Mesh Can Be Mess
Anant Pore and Ankush Sarwal*
Department of Medical and Health Science, University of Tata Medical Centre, India
Submission: March 05, 2019; Published: March 25, 2019
*Corresponding author: Ankush Sarwal, Department of Medical and Health Science, University of Tata Medical Centre, Kolkata, India
How to cite this article: Anant Pore, Ankush Sarwal. Mesh Can Be Mess. JOJ Dermatol & Cosmet. 2019; 1(4): 555568.
Abstract
The use of a prosthetic mesh to repair a tissue defect may produce a series of post-operative complications, among which infection is the most feared and one of the most devastating. The mesh related infections after hernia repair of up to 8% have been reported. Hence, the use of mesh should be with great care and caution. Strategies which are beneficial in reducing the incidences of mesh related infections after hernia repairs should be used in clinical practice.
Keywords: Prosthetic Mesh Tissue Defect Post-Operative Complications Devastating Hernia Repair Strategies
Introduction
Mesh use in abdominal hernia surgery is now a standard treatment. However, incidences of the mesh related infections after hernia repair of up to 8% have been reported [1-3]. The rate of infection is influenced considerably by underlying co-morbidity, mostly increased in patients with diabetes, immune suppression or obesity. Type of prosthetic mesh used can also influence the rate of infection. The rate of infection increases if the hernia repair is combined with other procedures like appendectomy, cholecystectomy, enterotomy [4,5].
Case Summary
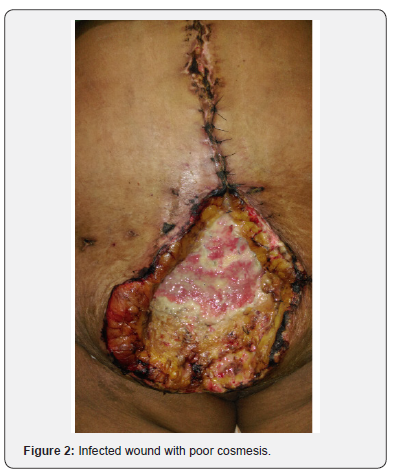
60-year-old obese lady with known comorbidity of diabetes was operated for incisional hernia with defect of size around 7-8cms. After closure of primary defect Overlay repair was done with propene mesh of Size 15x15 cm2. The immediate post-operative period was uneventful. She was discharged from the hospital after 7 days. However, after 2 weeks of her surgery, she developed localised swelling at one of the edges of the wound with pain & tenderness without any signs of septicaemia. Ultrasonography of local site showed localised collection of pus. This was drained, sent for culture & she was started with empirical Intravenous antibiotics. On day 3 of admission she developed high grade fever with entire wound dehiscence. In view of this higher generation IV antibiotics were started. She was haemodynamically stable, so initially she was treated conservatively with vacuum assisted dressing (Figure 1). Patient improved clinically and granulation was formed over the wound, so on day 10 Secondary suturing was done. However, on day 3 post-secondary suturing she again developed pus discharge from wound, culture was sent which showed Methicillin Resistant Staphylococcus Aureus andher condition deteriorated clinically (Figure 2). In view of this, decision was taken to remove the mesh. Entire Mesh was removed, and secondary suturing was done with panniculectomy. Post-surgery patient had an uneventful recovery and was discharged on 8th day post-surgery and doing well in follow up

Discussion
All abdominal wall hernia more than 2cm defect require surgical intervention. With use of Laparoscopic techniques in hernia repair, the cosmetic results have improved, and hospital stay has required. However, the use of mesh should be with great care and caution. The material used should be selected carefully. The most important point regarding prevention of mesh related infections is that foreign body reactions depend on the amount of prosthesis used [2,3]. Mesh infection results in increased patient morbidity because of secondary operations, impaired wound healing, functional loss of the abdominal wall, and significantly extended hospital stay. Besides there is lot of mental trauma involved for the patient due to poor cosmesis and prolonged treatment. As the use of synthetic materials for hernia repair is on the rise, the number of patients who will suffer from infections is likely to increase. Surgeons should try to minimise the area ofmesh that is introduced during the surgery and avoid any external skin contact with mesh, as the inserted foreign material is an ideal medium for bacterial colonisation [6]. Studies have shown that rinsing the wound with antibiotic containing solution inhibits the adhesion of bacteria to the surface of mesh as well as their growth [7]. Above mentioned strategies seen to be beneficial in reducing the incidences of mesh related infections after hernia repairs. However, no definitive recommendations can be made in favour of any approach. Mesh explantation is the only feasible option if mesh infection has developed as if the foci of infection, which in these cases is mesh itself is not taken care of then the world is highly unlike to heal and could lead to further morbidity and septicaemia..
Conclusion
Clinician should promptly consider the possibilities of mesh infections in any patient who has undergone hernia repair with mesh and has signs & symptoms of infections. Risk factors of prosthesis infection should be minimised to avoid mesh explantation as this has a long-standing morbidity and poor cosmetic results for the patient.
References
- Heniford BT, Park A, Ramshaw BJ, Voeller G (2000) Laparoscopic ventral and incisional hernia repair in 407 patients. J Am Coll Surg 190(6): 645-650.
- Kirshtein B, Lantsberg L, Avinoach E, Bayme M, Mizrahi S (2002) Laparoscopic repair of large incisional hernias. Surg Endosc 16(12): 1717-1719.
- Petersen S, Henke G, Freitag M, Faulhaber A, Ludwig K (2001) Deep prosthesis infection in incisional hernia repair: predictive factors and clinical outcome. European Journal of Surgery banner 167(6): 453-457.
- Sarwal A, Khullar R, Sharma A, Soni V, Baijal M, et al. (2018) Case report of ventral hernia complicating bariatric surgery. J Minim Access Surg 14(4): 345-348.
- Geisler DJ, Reilly JC, Vaughan SG, Glennon EJ, Kondylis PD (2003) Safety and outcome of use of nonabsorbable mesh for repair of fascial defects in the presence of open bowel. Dis Colon Rectum 46(8): 1118-1123.
- Deysine M (1998) Pathophysiology, prevention, and management of prosthetic infections in hernia surgery. Surg Clin North Am 78(6): 1105-1115.
- Troy MG, Dong QS, Dobrin PB, Hecht D (1996) Do topical antibiotics provide improved prophylaxis against bacterial growth in the presence of polypropylene mesh? Am J Surg 171(4): 391-393.






























