Digital Angioleiomyoma: A Case Report
David J Goyette*
Podiatric Surgeon, Essex Partnership University Foundation NHS Trust, United Kingdom
Submission: February 10, 2024; Published: February 22, 2024
*Corresponding author: David Goyette, BSc (HONS) MSc FRCPodS, Department of Podiatric Surgery, Rochford Hospital, Union Lane, Castle Road, Rochford, Essex, SS4 1RB, UK Email: david.goyette@nhs.net
How to cite this article: David J G. Digital Angioleiomyoma: A Case Report. JOJ Case Stud. 2024; 14(4): 555893.. DOI: 10.19080/JOJCS.2023.14.555893.
Abstract
The objective of the article is to raise the index of clinical suspicion of these small, solitary, slow growing, and usually painful benign tumours amongst healthcare professionals who manage foot and ankle pathology. Thus, aiding their inclusion in the differential diagnoses of soft tissue tumours, along with ganglion cyst, giant cell tumour, schwannoma and bursa. The author recounts a case of digital angioleiomyoma and outlines typical signs, symptoms, imaging and histopathological findings. Definitive diagnosis is via histopathology after in toto excision. Recurrence after excision is rare.
Keywords: Angioleiomyoma; Digital angioleiomyoma; Tumour; Foot
Abbreviations: mm: Millimeters; cm: Centimeters; MRI: Magnetic Resonance Imaging; PIPJ: Proximal Interphalangeal Joint
Introduction
Leiomyoma are slow growing benign neoplasms of smooth muscle. They are characterised by the smooth muscle of origin [1,2]. Superficial, e.g. piloleiomyoma arise from the smooth muscle of erector pili muscles in skin. Genitoleiomyoma from vulvar, scrotal or areolar smooth muscle and Vascular or angioleiomyoma originating from vascular smooth muscle of the tunica media of small veins [1-4].
Angioleiomyoma are common throughout the body. Accounting for 5% of all benign soft tissue neoplasms, with 89% of cases present in the extremities. Of which, 66-71% occur in the lower extremity and 22-29% in the upper extremity [5,6], They represent 0.2% of cases of soft tissue tumours occurring in the foot, with the heel being the most common location [2,7]. However, digital angioleiomyoma are rarer accounting for only 9% of pedal cases, with less than 20 cases previously described [2,6,8].
Although cases affecting patients between 12 and 80 years of age appear in the literature, around two thirds of cases occur between the 4th and 6th decades [2,6,8].
Angioleiomyoma affect males to females at a ratio of 1:1.7. A tenfold increased incidence in east Africans compared to Caucasians living in the same temperate climate is noted [9]. However, no direct genetic associations for the development of angioleiomyoma exist [10].
Postulation on the pathogenesis of angioleiomyoma has included minor trauma, hormonal changes in pregnancy; particularly altered oestrogen levels, infection, arteriovenous malformation, venous stasis and traumatic venous congestion [10,11].
Masses are small, typically less than 2 centimetres in diameter, well-defined, often encapsulated, solitary ovoid lesions with glistening yellow, pink, grey, white, silver and brown colouration separately described [2,5,6,10,12].
Four histopathological sub types exist. All are composed of varying concentrations of bundles of eosinophilic smooth muscle cells with cigar or spindle shaped nuclei that stain positively for smooth muscle actin. These surround vascular channels of varying sizes. They exhibit moderately low overall mitotic activity and cellularity with no evidence of atypia [2,5,10,11,13,14]. Reports of intra tumour calcification, mature fat cells, hyalinisation, myxoid changes, organising thrombus and lymphocytic infiltration exist [10,11,14]. Cytology findings following fine needle aspiration show uniform spindle cells mixed with smooth muscle, collagen, macrophages and fat cells. These findings are insufficient to make a diagnosis [11].
Clinically, angioleiomyoma present as solitary, firm, small (<2cm), slow growing and long standing, mobile, sub cutaneous nodules [8,11,14]. Postulated to be due to mass effect, secondary to ischaemic change following contraction of smooth muscle and local nerve compression, pain is a symptom in around two thirds of cases. Exposure to cold and pressure including shoe gear can also elicit symptoms. [2,5,8,11,13,16]. Increasing size with physical activity is possible [8,11,14]. The slow growing nature of the tumours is highlighted by a delay of 4-10 years between subjective onset and excision [2,8].
The vast majority of authors recommend that excision with histopathology is the standard of care for diagnosis and exclusion of malignancy [8,10,11,14,16]. Excision has a good prognosis with low recurrence rates around 1:250 [5]. If recurrence occurs, repeat examination of the original histopathology to rule out leiomyosarcoma should be undertaken [10]. Malignant change is rare with only a few cases of leiomyosarcoma reported in the literature [1].
4.1. Imaging
Aside from increased soft tissue intensity at the site of the tumour, plain radiographs are usually unremarkable [14]. In some cases, secondary compression phenomenon of bone of the intermediate phalanx of a lower limb digital mass can appreciated on X –ray [8]. Ultrasound examination shows; well defined, ovoid, homogenous, non-compressible mass. Descriptions of anechoic and hypoechoic areas alternating with isoechoic regions are found in the literature. Feeding arteries may be visualised as tubular structures with numerous intra lesion branches [11,17,18].
Magnetic resonance imaging (MRI) changes are consistently reported and secondary to varied proportions of component smooth muscle cells and blood vessels. T1 images typically show well-circumscribed homogenous masses, which are isointense to skeletal muscle. A thin hypointense capsule surrounding the lesion are often present on both T1 and T2 images [11,12,14]. Within the tumour heterogeneous, hyper and isointense areas are visible on T2 and STIR images. Hyperintense areas correspond to smooth muscle and are multiple linear or branching in appearance. These areas show strong enhancement on intra venous contrast. Areas of tough fibrous tissue or intravascular thrombi correspond to isointense areas. These do not show enhancement on contrast [11,12,14]. MRI cannot differentiate histopathological sub types [11,12].
Case Report
A 62-year-old male patient presented in clinic describing a 3-year worsening history of pain and soreness from a slow growing mass affecting the dorsal aspect of his left third toe. The mass had been present for five years prior to his discomfort. Symptoms were worse with walking and wearing safety footwear. Relief achieved from removing footwear. The patient subjectively scored the pain at 8/10 on visual analogue scale when wearing safety shoes for work. No subjective colour change or swelling noted, he had noticed gradual enlargement of the mass. No direct trauma history recalled. The pain caused him to limp and utilise oral analgesia. An occasional tingling pain in the digit could cause sleep disturbance. Embarrassed by the appearance of the mass, the patient had avoided taking his grandchildren swimming. No previous treatment or imaging had taken place. When questioned, the patient’s idea was that the mass was a ganglion; his main concerns were the discomfort as well as the appearance. His expectation was to achieve a reduction of symptoms. He felt that this warranted an operation.
Medical history was remarkable for hypertension, asthma and a history of hepatitis A. Previous surgery: laparoscopic cholecystectomy and left lateral ankle ganglion excision.
Medication: Salbutamol, Beclometasone with formoterol inhaler and Ramipril 2.5mg.
No known allergies.
On examination, vascular and neurological supply to the distal lower limb was intact. Skin was of normal colour, temperature and texture. Patient was using a well-fitting running shoe.
Musculoskeletal examination was grossly normal. At the level of the proximal interphalangeal joint (pipj) of the left third toe, a well-defined, ovoid, rubber, partially fluctuant, non-emptying, non-tender, non-pulsatile soft tissue mass was present. Differential diagnoses included, ganglion cyst and giant cell tumour of tendon sheath. Management options discussed, included do nothing, needle biopsy and in toto excision with histopathology. He considered these whilst waiting for the results of plain radiographs and ultrasound examination.
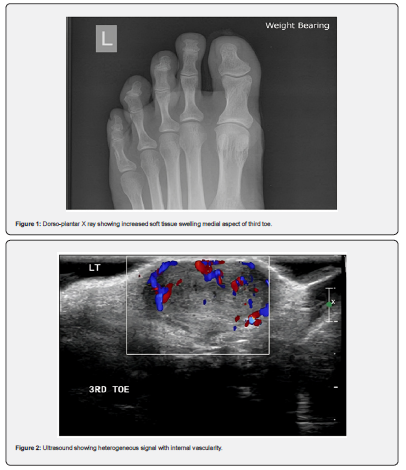
Dorso-plantar radiograph (Figure 1) highlighted mild increased soft tissue swelling on the medial aspect of the left third toe at the level of the proximal interphalangeal joint. Ultrasound (Figure 2) revealed, a large, 1.9cm x 1.3cm lesion showing internal vascularity overlying the dorsal aspect of the proximal interphalangeal joint of the left third toe. Magnetic resonance imaging (MRI) was advised for further characterisation.
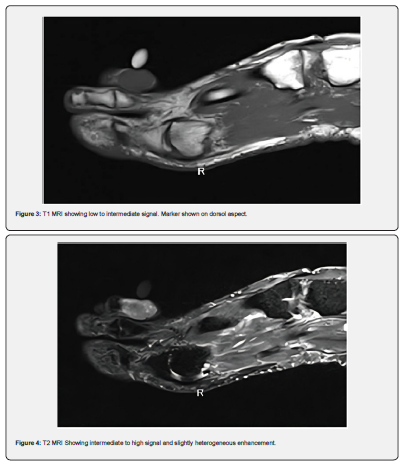
Measuring 0.9 x 1.1 by 1.8 cm a soft tissue mass at the level of the left third pipj could be visualised on MRI. This gave low to Intermediate signal on T1 (Figure 3), intermediate to high on T2 STIR imaging with slightly heterogeneous enhancement. (Figure 4) Bone marrow was normal on all sequences. Radiology reported, “Appearances are nonspecific and could represent a giant cell tumour of the tendon sheath or other benign pathology.”
The patient elected for excision with histopathology. Under regional ankle anaesthesia with ankle tourniquet and standard skin preparation and draping. A longitudinal double elliptical skin incision centred over the mass was performed. Blunt dissection revealed a silver/white well-demarcated mass surrounded by a thin, weakly adhered capsule. No vascular or neurological structures supplied the mass. Following in toto excision, a non-absorbable suture placed at the cephalic end of the mass aided orientation for histopathology. Inspection of the structures adjacent and deep to the mass found them normal and healthy. Skin closure with simple interrupted 3-0 sutures followed copious saline irrigation. Post-operative progress was uneventful, and sutures removed after two weeks with return to normal footwear and work. Follow up two months later was unremarkable with the patient pain free. He had returned to swimming.
Results and Discussion
Histopathology described the samples macroscopic findings as “single lobular greyish brown soft tissue measuring 18mm x 13mm x 10 mm” and microscopically “an angioleiomyoma that is seen reaching the excision margin focally. No malignancy is present.” Concluding, “Lesion left third toe: Angioleiomyoma.”
Whilst relatively common in the lower extremity and the foot, the rarer, digital location in this instance is worthy of reporting. The long-standing, slow growing nature of the lesion combined with worsening pain experienced by the patient are consistent with descriptions in the literature. Imaging is unable to confer definitive diagnosis. However, the findings in this case, particularly MRI are also in keeping with previous descriptions. Definitive diagnosis achieved via histopathology and recurrence is rare after excision.
Clinicians should consider Angioleiomyoma in the differential diagnoses of solitary soft tissue masses within the foot. Particularly when, long-standing and slow growing tumours are accompanied by characteristic mixed hyper and iso intense areas on T2 MRI.
Acknowledgement
Mr J A Nandlal MSc FRCPodS Consultant Podiatric Surgeon.
References
- Dominguez-Cherit J, Brandariz A (2003) Distal digital angioleiomyoma: a case report and review of the literature. International Journal of Dermatology 4(2): 141-143.
- Hammond MI, Miner AG, Pilang MP (2017) Acral and digital angioleiomyomata: 14-year experience at the Cleveland Clinic and a review of the literature. Journal of Clinical Pathology 44(4): 342-345.
- Enzinger FM, Weiss SW (1995) Soft Tissue Tumours. (3rd edn), St Louis: CV Mosby.
- Savage, P, Zyzda M, Kruse DL, Stone PA (2019) Leiomyoma of the Foot: A Case Report and Literature Review. The Journal of Foot and Ankle Surgery 58(3): 573-576.
- Morimoto (1973) Angiomyoma: A clinicopathologic study. Medical Journal of Kagoshima University 24: 663-683.
- Hachisuga T, Hashimoto H, Enjoji M (1984) Angioleiomyoma. A clinicopathologic reappraisal of 562 cases. Cancer 54: 126-130.
- Berlin SJ (1995) Statistical analysis of 307,601 tumours and other lesions of the foot. Journal of the American Podiatric Medical Association 85(11): 699-704.
- Yates BJ (2001) Angioleiomyoma: Clinical Presentation and Surgical Management. Foot and Ankle International 22(8): 670-674.
- Sweeney J, Keating S (1983) Angioleiomyoma. Journal of Foot Surgery 22(1): 21-22.
- Santucci A, Albini M, Ventura A, De Palma L (2000) Clinical and histological features of vascular leiomyoma of the foot: case report and literature review. Foot and Ankle Surgery 6(4): 267-274.
- Ramesh P, Annapureddy SR, Khan F, Sutaria PD (2004) Angioleiomyoma: a clinical, pathological and radiological review. International Journal of Clinical Practice 56(6): 587-591.
- Gupte C, Butt SH, Tirabosco R, Saifuddin A (2008) Angioleiomyoma: magnetic resonance imaging features in ten cases. Skeletal Radiology 37(11): 1003-1009.
- Katenkamp, D, Komeshi H, Langbein L (1988) Angiomyome: pathologische-anatomisch analyse von 229 fallen. Zentraib Allg Pathologische-Anatomisch 134(4-5): 423-433.
- Szolomayer LK, Talusan PG, Chan W, Lindskog DM (2017) Leiomyoma of the Foot and Ankle. Foot and Ankle Specialist 10(3): 270-273.
- Gajanthodi S, Rai R, Chaudhry RK (2013) Vascular Leiomyoma of Foot. Journal of Clinical and Diagnostic Research 7(3): 571-572.
- Buddemeyer K, McKissack HM, Farnell C, Robin JX, Qarmali M, et al. (2018) Leiomyoma of the Foot: A Case Report. Cureus 10(10): e3419.
- Chávez-López M, Reyna-Olivera G, Pedroza-Herrerac G (2014) Vascular Leiomyoma of the Foot: Ultrasound and Histologic. Reumatologica Clinica 10(5): 342-343.
- Sardanelli F, Renzetti P, Nardi F, Cittadini G, Tanara G, et al. (1996) Imaging of Angioleiomyoma. Journal of Clinical Ultrasound 24(5): 268-271.






























