Joubert Syndrome in a Child with Cystic Renal Disease and Nystagmus: A Case Report
Jovaria Ehsan*, Saima Shan and Hajra Sajjad
Associate Radiologist, Federal Government Polyclinic Hospital, Pakistan
Submission: December 19, 2022; Published: January 11, 2023
*Corresponding author: Jovaria Ehsan, Associate Radiologist, Federal Government Polyclinic Hospital, Islamabad, Pakistan
How to cite this article: Jovaria E, Saima S, Hajra Sajjad. Joubert Syndrome in a Child with Cystic Renal Disease and Nystagmus: A Case Report. JOJ Case Stud. 2023; 14(1): 555878. DOI: 10.19080/JOJCS.2023.14.555878.
Abstract
Joubert syndrome is a rare neurodevelopmental pathology with a spectrum of findings characterized by compromised vision and attention with disability of cognitive skills associated with cystic renal disease and hepatic fibrosis. Radiologically, it is described as having cerebellar vermian abnormalities with characteristic molar tooth appearance of mid brain along with visceral involvement. It is amongst the rarest autosomal recessive inherited disease predominantly affecting male children with less than 250 cases reported worldwide. We present a case of a four-year male child with delayed developmental milestones and hypotonia. Radiological investigations revealed cystic renal disease and hepatic fibrosis on Ultrasound abdomen with cerebellar vermian aplasia and characteristic molar tooth sign on MRI brain.
Keywords: Joubert syndrome; Nystagmus; Molar tooth sign
Introduction
Joubert syndrome is an uncommon hereditary disease manifested in infants as ataxia, nystagmus and delay in achieving milestones [1]. Moreover, other features may accompany Joubert syndrome including cystic renal disease, hepatic fibrosis, skeletal involvement and retinal involvement, which are categorized as Joubert syndrome related disorders (JSRD) [2]. The disorder is named after French neurologist Marie Joubert who first described its clinical aspects in 1968 in four siblings [1-3].
The incidence of the syndrome is approximately calculated out to be 1/80,000 to 1/100,000 live births [3]. It has predilection for male infants [1]. On average, the diagnosis is established at 33 months of age [4]. Our patient was a four years old child who had developmental delay with ataxic gait and nystagmus. He was diagnosed as Joubert syndrome with related disorders (JSRD) on a series of radiological investigations. Only few of such cases have been reported worldwide, with none of them reported from Pakistan.
Case Report
A four years old male child was referred to Department of Radiology from the Paediatrics department for ultrasound abdomen. He primarily presented with altered sensorium, hematuria and vomiting for one day.
On examination, the child was pale, febrile and tachypneic. He had reactive pupils bilaterally with nystagmus (Figure 1).
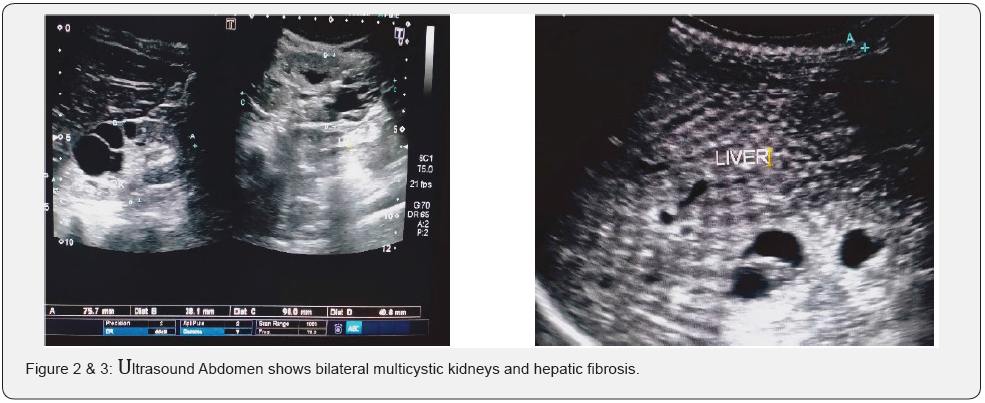
The child had delayed developmental milestones with poor suckling reflex, inability to hold the neck and crawling until the age of one year. He had delayed motor skills with ataxic gait, ankle clonus and upgoing planters. Cardiovascular, respiratory and abdominal examinations were unremarkable. On biochemical evaluation he had deranged renal and liver function tests. On ultrasound abdomen, he had enlarged multicystic kidneys with urinary tract infection and hepatic fibrosis (Figure 2 & 3).
CT scan and MRI brain was carried out to find out the cause of delayed milestones, hypotonia and nystagmus. Both revealed cerebellar vermian agenesis with dilated fourth ventricle and iconic Molar Tooth sign characteristic of Joubert syndrome (Figure 4 & 5).
Considering the clinical and radiological aspects of this child, the diagnosis of Joubert syndrome subtype with renal (JS-R) and hepatic (JS-H) defects was made.
The child has two elder male siblings, the elder one being 12 years old with delayed developmental milestones and is deaf, dumb and cognitively impaired, the younger one being 9 years old is healthy with developmental milestones consistent for his age.

Discussion
Joubert syndrome is an infrequent disease typically characterized by key diagnostic criteria including infantile hypotonia/ataxia, cognitive impairment and characteristic molar tooth sign on MRI brain [1-3]. Molar tooth sign is a radiological hallmark signifying cerebellar vermian and brainstem developmental abnormality [3,4]. A high resolution MRI brain with 3mm cuts is usually advised for visualizing the signs of Joubert syndrome [5]. It is seen in axial cuts of cerebral CT and MRI. Our patient fulfilled the diagnostic criteria in its entirety with agenesis of cerebellar vermis and dilated fourth ventricle.
Patients with Joubert syndrome additionally, may show tachypnea or periods of apnea in infancy due to brainstem involvement [1,6]. Our patient however had only one past history of hospital admission with a respiratory tract infection. He had an unremarkable respiratory system examination.
Ocular involvement in Joubert syndrome is still debatable. Researches done worldwide show that majority of the affected children had disconjugate gaze and nystagmus. Some of the children also had retinal defects [5-7]. Nystagmus in some of the children resolves with advancing age [3], however our patient had persistent nystagmus at 4 years of age starting from birth. No retinal defect was found at opthalmological examination.
Joubert syndrome is found along with renal involvement in 23- 32% population affected by the syndrome and mostly manifests as cystic kidney disease often worsening into end stage renal disease over a period of a decade [2,5]. Our patient had bilateral enlarged kidneys with multiple cysts replacing the normal renal parenchyma.
Few of the patients with Joubert syndrome may have hepatic involvement manifesting as hepatic fibrosis.
Such patients have deranged liver function tests also [1]. According to Brancati [8], early onset of hepatic involvement may be manifested as hepatosplenomegaly. Our patient had changes of early hepatic cirrhosis on Ultrasound with deranged liver function tests.
An umbrella term “Joubert syndrome and related disorder” (JSRD) is recently introduced term that encompasses all the disorders showing molar tooth sign with ocular and visceral involvement [2,6,9]. Phenotypic presentations of Joubert syndrome is categorized into 6 six subtypes: JS with ocular defect (PureJS), JS with renal defect (JS-R), JS with hepatic defect (JS-H), JS with ocular defect (JS-O), JS with oculorenal defect (JS-OR), JS with orofaciodigital defects (JS-OFD) [2,6,8].
Prenatal diagnosis of Joubert syndrome is possible as early as 11 weeks with chorionic villus sampling [10]. In addition fetal anomaly scans done before 24 weeks can also help in diagnosis.
Mother of our patient was clueless of her child as she never underwent an anomaly scan. An obstetric scan done at 32 weeks revealed isolated dilated 4th ventricle. She was advised fetal MRI but didn’t proceed due to financial constraints.
Proper rehabilitation services for cognitive and speech development is required to improve quality of life [11], hence the management must be started timely to prevent further complications. Parents of our patient were counselled in detail about the prognosis and symptomatic treatment of the child [12].
Conclusion and Recommendation
Early and timely diagnosis is vital for patients with Joubert disease with enhanced focus on elevating quality of life by preventing renal and hepatic complications.
References
- Elhassanien AF, Alghaiaty HA (2013) Joubert syndrome: Clinical and radiological characteristics of nine patients. Annals of Indian Academy of Neurology 16(2): 239-244.
- Poretti A, Huisman TA, Scheer I, Boltshauser E (2011) Joubert syndrome and related disorders: spectrum of neuroimaging findings in 75 patients. American Journal of Neuroradiology 32(8): 1459-1463.
- Parisi MA (2019) The molecular genetics of Joubert syndrome and related ciliopathies: The challenges of genetic and phenotypic heterogeneity. Translational Science of Rare Diseases 4(1-2): 25-49.
- Hurtado P, Pachajoa H (2010) Molar tooth sign: a characteristic image in Joubert syndrome. Neurologia (Barcelona, Spain) 25(2): 140-141.
- Parisi MA (2009) Clinical and molecular features of Joubert syndrome and related disorders. In: American Journal of Medical Genetics Part C: Seminars in Medical Genetics 2009 Nov 15. Hoboken: Wiley Subscription Services, Inc., A Wiley Company, Vol. 151, No. 4, pp. 326-340.
- Maria BL, Hoang KB, Tusa RJ, Mancuso AA, Hamed LM, et al. (1997) Joubert syndrome revisited: key ocular motor signs with magnetic resonance imaging correlation. Journal of Child Neurology 12(7): 423-430.
- Brancati F, Dallapiccola B, Valente EM (2010) Joubert Syndrome and related disorders. Orphanet Journal of Rare Diseases 5(1): 20.
- Devi AR, Naushad SM, Lingappa L (2020) Clinical and molecular diagnosis of Joubert syndrome and related disorders. Pediatric Neurology 106: 43-49.
- Doherty D, Glass IA, Siebert JR, Strouse PJ, Parisi MA, et al. (2005) Prenatal diagnosis in pregnancies at risk for Joubert syndrome by ultrasound and MRI. Prenatal Diagnosis: Published in Affiliation with the International Society for Prenatal Diagnosis 25(6): 442-447.
- Bachmann Gagescu R, Dempsey JC, Bulgheroni S, Chen ML, D'Arrigo S, et al. (2020) Healthcare recommendations for Joubert syndrome. American Journal of Medical Genetics Part A 182(1): 229-249.
- Akhtar A, Hassan SA, Falah NU, Khan M, Sheikh FN (2019) Joubert syndrome: a rare radiological case. Cureus 11(12): e6410.
- Romani M, Micalizzi A, Valente EM (2013) Joubert syndrome: congenital cerebellar ataxia with the molar tooth. The Lancet Neurology 12(9): 894-905.






























