Cutaneous Lupus Erythematosus: An Overview of Clinical Manifestations
Laura Sofia Triviño1*, Maria Alejandra Nieto Salazar1, Salma Habib2, Jessica Mariela Amaya Alvarez3, Zulma Dorila Sosa Carcamo4, Erick Flores5, David Adrian De Leon Garza6, Fredy Reynaldo Pavón Enamorado7, Ernesto Calderon Martinez8, Jhon Navarro González9, David Arriaga Escamilla10, Fatima Shaheen11 and Blanca Estefanie Avalos Quijano4
1Juan N Corpas University, Colombia. Larkin Community Hospital, USA
2Institute of Applied Health Science, Bangladesh. Larkin Community Hospital, USA
3Universidad Salvadoreña Alberto Masferrer, El Salvador. Larkin Community Hospital, USA
4Universidad Evangélica de El Salvador, El Salvador
5Centro de Estudios Universitarios Xochicalco, México
6Universidad de Monterrey, México
7Universidad Católica de Honduras, Honduras
8Universidad Nacional Autónoma de México, México
9Universidad Del Zulia, Venezuela
10Universidad Justo Sierra, México
11MNR Medical College, India
Submission: February 02, 2023;Published: February 15 2023
*Corresponding author: Laura Sofia Triviño, Juan N Corpas University, Colombia. Larkin Community Hospital, USA
How to cite this article: Laura Sofia Triviño, Maria Alejandra Nieto Salazar, Salma Habib, Jessica Mariela Amaya Alvarez, Zulma Dorila Sosa Carcamo, et al. Cutaneous Lupus Erythematosus: An Overview of Clinical Manifestations. JOJ Dermatol & Cosmet. 2023; 5(2): 555658. DOI: 10.19080/JOJDC.2023.05.555658
Abstract
Background: cutaneous lupus erythematosus (CLE) is one of the four main types of lupus, a well-known chronic inflammatory autoimmune disease. Subtypes are currently grouped based on histology, duration, clinical findings, and laboratory tests. Lupus erythematosus is a connective tissue disease with a complex involvement of immunologic, genetic, and environmental factors. Although the etiology is poorly understood, insights elucidate the importance of disrupting hemostasis from the immunoregulatory disarray, immunologic tolerance, complement system, and development of autoantibodies.
Purpose of the study: This narrative review aims to provide a comprehensive overview of the clinical presentation, diagnosis, and treatment of the different subtypes of CLE to better understand this complex condition and its subtypes.
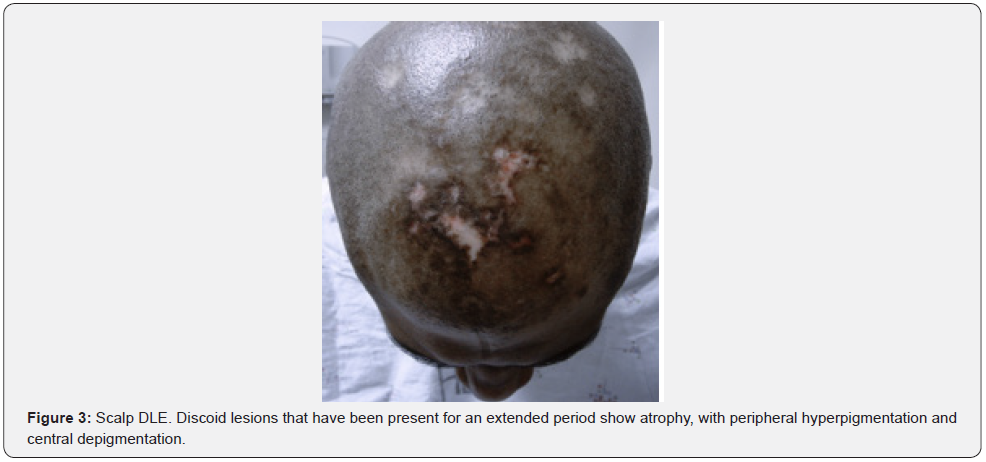
Results/findings: The incidence of CLE varies among different racial and ethnic groups. It is more prevalent in women, with a female-to-male ratio of approximately 9:1. Incidence of CLE is challenging to estimate because the condition is often underdiagnosed, and there is a lack of population-based studies. Acute Cutaneous Lupus has the highest incidence. The hallmark feature of localized lesions is malar rash or butterfly erythema. Subacute Cutaneous Lupus, a non-scarring, highly photosensitive erythematous rash, over sun-exposed areas, with hypopigmentation or telangiectasia. Chronic Cutaneous Lupus, the subtype Discoid LE (DLE), is the most common, with well-defined erythematous plaques exacerbated by sun exposure becoming atrophic, with hyperpigmentation peripherally and depigmentation centrally through time.
Conclusion: The treatment of most CLE subtypes includes ultraviolet light protection, corticosteroids, and calcineurin inhibitors. Novel treatments such as biological therapies continue under investigation, but preliminary data seems promising.
Keywords: Acute cutaneous lupus erythematosus; Chronic cutaneous lupus erythematosus; Cutaneous lupus erythematosus; Discoid lupus erythematosus; Lupus erythematosus profundus; Lupus erythematosus tumidus; Sub-acute cutaneous lupus erythematosus
Abbreviations: Neonatal and pediatric Lupus Erythematosus (NLE); Cutaneous Lupus Erythematosus (CLE); Drug-Induced Lupus (DIL); Systemic Lupus Erythematosus (SLE) Acute Cutaneous Lupus Erythematosus (ACLE), Subacute Cutaneous Lupus Erythematosus (SCLE), Chronic Cutaneous Lupus Erythematosus (CCLE). Discoid Lupus Erythematosus (DLE), Lupus Erythematosus Profundus (LEP), Chilblain Lupus Erythematosus (CHLE), Lupus Erythematosus Tumidus (LET); Toxic Epidermal Necrolysis (TEN)-like; Ultraviolet (UV)
Introduction
The term lupus was first applied to skin disease in 916 AD by Hebernus of Tours. Willan, in 1700 used the term lupus to describe destructive and ulcerative conditions of the face. However, the first clear description of lupus was reported by Cazenave in 1833 under the term erythema centrifugum, which a few years later he renamed the term, calling it lupus erythematosus and gave the classic description of discoid lupus erythematosus. Lupus is defined as a chronic inflammatory autoimmune disease with a wide range of clinical presentations resulting from its effect on multiple organ systems. The four main types of lupus are neonatal and pediatric lupus erythematosus (NLE); cutaneous lupus erythematosus (CLE); drug-induced lupus (DIL); and systemic lupus erythematosus (SLE). Cutaneous lupus erythematosus is a frequent finding in systemic lupus erythematosus patients and can also exist as a single entity without associated systemic autoimmunity. Subtypes of CLE are currently grouped based on histology, lesion duration, clinical findings, and laboratory abnormalities, which includes acute cutaneous LE (ACLE), subacute cutaneous LE (SCLE), and chronic cutaneous LE (CCLE). CCLE encompasses discoid LE (DLE), LE profundus (LEP), chilblain LE (CHLE), and LE tumidus (LET) [1]. The frequency of cutaneous manifestations in SLE is as high as 70%, and the overall prevalence of CLE is reported as more significant than 0.07% and may be equivalent to SLE in some populations [2]. Similar to proposed etiologies for SLE, current theories discuss a multifactorial relationship leading to the development of cutaneous lupus, including genetic susceptibility, autoimmune induction, and immune system damage.
In order to properly diagnose cutaneous manifestations of LE, the physician must first correctly classify the subtype and exclude systemic involvement of the disease. CLE diagnosis should be based on the findings of patient history, clinical exam, laboratory studies, serology, as well as histology, and direct immunofluorescence (DIF) exam of skin biopsies if the histology is not diagnostic [1]. The approach to the treatment of signs and symptoms of lupus depends on the type and the severity of the disease. General recommendations for all patients include sunlight protection, proper diet and nutrition, exercise, smoking cessation, appropriate immunizations, and management of comorbid conditions [3]. This review study aims to provide a comprehensive overview of the clinical presentation, diagnosis, and treatment of the different subtypes of CLE to better understand this complex condition and its various subtypes.
Etiology and Pathogenesis
Lupus erythematosus is a connective tissue disease with a diverse variety of cutaneous manifestations with the complex involvement of immunologic factors, genetic susceptibility, and environmental triggers exposure [4]. The etiology is typically defined by the interaction of these multiple factors that together trigger the development of the disease. Insights from the complex study of disease pathogenesis elucidate the importance of the implication of the loss of hemostasis from the immunoregulatory disarray, loss of immunologic tolerance, the complement system activation, to the development of autoantibodies that arises from the spectrum of innate and adaptive immune components activation response [5]. The autoimmune pathways involved in the disease development and pathogenesis still need to be clarified entirely and understood, as susceptibility from mutation, various risk alleles, genetic polymorphisms, and ultimately the interaction with the environment triggers immune activation and disease manifestation [6]. Unregulated keratinocyte apoptosis is one of the critical factors that has been implicated in the development of CLE manifestations through dysregulated pathways such as p53, TNFa, Fas/FasL, unwanted antigen-presenting of anomalous MHC [5], and ultimately releasing nuclear debris that serves as the reservoir of autoantigen for autoreactive T and B cells [6].
Epidemiology
The epidemiology of CLE in the United States is not well defined, but it is estimated that between 5% and 10% of people with systemic lupus will develop the condition [7,8]. The incidence of CLE varies among different racial and ethnic groups. According to the Lupus Foundation of America, African Americans, Hispanic Americans, and Asian Americans are more likely to develop lupus and CLE than non-Hispanic white Americans [8]. CLE is more common in women than men, with a female-to-male ratio of approximately 9:1. The disease typically develops between the ages of 20 and 50. However, it can occur at any age [7]. CLE is a chronic condition that can significantly impact a person’s quality of life. The disease is associated with an increased risk of skin cancer, as well as with other complications such as scarring, disfigurement, and infections. There are several risk factors for CLE, including exposure to sunlight, hormonal changes (such as pregnancy or menopause), and certain medications (such as hydrochlorothiazide and quinidine). People with other autoimmune diseases, such as rheumatoid arthritis or Sjogren’s syndrome, are also at an increased risk of developing CLE [9]. It is important to note that the incidence of CLE is challenging to estimate because the condition is often underdiagnosed, and there is a lack of population-based studies. However, it is clear that CLE is a relatively uncommon disease and that it is more common in people with darker skin tones and in women [7,8,9].
Acute Cutaneous Lupus
Acute Cutaneous Lupus Erythematosus (ACLE) has the highest incidence of systemic involvement (∼90%) and is more common in female patients with fair skin in their 30s [10]. ACLE is subdivided into localized lesions and generalized lesions. The hallmark feature of localized lesions is malar rash or butterfly erythema, which is described as symmetrical erythema/redness (and/or edema) over the dorsum of the nose and malar region that spares the nasolabial folds, might last days to weeks and often appears after sun exposure (typically misinterpreted as sunburn) (Figure 1). Generalized ACLE is less common and is associated with systemic disease activity. It presents as a symmetrically widespread macular or maculopapular exanthema that involves the trunk and extremities, in particular UV-exposed areas (i.e., V-area of the neck and extensor aspects of the arms). The palmar surfaces, hands’ dorsum, and fingers’ extensor surfaces are commonly involved, while interphalangeal and metacarpophalangeal joints are typically spared. Additionally, telangiectasia and periungual erythema frequently arise at the nail fold and may be associated with a red lunula. The severe form of generalized ACLE is characterized by toxic epidermal necrolysis (TEN)-like lesions and is described as “Acute Syndrome of Apoptotic Pan Epidermolysis” and is rarely seen in patients with the disease [11].

The diagnosis of ACLE requires proper sub-type classification through a combination of physical examination, laboratory studies, histology, and antibody serology. Also, direct immunofluorescence and photo-provocation may be used to confirm the diagnosis in some specific cases to exclude systemic disease [1]. It is important to establish the histopathological diagnosis by punch biopsy since the condition is chronic and often requires systemic treatment and comprehensive advice regarding triggering factors. Histologically, ACLE lesions show liquefactive degeneration of the basal layer, edema of the upper dermis, and a scattered interface, perivascular, and peri adnexal lymphocytic infiltrate, all of which are generally less pronounced as compared to other CLE subtypes. Immunologically, a positive ANA is found in 95% of ACLE patients, as well as a high incidence of anti-dsDNA and anti-Sm antibodies. Lesional direct immunofluorescence reveals granular immune deposits at the dermal-epidermal junction and perivascular deposits in the upper dermis, most commonly IgM [1]. The first-line treatment of ACLE is patient education on proper UV protection and appropriate local therapy with corticosteroids or calcineurin inhibitors and systemic agents. UV protection includes sun avoidance, protective clothing, and broadspectrum sunscreens with a high UV-protecting factor. Systemic agents are indicated in cases of widespread scarring or treatmentrefractory disease [12]. For refractory cases, several treatments can be attempted, such as retinoids, methotrexate, thalidomide, mycophenolate, azathioprine, and dapsone.
Subacute Cutaneous Lupus
Subacute Cutaneous Lupus (SCLE) primarily occurs in an age range of 50 - 52 years [13]. SCLE is a non-scarring, highly photosensitive erythematous rash often presented over sun-exposed areas [14]. The condition may present with hypopigmentation, telangiectasia, and multiple papulosquamous or annular polycyclic lesions (Figure 2). Patients frequently have mild disease severity with musculoskeletal complaints and serologic abnormalities. SCLE is manifested more often in the arms, neck, shoulders, chest, and extensor surfaces and usually spares the face. The diagnosis is mainly based on clinical features and confirmed by histopathology. Severe systemic disease is less common in these patients. However, around 10% of patients can present central nervous system involvement, vasculitis, or nephritis [15]. The treatment includes lifestyle management, sunprotective clothes, proper use of sunscreen, and pharmacological therapy [16]. The first line of treatment consists of corticosteroids and calcineurin inhibitors. If the conditiosn is refractory, secondline options include methotrexate, belimumab, and/or dapsone [16].

The existent classification for Chronic Cutaneous Lupus Erythematosus (CCLE) is a subdivision that encompasses the Discoid LE (DLE), Lupus Erythematous tumidus (LET), lupus erythematosus panniculitis/profundus (LEP) and chilblain LE. By far, the most common subtype is DLE, with a 50% frequency in women in their fourth and fifth decade of life but with a more benign course (only 5-10% develop SLE). Table 1 compares the main findings of the three types of CLE and their corresponding risk of developing SLE. The clinical features of DLE include welldefined erythematous and scaly-like plaques localized primarily in the head and/or neck. Lesions are commonly exacerbated by sun exposure and trauma. As time advances, lesions become atrophic, peripheral hyperpigmentation, and central depigmentation. A classic longstanding discoid lesion of the scalp can be seen in Figure 3 [17].

The LEP or panniculitis sub-type is distinguished for presenting painful indurated nodules or plaques distributed in the face, scalp, upper torso, buttocks, and proximal extremities. Although it’s not clear the number of patients that will develop SLE in their disease course, Stull et al. described that around 50% of these patients present with DLE skin lesions in the overlaying skin during the diagnosis. Lupus Tumudus (LET), a CCLE subtype, has been characterized as less likely to be associated with SLE due to its benign course and only subtype occurring most commonly in men. Some authors and European guidelines even considered LET as the fourth CLE variant. The described lesions for LET subtype are strongly photosensitive erythematous macules, papules, plaques with smooth surfaces, sharply raised borders and no scale. Lastly, Chillbain LE is a rare CCLE variant that potentially develops features of SLE in approximately 20% of the patients. The CCLE frostbite-like lesions appear as painful, violaceous plaques/nodules in cold-exposed areas, provoking central erosions or ulcerations on acral surfaces [18]. For all the different CLE sub-types, a very detailed skin examination continues to be fundamental in order to properly diagnose all the cutaneous manifestations of LE and differentiate other skin conditions with skin biopsies. Furthermore, no specific approach for the CCLE subtypes differs from the essential preventive measures for cutaneous disease in SLE described above. These include aggressive sunprotective measures, Vitamin D supplementation, topical agents, and systemic first line and second-line treatments. In recent years, multiple agents (mainly biological therapies) have been under extensive investigation (i.e., Iberdomide) and have shown advantageous effects in phase II trials in patients with SCLE and CCLE [19].
Conclusion
Cutaneous Lupus Erythematosus is one of the four main types of Lupus, and it is a frequent clinical manifestation in Systemic Lupus Erythematosus. The autoimmune pathogenesis hasn’t been clarified yet, and there are still enormous efforts worldwide to elucidate the pathways that trigger the development of the disease. The clinical manifestations, including elementary lesions, topography, and the association with UV rays’ exposition, have been excellently described in the literature and synthesized in this review. Current evidence supplies the clinician with the appropriate tools to set up a diagnosis. Although the diagnosis might be challenging, physicians and other healthcare professionals have the resources to provide general recommendations for reducing CLE severity in order to prevent skin damage. The effectiveness of new treatments, such as biological medications, is still in the early stages of research, but preliminary results appear promising.
References
- Okon LG, Werth VP (2013) Cutaneous lupus erythematosus: diagnosis and treatment. Best Pract Res Clin Rheumatol 27(3): 391-404.
- Stannard JN, Kahlenberg JM (2016) Cutaneous lupus erythematosus: updates on pathogenesis and associations with systemic lupus. Curr Opin Rheumatol 28(5): 453-459.
- Stull C, Sprow G, Werth VP (2023) Cutaneous Involvement in Systemic Lupus Erythematosus: A Review for the Rheumatologist. J Rheumatol 50(1): 27-35.
- Bitar C, Menge TD, Chan MP (2022) Cutaneous manifestations of lupus erythematosus: a practical clinicopathological review for pathologists. Histopathology 80(1): 233-250.
- Moura Filho JP, Peixoto RL, Martins LG, Duarte de Melo S, Ligiana Leite de Carvalhoet al. (2014) Lupus erythematosus: considerations about clinical, cutaneous and therapeutic aspects. An Bras Dermatol 89(1): 118-125.
- Little AJ, Vesely MD (2020) Cutaneous Lupus Erythematosus: Current and Future Pathogenesis-Directed Therapies. Yale J Biol Med 93(1): 81-95.
- Reddy BY, Hantash BM (2009) Cutaneous Connective Tissue Diseases: Epidemiology, Diagnosis, and Treatment. Open Dermatol J 3(1): 22-31.
- Lupus facts and statistics. Lupus Foundation of America.
- Blake SC, Daniel BS (2019) Cutaneous lupus erythematosus: A review of the literature. Int J Womens Dermatol. 5(5): 320-329.
- Grönhagen CM, Nyberg F (2014) Cutaneous lupus erythematosus: An update. Indian Dermatol Online J 5(1): 7-13.
- Kuhn Annegret, Landmann Aysche, Bonsmann Gisela. “Chapter 39: Cutaneous Lupus Erythematosus”. In Systemic Lupus Erythematosus: Basic, Applied and Clinical Aspects Edited by George C. Tsokos, 333-339.
- Kuhn A, Ruland V, Bonsmann G (2011) Cutaneous lupus erythematosus: update of therapeutic options part II. J Am Acad Dermatol 65(6): 179-193.
- Biazar C, Sigges J, Patsinakidis N, Vincent Ruland V, Susanne Amler, et al. (2013) Cutaneous lupus erythematosus: first multicenter database analysis of 1002 patients from the European Society of Cutaneous Lupus Erythematosus (EUSCLE). Autoimmun Rev 12(3): 444-454.
- Jatwani S, Hearth Holmes MP. Subacute Cutaneous Lupus Erythematosus. [Updated 2022 Aug 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing, US.
- Tiao J, Feng R, Carr K, Okawa J, Werth VP (2016) Using the American College of Rheumatology (ACR) and Systemic Lupus International Collaborating Clinics (SLICC) criteria to determine the diagnosis of systemic lupus erythematosus (SLE) in patients with subacute cutaneous lupus erythematosus (SCLE). J Am Acad Dermatol 74(5): 862-869.
- Nutan F, Ortega-Loayza AG (2017) Cutaneous Lupus: A Brief Review of Old and New Medical Therapeutic Options. J Investig Dermatol Symp Proc 18(2): S6-S6.
- McDaniel B, Sukumaran S, Koritala T, Tanner LS (2022) Discoid Lupus Erythematosus. In: StatPearls. Treasure Island (FL): StatPearls Publishing, US.
- Żychowska M, Reich A (2022) Chronic Cutaneous Lupus Erythematosus in a White Population: Dermoscopic Characteristics by Clinical Subtype, Lesion Location and Disease Duration. Dermatol Ther (Heidelb) 12(9): 2117-2133.
- Furie RA, Hough DR, Gaudy A, Ying Ye, Shimon Korish, et al. (2022) Iberdomide in patients with systemic lupus erythematosus: a randomised, double-blind, placebo-controlled, ascending-dose, phase 2a study. Lupus Sci Med 9: e000581.






























