Abstract
Blurred vision following LASIK is commonly attributed to residual refractive error or regression, yet accommodative dysfunction is often underrecognized. This case report details a 31-year-old software engineer who developed intermittent blurred vision, eyestrain, and near-focusing difficulty post-LASIK despite achieving 20/20 uncorrected visual acuity immediately after surgery. Optometric evaluation revealed accommodative excess—characterised by reduced accommodative facility, elevated positive relative accommodation, and difficulty with plus lenses—likely intensified by prolonged near work and digital device use. Orthoptic findings supported this diagnosis, prompting a structured vision therapy regimen with home reinforcement over 24 in-office sessions. Therapy focused on enhancing convergence awareness, relaxing accommodation, and restoring fusional vergence dynamics. The patient experienced symptomatic improvement and retained an uncorrected visual acuity of 20/20 after the intervention. The accommodative function was further normalised and exhibited a decreased CISS score. This report highlights accommodative excess as a potential post-LASIK complication, emphasising the importance of preoperative orthoptic screening and individualized vision therapy. Assessing occupational visual demands and binocular function may enhance patient satisfaction and mitigate misattributed surgical dissatisfaction. A multidisciplinary, proactive approach may be crucial in refractive surgery workups, particularly among individuals with high near-work exposure.
Keywords: Accommodative dysfunction; Itrace; LASIK; LASIK – complications; Vision therapy
Introduction
Blurred vision after LASIK is a common concern among patients with myopia. This symptom can pose a challenge for clinicians because it may indicate to patients that the surgery was unsuccessful. Myopia after LASIK can occur due to a range of factors, including residual refractive error, myopia regression, and ectasia, which require further examination [1]. Moreover, post-LASIK binocular vision dysfunction, which is frequently disregarded, can markedly affect visual quality [2]. This case report describes a rare case of accommodative excess following LASIK surgery.
Case Presentation
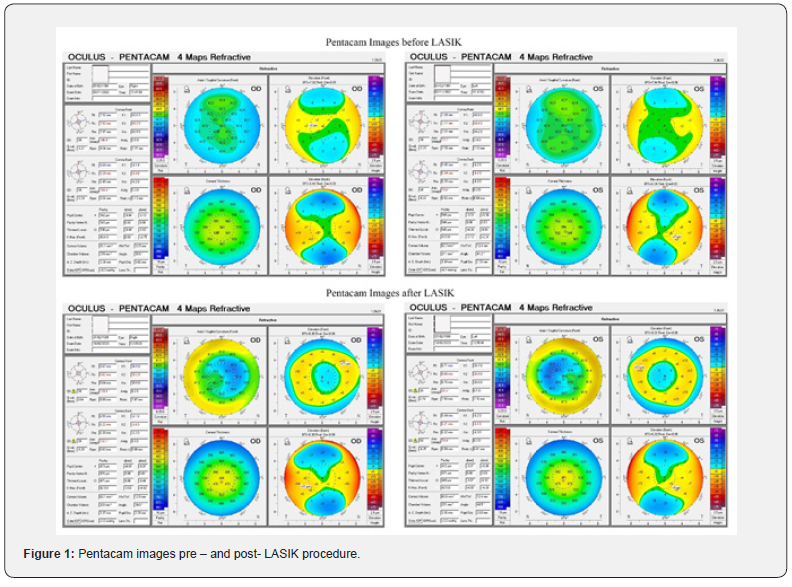
A 31-year-old male software engineer was presented for consultation regarding LASIK surgery. His ocular history included wearing glasses since the age of 15 years, and he experienced no ocular discomfort despite working with a computer for 14-15 hours every day. No significant systemic and family history was reported. In optometric evaluation, the distance visual acuity (Snellen) was measured at 20/20, N6 in each eye with a power of -6.75 DS/-0.50 DC x 90° in the right eye and -6.75 dioptre sphere (DS)/-0.50 dioptre cylinder (DC) x 90° in the left eye. The manifest refraction was not altered. After cycloplegic refraction, visual acuity was maintained at 20/20, in each eye with a prescription of -6.50 DS/-0.50 DC X 50° in the right eye and -6.75 DS/-0.50 DC X 90° in the left eye. Both the anterior and posterior segments appeared within normal limits. Normal Pentacam images (Figure 1) and corneal topography ruled out the Keratoconus. Consistent cycloplegic and manifest refraction led to avoiding the post-mydriatic test. Considering all assessment findings, femtosecond LASIK was recommended.
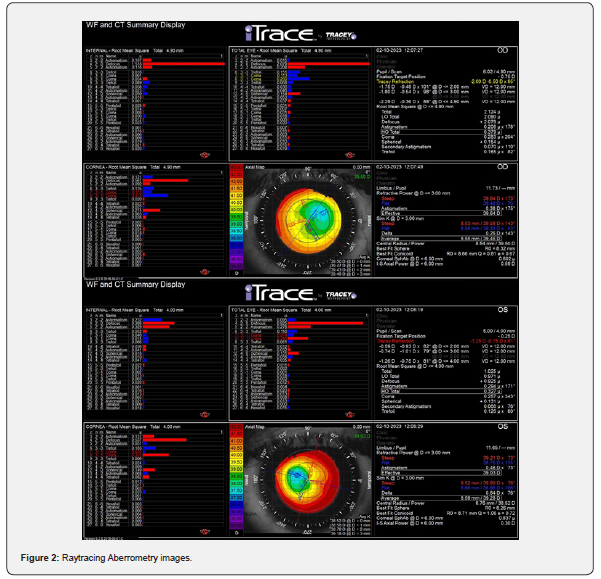
The patient underwent femtosecond LASIK without complications. The flap was created using an FS-200 femtosecond laser, and an EX-500 excimer laser was used to create the ablation. Postoperative visual acuity was 20/20. The patient was visited for postoperative follow-up after 1, and 3 months. However, 6 months after surgery, the patient experienced intermittent blurred vision, eye pain, difficulty in focusing on nearby objects, and headaches after the increased near-work activity for 15 days. The uncorrected visual acuity of each eye was 20/30. In manifest refraction, visual acuity improved to 20/20, N6 with the right eye -0.50 DS/-0.50 DC x 50° and the left eye -0.25 DS/-0.50 DC x 90°. In cycloplegic refraction, the visual acuity was 20/20 with -0.25 DS/-0.50 DC x 50° in the right eye and -0.25 DS/-0.50 DC x 90° in the left eye. In the slit-lamp examination, the flap appeared at a position with a clear interface. The Pentacam images showed normal ablation (Figure 1), and raytracing Aberrometry demonstrated increased internal aberration compared with the corneal aberration (Figure 2). Therefore, an orthoptic evaluation was recommended. An orthoptic evaluation revealed mild exophoria at the near, but the near point of convergence was normal. Additional tests revealed large positive relative accommodation, reduced accommodative facility, and difficulty with plus lenses (Table 1). The patient was diagnosed with accommodative excess and was motivated to receive in-office vision therapy for 24 sessions [3], 3 days a week, and home-based therapy daily for 40 minutes for 3 months (Table 2).


The primary objective of vision therapy was to enhance awareness of convergence and relaxation of accommodation, normalize the fusional vergence amplitude and facility at near, improve the accommodative amplitude, and develop the ability to stimulate and relax the accommodation. After 24 sessions, all accommodative and vergence parameters were normal, the uncorrected visual acuity improved to 20/20, N6, and the patient was able to focus on objects at every distance without spectacles. The manifest refraction appeared at -0.50 DC x 50° and -0.25 DC x 90° in the right and left eye, respectively. The CISS score reduced significantly. Subsequently, he continued the therapy for 3 months. After 6 months, the patient reported his satisfaction as the treatment outcome was maintained after this period.
Discussion
Accommodative excess is a less common anomaly that accounts for approximately 10% of the reported cases [4]. This condition is characterized by an overactive focusing mechanism that results in difficulty when focusing on distant objects after extended periods of near work [3]. Increased symptoms have been associated with the growing use of computers and digital devices among professionals [2]. As a software engineer, the patient works long hours on computers, which could be a contributing factor to the development of accommodative excess.
Clinicians often use the terms “accommodative excess” and “accommodative spasm” interchangeably, although they refer to different conditions. Clinical signs of accommodative spasm include pseudomyopia, variable retinoscopic reflex, fluctuating visual acuity, and miosis [3]. The definitive diagnosis is typically made through cycloplegic refraction or modified optical fogging. A notable reduction in myopia or a shift to minimim hyperopia upon relaxation of the condition confirms the diagnosis [5]. In this case, the cycloplegic refraction did not confirm pseudomyopia or accommodative spasm. However, the higher internal aberration from the raytracing aberrometer indicates optical imperfections, warranting an orthoptic evaluation.
Success in LASIK surgery depends on patient satisfaction and achieving optimal vision. Experiencing blurred vision within 6 months post – LASIK led the patient to consider residual refractive error and suspect the success of the procedure. After LASIK, changes in accommodation for near vision may require restimulation, potentially leading to overcompensation [6]. Zheng et al. [7] explored accommodation alterations 1 month after SMILE surgery, but these changes were not recorded [7]. Karimian et al. [8] noted increased accommodative facility among patients with myopia 1 month after photorefractive keratectomy [8]. Consistent with the findings of Liu et al. [9] & Fu et al. [10] both the amplitudes of accommodation and the accommodative facility were enhanced 1 month following the insertion of an iris-fixed phakic intraocular lens [9,10]. Thus, abrupt accommodation changes might normalize within a month. Nonetheless, patients reported discomfort 3 months after surgery, which was likely due to prolonged near-work activity rather than the surgery itself, leading to visual fatigue. Pre-existing accommodative dysfunction may have worsened gradually. 24 in-office vision therapy sessions help treat accommodative and binocular dysfunctions, developing the ability to relax accommodation, normalizing amplitude, and maintaining fusional vergence.
Conclusion
This case report underscores the necessity of evaluating occupational history and visual requirements in LASIK consultation to optimize postoperative outcomes. Extended work can cause vision problems and post-surgical complications. Therefore, orthoptic evaluation and vision therapy should be considered before LASIK to improve visual outcomes and mitigate risks.
Declaration
Data availability statement: The datasets used and analysed
during the current study are available from the corresponding author
on reasonable request.
Ethics approval: The need for Ethical approval was waived off by
the Narayana Nethralaya Ethics Committee for the case reports.
Consent to participate and publication: Informed consent to
participate and informed consent to publication were obtained
from the patient prior to submission.
References
- Sahay P, Bafna RK, Reddy JC, Vajpayee RB, Sharma N (2021) Complications of laser-assisted in situ keratomileusis. Indian Journal of Ophthalmology 69(7): 1658-1669.
- Muthu S, Jethani J, Annavajjhala S, Gupta S, Gupta K, et al. (2020) Integrating binocular vision assessment in refractive surgery work-up: Proposition and protocol. Indian Journal of Ophthalmology 68(12): 2835-2846.
- Scheiman M, Wick B (2008) Clinical management of binocular vision: heterophoric, accommodative, and eye movement disorders. Lippincott Williams & Wilkins.
- Cacho-Martínez P, García-Muñoz Á, Ruiz-Cantero MT (2010) Do we really know the prevalence of accomodative and nonstrabismic binocular dysfunctions? Journal of Optometry 3(4): 185-197.
- Manna P, Karmakar S, Bhardwaj GK, Mondal A (2023) Accommodative spasm and its different treatment approaches: A systematic review. European Journal of Ophthalmology 33(3): 1273-1286.
- García‐Montero M, Albarrán Diego C, Garzón‐Jiménez N, Pérez‐Cambrodí RJ, López‐Artero E, et al. (2019) Binocular vision alterations after refractive and cataract surgery: a review. Acta Ophthalmologica 97(2): e145-e155.
- Zheng K, Han T, Zhou X (2016) Accommodative changes after SMILE for moderate to high myopia correction. BMC Ophthalmology 16(1): 1-5.
- Karimian F, Baradaran-Rafii A, Bagheri A, et al. (2010) Accommodative changes after photorefractive keratectomy in myopic eyes. Optometry and Vision Science 87(11): 833-838.
- Liu L, Lü F, Wang Q, Xue A, Chen S, et al. (2010) Change of accommodative function in phakic eyes with iris-fixated phakic intraocular lens implantation. [Zhonghua yan ke za Zhi] Chinese Journal of Ophthalmology 46(7): 621-624.
- Fu J, Wang X, Wang N, Wang J, Zhao S (2013) Accommodation perimeters after phakic posterior chamber implantable contact lens implantation. [Zhonghua yan ke za Zhi] Chinese Journal of Ophthalmology 49(7): 633-636.






























