Audiological Profiling in Paraneoplastic Neurological Syndrome: A Case Report
Fathima Shahla CK, Annapurna G Parameswaran and Teja Deepak Dessai*
Department of Hearing Studies, Dr. S. R. Chandrasekhar Institute of Speech and Hearing, India
Submission: May 04, 2022; Published: June 15, 2022
*Corresponding author: Teja Deepak Dessai, Assistant Professor, Dr. S. R. Chandrasekhar Institute of Speech and Hearing, Bengaluru, 560084, India
How to cite this article: Fathima Shahla CK, Annapurna G Parameswaran and Teja Deepak Dessai. Audiological Profiling in Paraneoplastic Neurological Syndrome: A Case Report. JOJ Case Stud. 2022; 13(4): 555868. DOI: 10.19080/JOJCS.2022.13.555868.
Abstract
The study reports a case with complaints of imbalance with postural changes and gait for 4 months. Mr. X was subjected to a detailed Audiological and Vestibular assessment. On evaluation, the objective and subjective test results revealed the presence of retro cochlear pathology. Thus, Mr. X was referred for a Neurological opinion and the results indicated the presence of Paraneoplastic Neurological Syndrome. Therefore, we can understand that individuals with Paraneoplastic Neurological Syndrome can present with abnormal audiological and vestibular test findings.
Keywords: Neurological condition; Autoimmune disorder; Audiology findings; Vestibular findings
Introduction
Paraneoplastic neurological syndromes (PNS) are rare disorders associated with cancer, not caused by direct invasion, metastasis or consequences of treatment. They are usually autoimmune in nature. PNS are rare, but are potentially treatable. PNS is associated with cancer, but is not caused by the direct tumour invasion, metastasis or consequences of treatment taken [1]. Primarily, PNS precedes or follows the cancer diagnosis, while, in some cases, the primary cancer may not be found in autopsy results [2]. They can affect any area of the nervous system, including the central, peripheral and autonomic nervous system. Auche [3], stated the involvement of peripheral nervous systems in cancer patients. Although the system involvement is often multifocal, like encephalomyelitis, it can involve a single system, e.g., cerebellar degeneration. PNS can present with multiple clinical manifestations like encephalitis, autonomic failure, peripheral neuropathy, cerebellar ataxia, visual complaints and many others [4]. The authors also stated that PNS are mainly autoimmune. When the body tries to eliminate tumour cells, it launches an immune response, and this response can target normal neural tissues [5]. This could be mediated by antibodies or by T-cells [6]. Thus, PNS reflects a nervous system-specific autoimmune attack initiated by onconeural antigens released to the peripheral lymphoid tissue from an unsuspected primary or recurrent neoplasm [2]. Frequently, a cerebrospinal fluid (CSF) study in these patients reveals lymphocytic pleocytosis, elevated protein, increased immune globulins (IgG) synthesis and oligoclonal bands, supporting the immunological pathology. The exact incidence and prevalence of these disorders are unknown. PNS are a rare clinical condition. It is estimated that 0.5-1% of all patients with cancer have clinically disabling PNS [1]. Early diagnosis and treatment are important because any delay can result in rapid progression and irreversible neurological damage. Diagnosing PNS is often difficult. It requires a combination of clinical and laboratory evaluations to reach early diagnosis.
Treatment of PNS includes treatment of the tumour, immunotherapy and supportive therapy. The best way to stabilize PNS is to treat the cancer as soon as possible. This includes surgical removal of tumour, chemotherapy and/or radiotherapy [4].
Cerebellar ataxia is one of the conditions observed in individuals with PNS and it refers to ataxia due to dysfunction of the cerebellum [7]. This causes a variety of elementary neurological deficits including asynergy, dysmetria and dysdiadochokinesia. Furthermore, ataxia may be caused by disturbances in cerebellum, brainstem, spinal cord, and peripheral nerves. People with acute cerebellar ataxia often have a loss of coordination and may have difficulty performing daily tasks.
Materials & Methods
Consent was taken from the patient and the data was anonymized to maintain patient confidentiality.
Case Report
The case presented in this study is a 62year old male who visited our institute for Audiological and Vestibular assessment. Mr. X, reported instability with postural changes and gait for 4 months. The onset was gradually progressive in nature. Mr. X worked as a machinery maintenance handling officer, and reported no exposure to noise (document handling office work in a relatively quiet room). The direct interview revealed recurrent attacks of low sodium level in blood and intake of medication for hypertension & diabetes mellitus for the past 10 years (details not revealed by Mr. X).
Results and Discussion

Audiological assessment was carried out using a test battery approach which comprised of various subjective and objective tests. Otoscopic examination showed bilateral cone of light on tympanic membrane with no obstruction or foreign bodies in the external auditory canal. Next Mr. X was subjected to Pure Tone Audiometry (PTA) testing in both air conduction & bone conduction mode from 250Hz to 8KHz and 250Hz to 4KHz respectively using GSI Audiostar Pro Clinical Audiometer. Mr. X was provisionally diagnosed as “Bilateral Hearing Sensitivity within Normal Limits with a Sensorineural Dip at 4KHz”. Further, additional tests such as Tympanometry and Reflexometry were performed using GSI Tympstar Pro. Figure 1 represents the test findings of PTA, Tympanometry and Reflexometry testing. Probe tones 226Hz & 678Hz were used for tympanometry. The test results revealed bilateral “A” type tympanogram with present ipsilateral and contralateral acoustic reflexes only in the right ear. Mr. X was also administered with DPOAEs using ILOV 6 software with L1 65dB and L2 55dB, F2/F1= 1.2 and test frequency range of 1000Hz to 8000Hz in both ears. Results revealed absent DPOAEs suggesting outer hair cells dysfunction in both the ears. To add on, Speech Audiometry results showed 15dB and 20dB scores for Speech Recognition Threshold in right and left ear respectively suggesting good PTA and SRT correlation. Likewise, Speech Reception Score showed 100% Score, Most Comfortable level was obtained at 45dBHL and Uncomfortable Loudness Level was obtained beyond 110dBHL for both the ears respectively. SPIN test was performed at 0dBSNR indicating fair auditory figure ground discrimination scores in right ear (40%) and poor scores in left ear (64%). Similarly, to rule out the presence of cochlear pathology, Short Increment Sensitivity Index test was performed and the scores were negative.
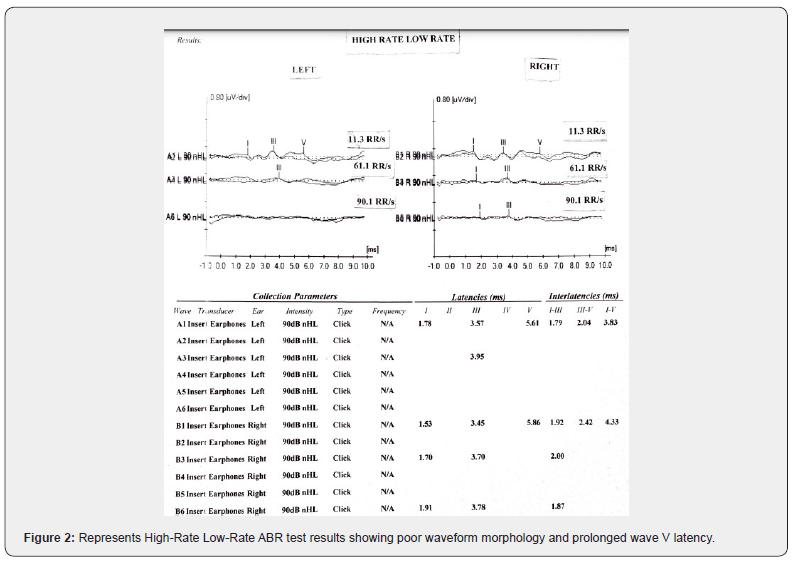
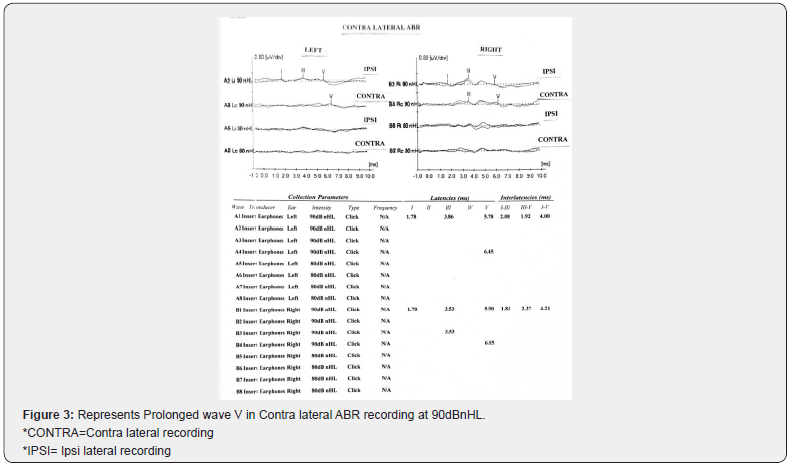
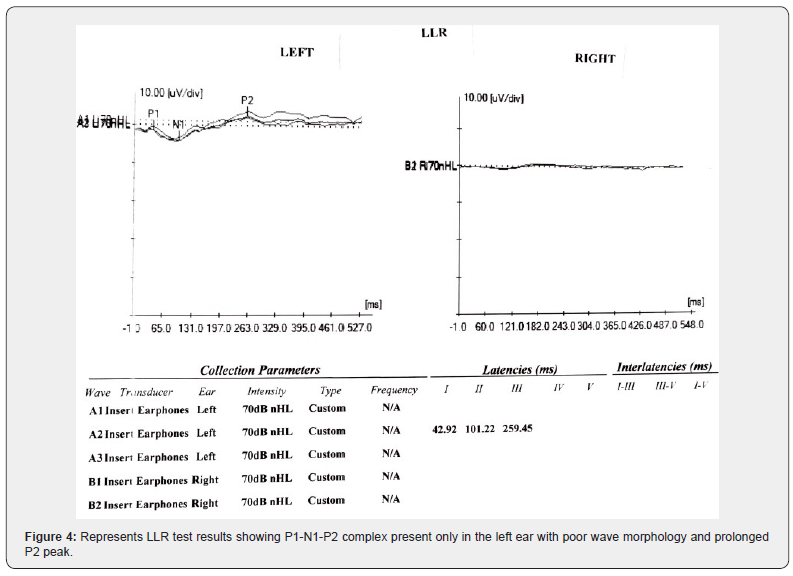
The above test results led to poor inter-test result correlation thereby, requiring further need to investigate using Electrophysiological tests. Diagnostic High-Rate Low-Rate Auditory Brainstem Response was performed using three repetition rates (RR) such as 11.3RR/s, 61.1RR/s and 90.1RR/s at higher intensity level of 90dBnHL which indicated bilateral retro-cochlear pathology with poor waveform morphology and prolongation of peak V in both the ears. Below Figure 2 represents the ABR findings. Likewise, test results of contralateral ABR confirmed the diagnosis of retrocochlear pathology with poor peak V waveform morphology and prolongation at 90dBnHL. The waveforms could not be elicited at lower intensity levels and are depicted in Figure 3. To add on in audiologic profiling, Mr. X was subjected to Late Latency Response (LLR) using speech stimuli /da/ at 0.5 repetition rate/s at an intensity of 70dBnHL. The P1-N1-P2 complex was present in the left ear with poor waveform morphology, however, the same was absent in the right ear. Figure 4 represents the LLR test results.
Additionally, considering the postural instability as the major complaint of Mr. X, he was subjected to subjective vestibular assessment, where only in the Romberg test sway was observed on both the sides. Other tests such as the Unterberg test, Fukuda Stepping Test, Dix Hallpike Test, Supine Head Roll Test, Disdiadochokinesis Test observed negative results. In the objective testing, Cervical Vestibular Evoked Myogenic Potentials (cVEMP) using tone burst stimuli of 500Hz and 1000Hz and Ocular Vestibular Evoked Myogenic Potentials (oVEMP) using tone burst stimuli of 500 Hz were administered at 95dBnHL. Absent P1-N1 and N1-P1 peaks were observed in both the testing respectively. Both cVEMP and oVEMP electro-physiological tests were performed using Biologic Navigator Pro version 7.2.
Early identification and treatment of paraneoplastic cerebellar degeneration is very important because a delay in the treatment can result in rapid progression and permanent neurological damage. Cerebrospinal Fluid (CSF) antibody testing is encouraged along with serum testing for the identification of the PNS. CSF study may reveal lymphocytic pleocytosis, elevated protein, increased IgG synthesis and oligoclonal bands, which indicate an immunological pathology.
The literature suggests the PNS treatment to comprise of the tumour treatment if identified, immunotherapy and supportive therapy. Treating cancer as soon as possible is the best way to stabilize PNS. This includes surgical removal of tumour, chemotherapy and/or radiotherapy. Immunotherapy includes steroids, intravenous immune globulins (IV IgG), plasma exchange, cyclophosphamide, azathioprine and rituximab. Supportive therapy includes symptomatic treatment like analgesics, antiepileptics, psychiatric medications, dysautonomia medications, physiotherapy, occupational therapy and speech and swallowing therapy. The treatment is patient specific and might need customisation as per the need [4].
All the test findings of Mr. X indicated presence of retro cochlear pathology and hence, Neurology referral was done to take a neurological assessment. Here, during the counselling session, Mr. X put forward his previous neurological investigation report and informed us of visiting our institute to seek a second opinion of his condition “Subacute onset of Cerebellar Ataxia along with Paraneoplastic Neurological Syndrome/ (?) infective cause”. Additionally, Mr. X had undergone Nerve Conduction study and the findings indicated “Mild Bilateral common peroneal nerve Axonal Neuropathy”. In his medical report whole body Fluorodeoxyglucose (FDG) - Positron Emission Tomography (PET), Computed Tomography (CT) SCAN showed an active “Mildly Prominent Mediastinal and Left Hilar Lymph Nodes’’ likely of infectious etiology. PET scans found to be useful in almost 39% of the cases when other imaging modalities fail to diagnose PNS [8]. Further, through non-contrast MRI whole spine screening, a mild diffuse disc bulge at C5-6, L2-3 and L5-S1 levels with mild marginal osteophytes at lumbar level were identified. The CSF antibody study reports confirmed the diagnosis of Mr. X having PNS and hence he was put up on medication for the same. CSF antibody test is one of the recommended tests to confirm the diagnosis of PNS [4].
We recommended Mr. X to monitor the neurological condition with a Neurologist, monitor hearing, undergo Physiotherapy and Vestibular Rehabilitation Therapy consisting of adaptive exercises, substitution exercises and habituation exercises 3 times a day for 3 months. Upon follow-up discussion with Mr. X after 3 months, he reported an overall reduction in the postural instability thereby leading to improved quality of life.
PNS often presents itself before the malignancy becomes clinically significant thereby making it a challenging task to diagnose PNS. The clinical investigations have reported no particular clinical pattern. Further, biopsies are invasive, difficult and nonspecific. Therefore, a combination of clinical and laboratory assessments needs to be carried out for correct and early diagnosis. Likewise, the treatment of underlying cancer is primarily important in the treatment of the neurological condition. Such can be achieved only with a high index of clinical suspicion. Case history pertaining to past or family history of cancer is essential. Presence of nonneurological symptoms such as anorexia, weight loss, fever, fatigue and dysgeusia are important clues towards PNS diagnosis. To add on, CSF evaluations often showcase nonspecific abnormalities such as mild to moderate degree lymphocytic pleocytosis, elevated protein and OCBs [4]. Therefore, one may establish the goal of PNS diagnosis with an alert mind and proceed forward with the suitable treatment at the earliest.
The above audiological and vestibular findings represented by Mr. X may also add to the existing clinical features of PNS. Presence of all the above-mentioned findings may directly or indirectly guide the clinician to hunt for the underlying condition with proper needed investigations. Therefore, an assessment of the hearing and balance system is of immense importance in the diagnosis of PNS.
Conclusion
This case highlights the need for collaborative functioning of various healthcare professionals in improving the quality of life of affected individuals. This also directs us to increase & seek referrals to other professionals in order to not miss any sequels of such neurological conditions. Identification of such rare conditions will further help in early identification and management of the condition.
References
- Dalmau J, Rosenfeild MR (2008) Paraneoplastic Neurologic syndromes. In: Fauci, Braunwald, Kasper, et al. (Eds.), Harrison's Principles of Internal Medicine.(17th edn), Vol 1, New York: McGraw Hill Medical, USA, pp. 623-627.
- Lachance DH, Lennon VA (2008) Paraneoplastic neurological autoimmunity. In Neuroimmunology in clinical practice. John Wiley and Sons 15: 210-217.
- Auche M (1890) Des nevrites peripheriques chez les cancereux. Rev Med 10: 785-807.
- Kannoth S (2012) Paraneoplastic neurologic syndrome: A practical approach. Annals of Indian Academy of Neurology 15(1): 6-12.
- Pittock SJ, Kryzer TJ, Lennon VA (2004) Paraneoplastic antibodies coexist and predict cancer, not neurological syndrome. Annals of Neurology 56(5): 715-719.
- Pittock SJ, Lennon VA (2016) Paraneoplastic Autoimmunity Affecting the Nervous System. In Brain Tumors. CRC Press 19: 543-568.
- Giometto B, Grisold W, Vitaliani R, Graus F, Honnorat J, et al. (2010) Paraneoplastic neurologic syndrome in the PNS Euronetwork database: a European study from 20 centers. Archives of Neurology 67(3): 330-335.
- McKeon A, Apiwattanakul M, Lachance DH, Lennon VA, Mandrekar JN, et al. (2010) Positron emission tomography–computed tomography in paraneoplastic neurologic disorders: systematic analysis and review. Archives of Neurology 67(3): 322-329.






























