Effect of Sokeikakketsuto Combined with Interventional Treatment on Low Back Pain - A Case Report
Hiroko Nakamura1,2, Mayako Uchida3, Yuko Miyamae4, Shinnosuke Kurata1, Kenji Shin1,5, Daisuke Kobayashi1, Takehiro Kawashiri1 and Takao Shimazoe1*
1Department of Clinical Pharmacy and Pharmaceutical Care, Graduate School of Pharmaceutical Sciences, Kyushu University, Japan
2Nakamura Pharmacy Ltd., Nogata, Japan
3Department of Education and Research Center for Pharmacy Practice, Faculty of Pharmaceutical Sciences, Doshisha Women's College of Liberal Arts, Japan
4Miyamae Pain Clinic, Sakai, Osaa, Japan
5Department of Pharmacy, Iizuka Hospital, Japan
Submission: June 20, 2022; Published: July 01, 2022
*Corresponding author: Takao Shimazoe, Department of Clinical Pharmacy and Pharmaceutical Care, Graduate School of Pharmaceutical Sciences, Kyushu University & Nakamura Pharmacy Ltd., Nogata, Fukuoka, Japan
How to cite this article: Hiroko N, Mayako U, Yuko M, Shinnosuke K, Kenji S. Effect of Sokeikakketsuto Combined with Interventional Treatment on Low Back Pain - A Case Report. JOJ Case Stud. 2022; 13(4): 555869. DOI: 10.19080/JOJCS.2022.13.555869.
Abstract
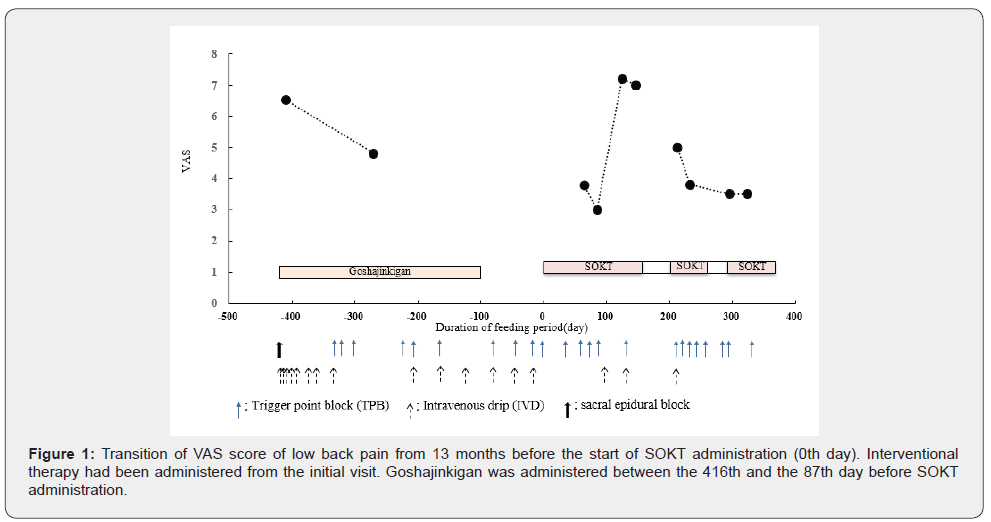
Analgesic and interventional treatments, such as trigger point block (TPB) injections, are used for chronic pain; however, in some cases, they are not effective, particularly for low back pain. Kampo medicine, a type of oriental medicine, may be effective in such cases. Sokeikakketsuto (SOKT) is a Kampo medicine with an analgesic effect. SOKT consists of 17 herbal medicines. In the present study, we report the case of a patient with chronic back and lower limb pain who received monthly TPB treatment with goshajinkigan for 1 year. This was changed to combined treatment with SOKT instead of goshajinkigan because the patient’s visual analogue scale (VAS) score deteriorated. The VAS score improved 2 months later. Continuous administration of the combined treatment maintained this improvement. Our findings suggest that SOKT improves the quality of life of patients with chronic low back pain who experience insufficient efficacy of their current treatment or an inability to continue treatment. Furthermore, Kampo medicine has relatively few side effects and interactions with other medical treatments.
Keywords: Sokeikakketsuto; Low back pain; Interventional therapy; Visual analogue scale; Kampo medicine
Introduction
In Japan, many patients suffer from low back pain, which reduces quality of life. In the Comprehensive Survey of Living Conditions [1] in 2019, low back pain was the most common symptom in men and the second most common symptom after stiff shoulders in women with illness or injury. In Japanese pain clinics, nerve blocks (epidural blocks, cateran epidural injections, various nerve blocks, and trigger point blocks [TPB]) are performed for moderate or severe pain in patients. In addition, alprostadil is used in cases where blood failure is suspected, depending on the patient’s general condition and the severity of the pain. A preparation containing an extract from inflamed cutaneous tissue of rabbits inoculated with vaccinia virus was inoculated, and vitamins B1, B6, and B12 preparations were made by intravenous infusion.
Nerve blocks for low back pain in patients with high visual analogue scale (VAS) scores or nocturnal pain are administered in both the acute and chronic phases. Drug treatment often involves nonsteroidal anti-inflammatory drugs, an extract from inflamed cutaneous tissue of rabbits inoculated with vaccinia virus, pregabalin, prostaglandin E1 derivatives, and Kampo medicines. Currently, eight types of Kampo medicines are used for low back pain in Japan, namely hachimijiogan, tokishigyakukagoshuyushokyoto, sokeikakketsuto (SOKT), tokakujokito, goshakusan, tsudosan, goshajinkigan, and ryokyojutsukanto. However, Goshajinkigan is reported that the Kampo has few effects in lowback pain of spinal diseases [2]. Among these, SOKT, which consists of 17 herbal medicines, is administered when patients experience low back and lower limb pain with feelings of coldness, arthralgia, and/or myalgia [3]. "Wan-Bing-Hui-Chun", a classical Chinese medicine book, advises that SOKT be used for patients with nocturnal pain. For patients with low back pain, multiple treatments are often used in combination; thus, it is difficult to consider the efficacy of a single agent. A literature search revealed only one case report of SOKT successfully treating chronic lower back and limb pain of the spinal column stenosis in a pain clinic [4]. In the Miyamae Clinic, there was no improvement with TPB injections of Neo Vitacain® and Carbocaine®; however, we identified one case that reported symptom improvement using SOKT instead of goshajinkigan used in combination. Kampo medicine is well established, and its prescription is tailored to the patient’s individual condition; however, evidence regarding SOKT has not been fully evaluated for the effects in chronic low back pain. In this case, interventional therapy was ineffective; however, additional SOKT treatment showed higher efficacy.
Case Presentation
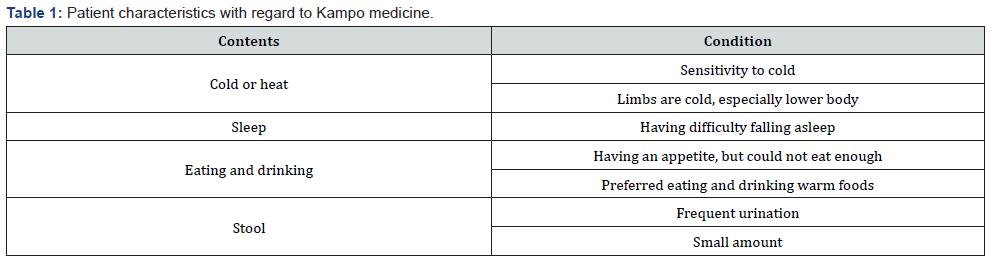
We present a case of a 79-year-old woman with a history of chronic back and lower limb pain. At 70-years old, she hurt her lower back and experienced numbness in her lower leg after being forced to swim. She was diagnosed as spinal canal stenosis, and underwent surgery at hospital A. The data of the MRI were not available from hospital A. At the age of 76 years, she had a compression fracture and worsening lower back and leg pain. She underwent a nerve block and drug treatment; however, her symptoms did not improve, and she underwent a vertebral fixation operation using bolts. Postoperatively, numbness appeared in an area below her groin, and the numbness below the knee was reduced 1 year postoperatively; however, the below the knee numbness remained. At the age of 78, she visited Miyamae Clinic because of pain and numbness in her legs. She complained of worsening lower limb pain, particularly before going to bed. The VAS score was 6.0-9.0. Loxonin® was prescribed at hospital A. At her initial visit, she was sensitive to cold and her limbs, especially the lower body, were cold. She had poor sleep. She had an appetite but was unable to eat sufficient quantities. She frequently urinated, and the quantity of her stool was small (Table 1). The attending physician diagnosed her with postoperative lumbar chronic pain and treated her with sacral epidural block injection and intravenous drip (IVD) injection with alprostadil, Neolamin® 3 B, and Neurotropin®. Her VAS score improved to 5.0 four days after the initial diagnosis. However, her lower back, buttock, and lower limb pain worsened, and IVD was performed using drugs, such as alprostadil, when the numbness was strong. Two months after the initial diagnosis, the left lower back pain deteriorated, and TPB with Neo Vitacain® and Carbocain® was started. Administration was continued every 1-2 months. With regard to drug treatment, goshajinkigan was used from the first visit because of numbness; however, her VAS score deteriorated, and it was discontinued. One year and 1 month after the initial diagnosis, she was diagnosed with recurrence of spinal canal stenosis at hospital A. Coldness and nocturnal pain of the lower limbs were observed, and SOKT (5.0g/day) was initiated. Generally, the daily dose of SOKT is 7.5g/day but a lower dose was used because of her weak gastrointestinal state.Six months before SOKT administration, the VAS score was 7.5. TPB and IVD were performed five times in 6 months, and the VAS score was 8.5 before SOKT administration. TPB was performed on the 32nd, 51st, and 64th day after the start of SOKT. On the 64th day, her lower back pain had a VAS score of 3.8. TPB was also performed on the 85th day, and improvement was maintained with low back pain (VAS score =3). On the 99th day, IVD of alprostadil and other drugs was performed because of numbness. TPB was not performed for pain because her VAS score was 4.0. On the 125th day of administration, her VAS score was 7.2, indicating deterioration as she carried a heavy load. Thereafter, Kampo medicine was stopped as she felt unstable upon waking-up in the morning, and her physician judged that the instability was due to insomnia and fatigue due to family care. Forty-five days after drug withdrawal, she complained of pain from her buttocks to her lower leg, which worsened at night. Her condition deteriorated (VAS score = 7.3), and SOKT was resumed with TPB administration. On the 8th day after resumption, the VAS score was decreased to 5.0. On the 29th day, TPB was administered and the VAS score was 3.8. On the 92nd and 120th days, TPB was administered, and the VAS score was 3.5; it continued to improve (Figure 1).
Discussion
The Longitudinal Cohorts of Motor System Organ, a large-scale cohort study by Yoshimura et al. [5] reported that the number of the patients with low back pain was 27.7 million (male: 12.1 million, female: 15.6 million) aged over 40 years in Japan [5]. Despite treatment recommendations, many patients suffer from both acute and chronic low back pain. Some drugs are weakly recommended, such as serotonin-noradrenaline reuptake inhibitors, weak opioids, agents extracted from inflamed rabbit skin inoculated with vaccinia virus, non-steroidal anti-inflammatory drugs, and acetaminophen, in the Japanese clinical guidelines [6] to address low back pain. The use of strong oral opioids is not recommended because of overdose and dependency. Moreover, although strong opioids were evaluated in some reports, they were not administered under the Japanese health insurance system, and side effects compelled patients to halt treatment with these drugs. However, the guidelines recommend nerve block injections for chronic low back pain.
At the Miyamae Pain Clinic, nerve block injection is recommended in patients with a VAS score of more than 5.0 or night-time pain. Clinically, SOKT may be prescribed to patients experiencing insufficient efficacy of their current treatment or blood stasis.
Zhang et al. [7] reported that a decoction of liquorice root and Paeoniae radix, which are components of SOKT, reduced the excessive expression of silent information regulator 1 of chronic construction disorder in neuropathy model rats; thus, these decoctions could attenuate mechanical allodynia and thermal hyperalgesia in a dose- and time-dependent manner [7]. Our previous study showed that SOKT inhibited oxaliplatin- and bortezomib-induced neuropathy in rats [8]. Furthermore, Gauchan et al. [9] reported that oxaliplatin induced a decrease in the blood flow rate and that neuropathy was improved by the recovery of the blood flow rate [9]. These results suggest that blood flow is involved in neuropathy. Bortezomib also induces mechanical, but not heat, stimulation-induced neuropathy. Moreover, bortezomib does not influence motor and autonomic nerves [10]. In this case, spinal canal stenosis was diagnosed, and the patient had low back pain due to compulsion of the spinal cauda equina nerve. Prostaglandin E1 preparations are used in mild cases; thus, the attending physician administered alprostadil by injection in the present case. Goshajinkigan is often used to treat numbness in the lower body. However, in this case, the combined use of goshajinkigan, TPB, and alprostadil improved numbness and swelling, but the improvement in pain was insufficient. VAS score decreased to 4.8, but thereafter, it increased to 9.0. VAS did not change; therefore, goshajinkigan was discontinued. As mentioned before, the effect of goshajinkigan is insufficient for low back pain and numbness of the lower limbs in spinal diseases [2], and so, goshajinkigan was also less effective in this case. Therefore, SOKT was started for the onset of nocturnal pain. The VAS score improved to 3.0. In this case, the improvement in pain was not sufficient by interventional treatment with TPB, IVD, or combination therapy of goshajinkigan, but the VAS score showed a decrease in response to SOKT rather than goshajinkigan.SOKT is reported to be effective in cases of blood flow disorders in which prostaglandin E1 preparations are applicable. Thus, the increase in blood flow rate by SOKT improves neuropathy [11]. SOKT is orally administered and is non-invasive; therefore, the physical and mental burden of treatment is not heavy, and long-term administration is possible. SOKT has already been recognised for its effects on joint pain, neuralgia, low back pain, and muscle pain; however, few reports have been published regarding treatment with SOKT. As more evidence is accumulated, it is expected that the therapeutic effect for intractable diseases will be further demonstrated. Since Western medicine is mainstream in clinical practice, we examined the synergistic effect of SOKT in combination with interventional treatment. Combination therapy lowered the VAS score and improved pain. However, the analgesic effects of each composition have yet to be elucidated. There are few reports of neuropathy other than spinal canal stenosis. Therefore, further studies are required. In conclusion, our findings suggest that the administration of SOKT in combination with interventional treatment was effective for neurogenic low back and lower limb pain.
Acknowledgement
We would like to thank Dr. Heisuke Kino at Sakai Yamaguchi Hospital, Prof. Kaoru Inoue at Osaka Medical and Pharmaceutical University, and Mr. Etsuhiko Ueno at Ueno Pharmacy.
Patient Perspective
This case report was approved by the Ethics committee of Kyushu University Hospital, Fukuoka, Japan (No. 2020-556).
References
- Ministry of Health, Labour and Welfare (2019) Outline of the results of National Livelihood survey 2019.
- Hamaguchi T, Yoshino T, Horiba Y, Watanabe K (2017) Goshajinkigan for low back pain: An observational study. J Altern Complement Med 23(3): 208-213
- Kato S (2019) Geriatric medicine 57: 171-175, in Japanese.
- Yamada K, Takao Y, Yanamoto F, Kageyama M (2012) Journal of the Japanese Society for the Study of Chronic Pain 31: 129-132, in Japanese.
- Yoshimura N, Akune T, Fujiwara S, Shimizu Y, Yoshida H, et al. (2014) Prevalence of knee pain, lumbar pain and its coexistence in Japanese men and women: The Longitudinal Cohorts of Motor System Organ (LOCOMO) study. J Bone Miner Metab 32(5): 524-532.
- (2019) Japanese Orthopaedic Association (JOA) Clinical Practice Guidelines on the Management of Low Back pain, (2nd edn).
- Zhang J, Lv C, Wang HN, Cao Y (2013) Synergistic interaction between total glucosides and total flavonoids on chronic constriction injury induced neuropathic pain in rats. Pharm Biol 51(4): 455-462.
- Nakamura H, Kawashiri T, Kobayashi D, Uchida M, Egashira N, et al. (2021) Analgesic effects of Sokeikakketsuto on chemotherapy-induced mechanical allodynia and cold hyperalgesia in rats. Biol Pharm Bull 44(2): 271-274.
- Gauchan P, Andoh T, Kato A, Sasaki A, Kuraishi Y (2009) Effects of the prostaglandin E1 analog limaprost on mechanical allodynia caused by chemotherapeutic agents in mice. J Pharmacol Sci 109(3): 469-472.
- Arakawa K, Torigoe N, Kazumaki N, Suzuki T, Narita M (2011) Jpn J Pharm Palliat Care Sci 4: 1-13.
- Ishida K (2013) Kampo medicines as useful therapeutic agents in clinical practice of neurology: Case reports & representative medicines. Rinsho Shinkeigaku 53(11): 938-941.






























