Road-Map of Hidradenitis Suppurativa Management
Ebaa Sabri* and François Petit
Private Clinic, Paris, France
Submission: October 11, 2021;Published: October 18, 2021
*Corresponding author: Ebaa Sabri, Private Clinic, Paris, France
How to cite this article: Ebaa S, François P. Road-Map of Hidradenitis Suppurativa Management. JOJ Dermatol & Cosmet. 2021; 4(3): 555638. DOI: 10.19080/JOJDC.2021.04.555638
Abstract
Hidradentitis Suppurativa (HS) is a primarily a chronic inflammatory skin disease that effects the folliculopilosebaceous unit [1]. Consequently, an inflammatory cascade occurs, presenting as recurrent, painful and inflamed nodules that often rupture and leak purulent materials [2]. The chronic timeline of the disease leads to the progression of nodules into accesses, epithelized sinuses, fistulae, and characteristic “rope-like scarring” [3]. The HS prevalence is around 1% of the population, its onset is usually after puberty, and commonly developing early in the third decade of life, and frequently remains active during the third and fourth decades of life. The women experience often an improvement with the onset of menopause, while usually the men continue with the active disease after 50 years old [4]. HS is more in female than male (approximate ratio 3:1) [4]. Smoking is one of the risk factors [2]. Approximately 40% of the patients have family members affected by the disease [4].
Keywords:Hidradenitis suppurativa; verneuil ’s disease; purulent materials; epithelized sinuses, fistulae
Management Road-Map
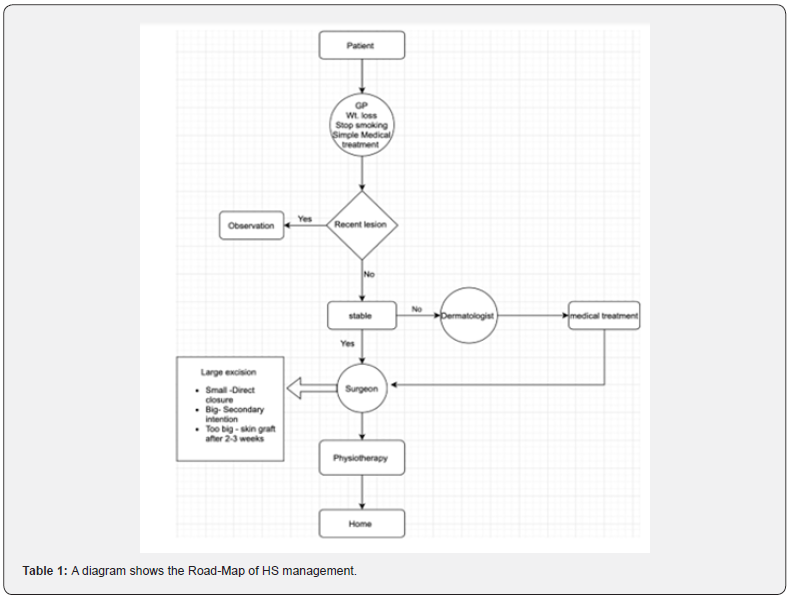
In many times the patients have been dispersed between different specialties, physicians, and medical structures. Here we present a road-map to orient the patients as well as the medical staff how to deal with HS correctly. The management of HS (Figure 1) requires a multi-disciplinary team (Table 1). This team consists of GP, dermatologist, surgeon, physiotherapist, nutritionist, psychologist, and a trained nurse. Sometimes we need all the members to deal with a patient and sometimes only some of them. The patient must firstly consults his GP, who should evaluate the condition, enhances the lift-style of the patient, cooperates with a nutritionist to reduce the weight, stop smoking and treat the simple cases. The condition is socially embarrassing that may give psychologic impacts on the patients who would be in need to have psychologic support. The improved cases need observation and follow-up with the GP. The resistant chronic lesions, must be referred to the surgeon for a surgical management. The surgeon evaluates the condition, the sever cases, chronic non-localized flared lesions in spite of the GP measures must be referred to a dermatologist to control and calm the active phase by medical therapy. After the stabilization and the settled down of the lesions. the dermatologist returns back the patient to the surgeon.
Surgical Treatment
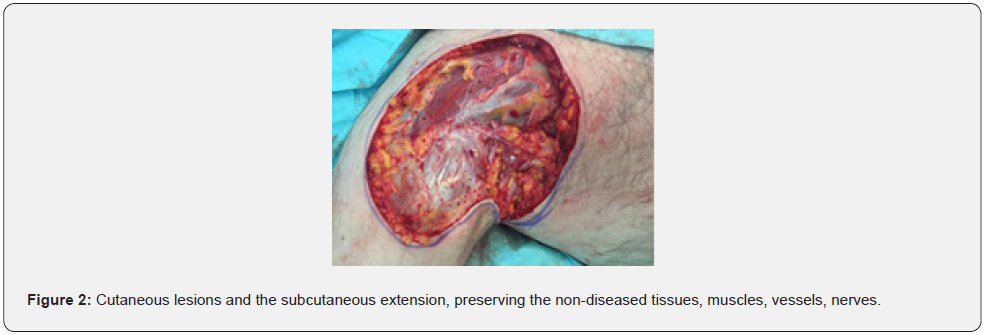
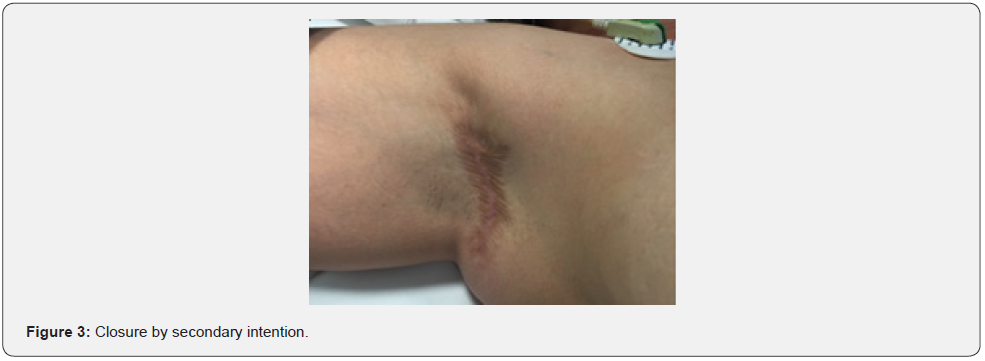
We recommend a trained plastic surgeon on these types of lesions to do the surgical treatment. We advise against the small excision, drainage, inserting a wick, etc. The surgical treatment consists of one or two stages; a wide excision with or without partial thickness skin graft, which will be planned 2-3 weeks post-excision. The excision (Figure 2) must be radical and large, consists of the totality of cutaneous lesions and the subcutaneous extension, preserving the non-diseased tissues, muscles, vessels, nerves. In a tiny lesion, we would -rarely- put some loosing stitches to bring the edges closer, not completely closed, to let a way-out for the exudates, and reduce the risk of recurrence. The open wound must be treated by regular dressing which would be done by a trained experienced nurse, using adaptable materials. We recommend “Algosteril” dressing every other day. This dressing gives excellent result on hemostasis, absorption and dryness of exudates by developing a granulation tissue. It can be changed easily in painless way. After 10 days the granulation tissue would be developed, no excessive exudation. We may switch to vaseline gauze dressing once each three days, and that must be controlled by the surgeon. Over the time the wound shrinkage continues until it will be completely closed by the secondary intention (Figure 3). This might take weeks. Sometimes we need to plan a partial thickness skin graft to cover the wound (Figure 4). The indications to have this second intervention are; a huge excision takes whole area, like whole armpit, long duration of immobility which consequently might cause a movement restriction and dysfunction. Long period of sick-leave, elevated expenses and being away from normal daily activities for a longtime. Finally, the presence of co-morbidity.


Discussion
HS is a chronic inflammatory disorder, effects about 1% of the people, with a male: female ratio 1:3 [1,5].
HS can be called Verneuil ’s disease after the French surgeon who described it. This chronic inflammatory condition effecting skin folds at axilla, inguinal, perineal and the inframammary regions. It is a disease of hair follicles [5].The patients sometimes are lost between different specialties, physicians and medical structures, and they become victims of incorrect or incomplete treatment. The loss of a strategy in the management leads to more complications, undesirable sequels, and long time suffering physically, socially and psychologically. That might occur due to patients and the medical staff unawareness or luck of strategy.
The road-map of the treatment needs sufficient time and efforts to achieve our goal but it is like a road-navigator which shows us the way to our destination in the best and safe manner. So this letter will help both, patients and medical staff to avoid miss management of this disease.
References
- Mazeika E, Jariene V, Valiukeviciene S (2021) Medical infrared thermography as hidradenitis suppurative diagnosis tool: literature review. Adv Dermatol Allergol XXXVIII (1): 32-35.
- Mokos ZB, Mise J, Balic A, Marinovic B (2020) Understanding the relationship between smoking and hidradenitis suppurative; Acta Dermatovenerol Croat 28(1): 9-13.
- Kelly G, Prens E (2016) Inflammatory mechanisms in hidradenitis suppurativa. Dermatol Clin 34(1): 51-58.
- Arturo GGL, Florelvis PR, Alfonzo P, Miguel R (2020) Hidradenitis Suppurativa, sparo and bariatric surgery. Ann Cas Rep Rev ACRR-163.
- Ulhasan UR, Qureishi F, Hasan K, Khraisat N, Al Naimi AA, et al. (2021) Hidradenitis suppurativa: “a surgical update with review of literature. J Sur Anesth Res 2(1): 1-4.






























