; Published: July 03, 2019
*Corresponding author: Jafar Alzubi, Department of Internal Medicine, Cleveland Clinic Akron General, Akron, OH 44307, USA
How to cite this article: Jafar A, Ahmad J, David H. A Rare Case of Infective Endocarditis Presenting with Acute ST-Segment Elevation Myocardial Infarction and Aortic Root Abscess. JOJ Int Med. 2019; 1(1): 555554.
Abstract
Acute coronary syndrome (ACS) is a rare complication in patients with infective endocarditis with high mortality rate, and it is most commonly caused by septic embolization into coronary arteries. Management of ACS caused by infective endocarditis is challenging, and the mainstay management of this clinical entity is still uncertain. Here, we report a 28-year-old male with infective endocarditis of native aortic valve complicated by acute ST-segment elevation myocardial infarction caused by septic emboli into multiple coronary arteries and aortic root abscess. This case emphasizes a rare presentation and complications of infective endocarditis in addition to the importance of early diagnosis of infective endocarditis-related ACS which its management is different from atherosclerotic coronary artery disease.
Keywords: Infective endocarditis Acute coronary syndrome Aortic abscess Fever
Abbrevations: ACS: Acute Coronary Syndrome; EKG: Electrocardiogram; IE: Infective Endocarditis; LAD: Left Anterior Descending; MRSA: Methicillin- Resistant Staphylococcal Aureus; PCI: Percutaneous Coronary Intervention; STEMI: ST-Segment Elevation Myocardial Infarction; TEE: Transesophageal Echocardiogram
Introduction
Infective endocarditis (IE) is a common disease with a significant healthcare burden and high mortality rate, ranging from 16% to 25% [1]. The high mortality rate of IE stems from its potential complications, which include septic embolization, valve destruction, mycotic aneurysms, and abscess formation. Septic embolization has a high incidence rate, up to 49%, in IE patients, and it mostly involves the central nervous system, kidney, spleen, and liver [1,2]. However, coronary embolization resulting in acute coronary syndrome is a rare complication of infective endocarditis and represents less than 1% of IE-related complications [3]. The objective of this case is to describe a patient with infective endocarditis of native aortic valve complicated by acute ST-segment elevation myocardial infarction (STEMI) caused by septic emboli into multiple coronary arteries and aortic root abscess. This case emphasizes a rare presentation and complications of infective endocarditis in addition to the importance of timely diagnosis and management of infective endocarditis-related acute coronary syndrome, which has prognostic impact on this life-threatening condition.
Case Report
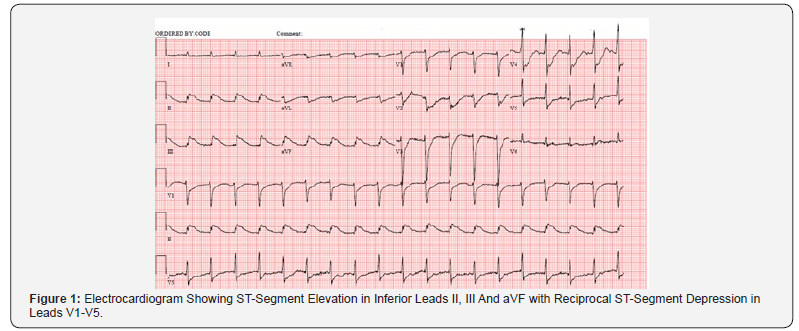
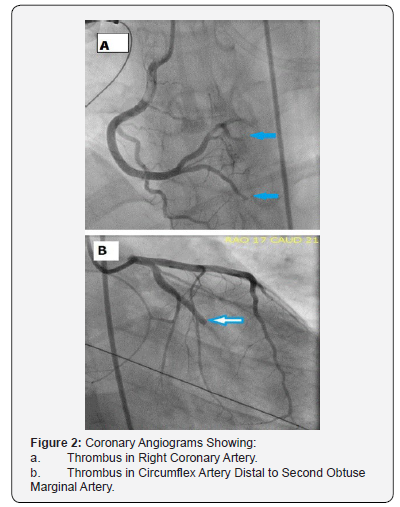
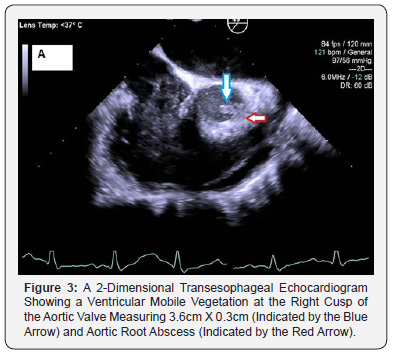
A 28 years old Caucasian male with past medical history significant for type 1 diabetes mellitus, essential hypertension and hyperlipidemia presented to the emergency department with fatigue, myalgia and chills of one-week duration. On presentation, the patient had a temperature of 97.3°F, blood pressure of 90/50 mmHg, heart rate of 140 beats per minute, and respiratory rate of 20 cycles per minute. Initial electrocardiogram (EKG) showed sinus tachycardia. Initial lab analysis revealed a troponin of 0.324ng/ml (normal <0.015ng/ml), leukocytosis with positive bacteriuria and pyuria on microscopic urine analysis. Ten hours after his presentation, the patient developed ventricular fibrillation cardiac arrest. Return of spontaneous circulation was achieved after 30 minutes of resuscitation, and a subsequent EKG (Figure 1) showed changes consistent with STEMI. Subsequently, emergent coronary angiograms (Figure 2) revealed thrombi in multiple coronary arteries; thus, no intervention was performed. Subsequently, an intra-aortic balloon pump was inserted, and the patient was started on multiple vasopressors and broad-spectrum antibiotics for septic and cardiogenic shock. Blood cultures grew methicillin-resistant Staphylococcal aureus. A 2-dimensional transesophageal echocardiogram (Figure 3) revealed ventricular mobile vegetation at the right cusp of the aortic valve measuring 3.6cm x 0.3cm with an aortic root abscess adjacent to the non-right commissure and a large pericardial effusion with left ventricular ejection fraction of 25%.
Hence, patient’s ACS and coronary emboli were attributed to aortic valve IE with septic embolization. Over the course of next few days, the patient developed multiple systemic septic emboli to the spleen and kidneys that were evident on a CT-abdomen without contrast. Cardiothoracic surgery was consulted for recommendations on aortic valve replacement and aortic root debridement. The patient underwent mechanical aortic valve replacement and root replacement with a 24mm homograft. Debrided aortic root specimens grew MRSA. A 2-dimensional transthoracic echocardiogram (TTE) subsequent to surgeryshowed improved left ventricular ejection fraction from 25% to 35%. The patient was discharged to a rehabilitation center after a 60-day hospital course.
Discussion
This is a rare case of native aortic valve IE presenting with ventricular fibrillation arrest and acute STEMI with aortic root abscess. Acute coronary syndrome is a rare complication of IE that is associated with high mortality rate. IE can cause myocardial infarction by different mechanisms including coronary embolization, complete occlusion of coronary ostia by vegetation on aortic cusp or external compression of coronaries from peri annular abscesses, and mycotic aneurysms [4]. Risk of coronary embolization generally increases with mobile vegetations, vegetation length >10 mm, infection with virulent organism, a previous embolism, and aortic valve endocarditis due to close proximity of the vegetations to the coronary ostia [5]. Additionally, septic emboli have been reported to format a higher rate in prosthetic valves than in native valves [6]. Diagnosis for coronary septic embolization is usually by coronary angiogram. Despite the risk of systemic embolization during cardiac catheterization, coronary angiography is considered a safe procedure in the setting of IE [7]. Management of ACS caused by infective endocarditis is considered challenging. The conventional treatment of acute coronary syndrome including antiplatelet therapy, anticoagulants, and thrombolytics can potentially result in fatal complications, particularly cerebral hemorrhage, given that many IE patients have concomitant septic emboli at other arterial beds including the brain, kidneys, and spleen [8]. While stent placement at the site of septic coronary embolism can displace the embolus, and compress it laterally against the coronary wall, which can potentially result in mycotic aneurysms.
Additionally, percutaneous transluminal coronary angioplasty of non-atherosclerotic coronary wall, which is compliant with elastic recoil features, can lead to suboptimal results including vessel re-occlusion, distal embolization, mycotic aneurysm formation, or coronary rupture and sudden death. Therefore, percutaneous coronary intervention (PCI) in IE-related ACS whether by stent placement or angioplasty, should generally be avoided [8-10]. However, aortic root abscess is considered a main indication for valve surgery.
Conclusion
Acute STEMI is a rare complication of IE and, on occasion, may be the initial presentation of infection as with this patient who had septic embolization into multiple coronary arteries. The diagnosis of IE in a patient presenting with STEMI is challenging and requires a high degree of suspicion for timely diagnosis and management, which has prognostic impact on this life-threatening condition. Management is also challenging, andit should be individualized based on patient’s age and overall clinical presentation including concomitant IE complications. Percutaneous coronary intervention should generally be avoided in this setting due to its associated complications.
References
- Mylonakis Eleftherios, Calderwood SB (2001) Infective endocarditis in adults. N Engl J Med 345: 1318-1330.
- Khan F, Khakoo R, Failinger C (2005) Managing embolic myocardial infarction in infective endocarditis: current options. J Infect 51(3): e101-105.
- Yeoh J, Sun T, Hobbs M, Looi JL, Wong S (2012) An uncommon complication of infective bacterial endocarditis. Heart Lung Circ 21(12): 811-814.
- Murtaza G, Rahman ZU, Sitwala P, Ladia V, Barad B, et al. (2017) Case of Acute ST Segment Elevation Myocardial Infarction in Infective Endocarditis-Management with Intra Coronary Stenting. Clin Pract 7(3): 950.
- Sofía Calero-Núñez, Vicente Ferrer Bleda, Miguel Corbí-Pascual, Juan Gabriel Córdoba-Soriano, Raquel Fuentes-Manso, et al. (2018) Myocardial infarction associated with infective endocarditis: a case series. European Heart Journal - Case Reports 2(1): 1-7.
- Manzano MC, Vilacosta I, San Román JA, Aragoncillo P, Sarriá C, et al. (2007) Acute coronary syndrome in infective endocarditis. Rev Esp Cardiol 60(1): 24-31.
- Welton DE, Young JB, Raizner AE, Ishimori T, Adyanthaya A, et al. (1979) Value and safety of cardiac catheterization during active infective endocarditis. Am J Cardiol 44(7): 1306-1310.
- Hunter AJ, Girard DE (2001) Thrombolytics in infectious endocarditis associated myocardial infarction. J Emerg Med 21(4): 401-406.
- Glazier JJ, McGinnity JG, Spears JR (1997) Coronary embolism complicating aortic valve endocarditis: treatment with placement of an intracoronary stent. Clin Cardiol 20(10): 885-888.
- Taniike M, Nishino M, Egami Y, Kondo I, Shutta R, et al. (2005) Acute myocardial infarction caused by a septic coronary embolism diagnosed and treated with a thrombectomy catheter. Heart 91(5): e34.






























