Dyskeratosis Congenita: A Potentially Malignant Disorder
Jahanfar Jahanbani1, Ali Lotfi2, Sareh Farhadi1 and Firoozeh Samim3
1Department of Oral Pathology, Dental Branch Tehran Islamic Azad University, Iran
2Department of Oral Pathology, Dental School Shahidbeheshti University of Medical Sciences, Iran
3Department of Oral Medicine, Oral and Maxillofacial Pathologist, McGill University, Canada
Submission: January 04, 2021;Published: January 21, 2021
*Corresponding author: Firoozeh Samim, Clinical Assistant Professor, oral medicine, oral and maxillofacial pathologist, McGill Faculty of Dentistry, Canada
How to cite this article: Jahanfar J, Ali L, Sareh F, Firoozeh S. Dyskeratosis Congenita: A Potentially Malignant Disorder. JOJ Case Stud. 2020; 12(1):555827. DOI: 10.19080/JOJCS.2021.12.555827.
Abstract
Importance: Dyskeratosis congenita is a rare disorder with a variety of complications and associated disorders. Early diagnosis and intervention are important in care for patients because of its predisposition toward anemia, its multiple complications, and its higher risks of malignancy.
Observations: We describe a case of dyskeratosis congenita from a 32 year-old female with a diagnosis of ‘Fanconi anemia’ referred to our dental clinic later on for her oral lesions. Oral and extra oral examination revealed oral leukoplakia; skin pigmentations on hands, arms and chest; and dystrophic nails. Chromosome test of the patient’s shorter telomere length in peripheral blood lymphocytes favored the diagnosis of dyskeratosis congenita.
Conclusion: Early detection of oral and extra oral manifestations together with long-term care are important in patients with dyskeratosis congenita because of its susceptibility to malignancy, hematologic anomalies and infections. As consequence, its follow-up and treatment protocols vary widely. Additional case reports shed light on this entity paving the way for better care and treatment for dyskeratosis congenita patients. This case and other related reports indicate the hidden symptoms and diagnostic difficulties of dyskeratosis congenita, its difficult differentiation from Fanconi anemia, and oral health care professionals should pay attention to its non-specific clinical features to possibly enhance its early diagnostic rates.
Keywords:Dyskeratosis congenita; Leukoplakia; Dystrophic nail; Skin pigmentation; Fanconi anemia
Introduction
Dyskeratosis congenita (dyskeratosis congenita) is a rare inherited disorder which was first described by Zinsser in 1906 [1]. Later Engman and Cole with their colleagues reported other cases in detail and hence its name is also known as Cole-Engman syndrome or Zinsser-Cole-Engman syndrome [2]. Dyskeratosis congenita is characterized by cancer predisposition, marrow failure and other somatic anomalies. Its malignancies include acute myeloid leukemia (AML) and solid tumors particularly squamous cell carcinomas in the head and neck areas. Other clinical findings are dental anomalies, short stature, pulmonary fibrosis, immune deficiencies, premature graying or loss of hairs, esophageal stricture, osteoporosis, liver cirrhosis, urinary tract abnormities and hyperhidrosis. But most of these abnormities are absent at birth and developed with age and thus the dyskeratosis congenita diagnosis is oftentimes delayed to adolescence and adulthood [3]. Oral health care providers should be aware of the hidden and obscure diagnostic signs and symptoms because the oral lesions may undergo malignant transformation before any diagnoses.
Dyskeratosis congenita is diagnosed by a classic triad of skin pigmentation, nail dystrophy and oral leukoplakia, in which the mottled or reticulated skin hyperpigmentation involves the face, neck, shoulders and truck; the nail dystrophy involves both hands and feet, and the nail plates can be small and thin with longitudinal ridges that may disappear with age [3]. But the three typical diagnostic features are only seen in 46% of dyskeratosis congenita patients, and 75% of patients present with only one or more features. A small subset of patients presents with initial manifestations as marrow failure; malignancies such as leukemia, squamous cell cancer in the head and neck, and hepatic or cervical cancers; or other somatic findings like pulmonary fibrosis [4].
The prevalence rate of dyskeratosis congenita is less than one per million. In the past years, dyskeratosis congenita has gained more interest due to its pathogenesis. For example, its critical etiological factor is telomere which maintenance defects have been suggested as the etiology of dyskeratosis congenita. Telomeres are specialized nucleoprotein structures protecting the chromosome ends from degradation and inappropriate recombination. Telomeres have been one of the hot topics in chromosome research since Elizabeth Blackburn, Carol Greider and Jack Szostak were awarded Nobel Prize in Medicine in the year 2009 for their discovery of chromosome protection by telomeres and the related enzyme telomerase [5-8]. The research trend may also have impact on the heating up of dyskeratosis congenita attention in clinical research and treatment.
Patients with dyskeratosis congenita present with progressive bone marrow failure and classically clinical mucocutaneous triad of dystrophic nails, reticular skin pigmentation and oral leukoplakia. However, other somatic anomalies have also been reported including premature tooth loss, epiphora, enteropathy and diarrhea, pulmonary fibrosis, liver cirrhosis, early graying of the hair, osteoporosis and avascular necrosis of the bone, testicular atrophy, cerebellar ataxia caused by cerebellar atrophy, learning difficulties and mental retardation [9].
Case Presentation
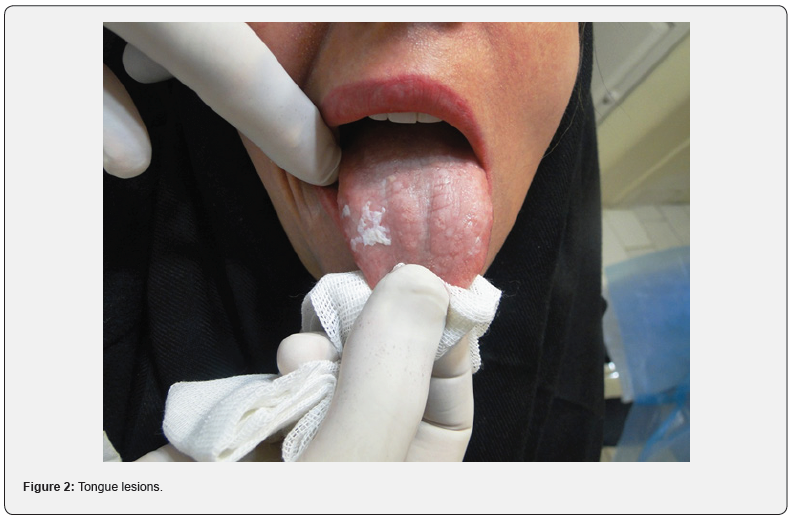
The case was a 37-year-old unmarried female patient referred to a private dental clinic two years earlier for her oral mucosal lesions. Patient appearance was pale; and during intra oral examination, a thin white plaque measured as 3 × 2cm on the anterior part of the mandibular buccal mucosa and attached gingiva together with another white plaque on the right dorsal part of the tongue were observed. These lesions had no indurated margins and were not scrapable with gauze (Figure 1 & 2). No other abnormal signs were observed in the teeth, periodontium, salivary glands and other oral structures.

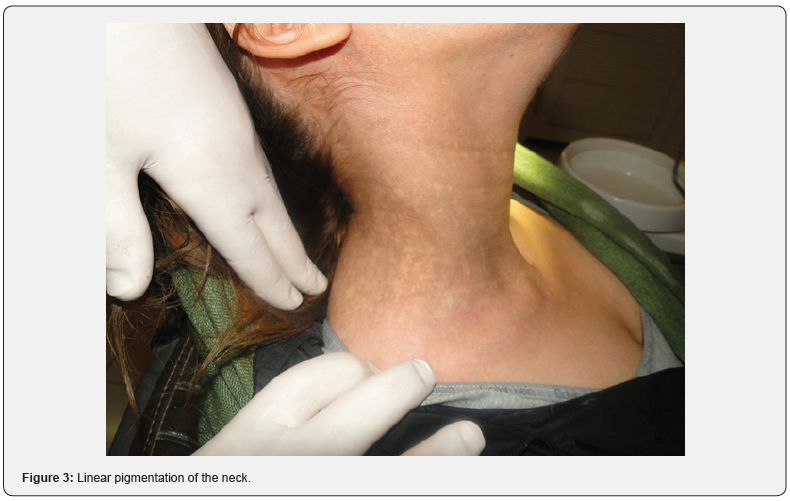
Examination of other parts of the body showed some linear brownish macular pigmentations on areas of the face, hands, neck and arms (Figure 3 & 4). The nails were brittle revealing mild changes of dystrophy. A positive chromosome breakage test in this patient was compatible with Fanconi anemia (Figure 5). The patient was undergoing treatment for her ‘anemia.’ But a later chromosome test of the patient’s telomere length in peripheral blood lymphocytes favored the diagnosis of dyskeratosis congenita.


The lesions on the buccal mucosa and the tongue were biopsied and the histopathology report confirmed the diagnosis of epithelial hyperplasia with mild to moderate dysplasia (Figure 6 & 7). One year later, in a follow-up visit another new white lesion on the left buccal mucosa was noticed. Histopathology report of the biopsy of the lesion confirmed mild to moderate dysplasia.


The patient has reported no history of similar lesions in her family. In addition, her dental, mucoskeletal, neurological, ophthalmic, genitourinary and psychological status were within normal limits. Based on the symptoms of skin pigmentation, nail dystrophy and oral leukoplakia, and the shorter telomere length in a chromosome test, the diagnosis of dyskeratosis congenita was made; and the patient has been followed up for oral malignancy, hematologic anomalies, and infections on a regular basis.
Discussion
Dyskeratosis congenita (dyskeratosis congenital) is a rare genetic disorder affecting 1:1,000,000 people in the world. Classically a clinical diagnosis is made by the presence of the mucocutaneous triad of oral leukoplakia, reticular and lacy skin pigmentation and dystrophic nails [10-12]. It is critical to note that the possibility of a more complicated entity is higher when more than one manifestations of mucocutaneous diseases in a patient is observed. Most importantly, most of the patients with classical dyskeratosis congenita will progress to bone marrow failure with predisposition to malignancy and a variety of dental, neurological, pulmonary, and gastrointestinal anomalies in relation to defective telomere maintenance [13,14].
In this report, the patient had the classical triad of oral leukoplakia, cutaneous pigmentations and mild dystrophic nails with anemia at the time of examination, in which the first chromosome breakage test was compatible with Fanconi anemia; but the followed genetic analysis of the patient’s telomere length favored the diagnosis of dyskeratosis congenita. In the literature, positive chromosome breakage may be shown in both Fanconi anemia and dyskeratosis congenita patients [15]; and aplastic anemia and cutaneous pigmentation may occur in both diseases [16]. But the two entities differ from each other; for example, Fanconi anemia may have a possible association with oral squamous cell carcinoma. In contrast to dyskeratosis congenita, Fanconi anemia is autosomal recessive with a minority being X-linked recessive patterns of inheritance and concomitant skeletal and renal anomalies. A most important differentiation test is chromosome test in which positive chromosome breakage is seen in Fanconi anemia; and much shorter telomere length is seen in dyskeratosis congenita [17]. Although telomere length in Fanconi anemia patients may be shorter than unaffected control individuals, they are mostly in normal range.
As mentioned above, nail dystrophy and oral leukoplakia have not been reported in Fanconi anemia as seen in the present case. These two symptoms have been suggested as critical signs for the differentiation of Fanconi anemia from dyskeratosis congenita [18]. In addition, hematopoietic deficiency has been reported in dyskeratosis congenita [19]. Furthermore, it has been emphasized that patients with dyskeratosis congenita have a predisposition for the development of a variety of malignancies such as myelodysplastic syndrome (MDS), secondary acute myeloid leukemia (AML), and head and neck squamous cell carcinomas [20,21].
It is worth noting that, in this case, two leukoplakic lesions were observed on the attached gingiva and lateral border of tongue, both of which are proved to have features of dysplasia above the basement membrane. Moreover, another new leukoplakia site was observed one year after the initial visit on the buccal mucosa, which were expected as reports show that patients with dyskeratosis congenita may develop independent tumors at more than one site [22].
Dyskeratosis congenita has variants [23]. Severe forma of dyskeratosis congenita called Hoyeraal-Hreidarsson syndrome is reported in early infancy together with other features like low birth weight, developmental delay, immunodeficiencies, cerebellar hypoplasia and bone marrow failure. Another reported dyskeratosis congenita variant is the Revesz syndrome with common dyskeratosis congenita features together with exudative retinopathy. But they are not the case of this report.
As an inherited disease, three patterns of inheritance are reported involving eleven genes as ACD, CTC1, DKC1, NHP2, NOP10, RTEL1, PARN, TERC, TERT, TINF2, and WRAP53. When these genes are mutated, they cause shorter telomeres through affecting telomere structure or telomerase [24-26]. As reported, telomerase is an enzyme in the maintenance of telomere to prevent end fusions, rearrangements, and secondary genomic instability. Telomere length is shorter in dyskeratosis congenita patients with bone marrow failure which may be related to disease severity and declines with age advancing [27]. Since the length of telomere is critical for normal cell proliferation, its defects may explain the anomalies observed in the skin and bone marrow as highly regenerative tissues and symptoms, which was observed in this case.
These multi gene mutations as the genetic causes of dyskeratosis congenita result in the complexity of dyskeratosis congenita clinical features and diagnostic difficulties. For example, dyskeratosis congenita can be seen in X-linked inheritance resulted from DKC1 gene mutations at Xq28 [28], autosomal dominant disease resulted from TERT or TINF2 gene mutations [29], and autosomal recessive disease resulted from TERT, NHP2, NOP10 mutations [30-32] to affect telomerase functions. As a consequence, oral health care professionals need to fully realize the complex genetic background of dyskeratosis congenita and its malignant potency in patients.
Current clinical findings in diagnosis help straight forward diagnosis of dyskeratosis congenita if all three diagnostic features present that define the disease well. However, in most cases these features may totally or partially absent which brings in diagnostic difficulties resulting in missing diagnosis. It is recommended that careful clinical history needs to be combined with thorough examination of the oral cavity and related body parts, as well as any other symptoms and signs related to bone marrow failure, cytopenias, cancer predisposition and other somatic anomalies. Importantly, personal and family history may offer useful information to clarify dyskeratosis congenita diagnosis [33]. As indicated by studies, nearly one quarter of dyskeratosis congenita patients as 10 out of 38 patients had personal or family history of pulmonary fibrosis or aplastic anemia, in which all of the 10 patients had TERT or TERC gene mutations. But absence in genetic mutation does not necessarily exclude the diagnosis of dyskeratosis congenita, and thus clinical and genetic tools should be used in patients with shorter telomere patterns to exclude dyskeratosis congenita [34]. In addition, as the most common cause of dyskeratosis congenita patient death, bone marrow failure occurs in three quarters of dyskeratosis congenita cases in which the median age is 10 years, and it typically starts with anemia or thrombocytopenia followed by pancytopenia as its symptoms and diagnostic features [11]. Clinical predominant dyskeratosis congenita symptoms and features with their percentages are listed in Table 1.
With regard to dyskeratosis congenita treatment, its current available treatment options are limited in which hematopoietic cell transplantation (HCT) is the only curative option for the severe cases of bone marrow failure, and pulmonary disease is a major cause of morbidity post HCT in dyskeratosis congenita patients [40]. Other conservative treatment such as anabolicandrogenic steroids may increase blood cell counts, but its adverse effects such as lipid abnormalities, splenic peliosis and growth acceleration require close monitoring upon its use [41]. In addition, reduced intensity conditioning (RIC) regimens can be used to treat dyskeratosis congenita patients sensitive to genotoxic agent such as those with Fanconi anemia [42], even though the clinical sequelae of RIC differ among patients.

Conclusion
In summary, dyskeratosis congenita constitutes a wide variety of manifestations and thus its follow-up and treatment protocols vary widely. However, early diagnosis and referral to specialty care is important in dyskeratosis congenita patients given their predisposition toward anemia, its multiple complications, and its higher risk of malignancies. Although the patient was previously treated for anemia because of a positive chromosome breakage test compatible with Fanconi anemia, the diagnosis of dyskeratosis congenita was not reached until after a later chromosome test showed the patient’s shorter telomere length. This case and other related reports indicate the hidden symptoms and diagnostic difficulties of dyskeratosis congenita, and oral health care professionals should pay attention to its non-specific clinical features to possibly enhance its early diagnostic rates.
References
- Tanaka A, Kumagai S, Nakagawa K, Yamamoto E (1999) Cole-Engman syndrome associated with leukoplakia of the tongue: a case report. J Oral Maxillofac Surg57(9):1138-1141.
- Boek KD, Degreef H, Verwilghen R, Corbel L, Daele MCV (1981)Thrombocytopenia:first symptom of dyskeratosis congenita. Pediatrics67(6):898-902.
- Shimamura A, Alter BP (2010) Pathophysiology and management of inherited bone marrow failure syndromes. Blood Rev24(3):101-122.
- Armanios MY, Chen JJ, Cogan JD, Alder JK, Ingeroll RG, et al. (2007) Telomerase mutations in families with idiopathic pulmonary fibrosis. N Engl J Med356(13):1317-1326
- AbdelKarim A, Frezzini C, Viggor S, Davidson LE, Thornhill MH, et al. (2009) Dyskeratosis congenita: a case report. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology and Endodontology108(2): e20-e24.
- Brown CJ (2000) Dyskeratosis congenita: report of a case. International Journal of Paediatric Dentistry10(4):328-334.
- Baran I, Nalcaci R, Kocak M (2010) Dyskeratosis congenita: clinical report and reviewof the literature. International Journal of Dental Hygiene8(1):68-74.
- Bessler M, Wilson DB, Mason PJ (2010) Dyskeratosis congenita. FEBS Lett 584(17): 3831-3838.
- Cole H, Rauschkolb J, Toomey J (1930) Dyskeratosis congenita with pigmentation, dystrophia unguis and leukokeratosis oris. Arch Derm Syph Suppl21:71-95.
- Dokal I (2011) Dyskeratosis congenita. Hematology Am Soc Hematol Educ Program2011:480-486.
- Mason PJ, Bessler M (2011) The genetics of dyskeratosis congenita. Cancer Genetics204(12):635-645.
- Nelson ND, Bertuch AA (2012) Dyskeratosis congenita as a disorder of telomere maintenance. Mutation Research730(1-2):43-51.
- Walne AJ, Dokal I (2009) Advances in the understanding of dyskeratosis congenita. British Journal of Haematology145(2):164-172.
- Dean A, Alamillos FJ, Velez A, Velasco F, Rodas J, et al. (1999) Squamous cell carcinoma of the oral cavity and Fanconi’s anemia. An association to bear in mind. Med Oral4(2):410-415.
- Coulthard S, Chase A, Pickard J, Goldman J, Dokal I (1998) Chromosomal breakage analysis in dyskeratosis congenita peripheral blood lymphocytes. Br J Haematol102(5):1162-1164.
- Vulliamy TJ, Dokal I (2008) Dyskeratosis congenita: the diverse clinical presentation of mutations in the telomerase complex. Biochimie 90(1):122-130.
- Alter BP, Giri N, Savage SA, Rosenberg PS (2015) Telomere length in inherited bone marrow failure syndromes. Haematologica100(1):49-54.
- Aukuck A(2007)Dyskeratosis congenita. Report of a case with literature review. Med Oral Patol Oral Cir Bucal12(5):E369-E373.
- Shahidi NT (1987)Fanconi anemia, dyskeratosis congenita, and WT Am J Med Genet Suppl3:263-278.
- Knight S, Vulliamy T, Copplestone A, Gluckman E, Mason P, et al. (1998) Dyskeratosis congenita (dyskeratosis congenita) registry: identification of new features of dyskeratosis congenita. Br J Haematol103(4):990-996.
- Alter BP, Giri N, Savage SA, Rosenberg PS (2009)Cancer in dyskeratosis congenita. Blood113(26):6549-6557.
- Baykal C, Kavak A, Gulcan P, Buyukbabani N (2003) Dyskeratosis congenita associated with three malignancies. J Eur Acad Dermatol Venereol17(2):216-218.
- Knight SW, Heiss NS, Vulliamy TJ, Aalfs CM, McMahon C, et al. (1999) Unexplained aplastic anaemia, immunodeficiency, and cerebellar hypoplasia (Hoyeraal-Hreidarsson syndrome) due to mutations in the dyskeratosis congenita gene, DKC1. Br J Haematol107(2):335-339.
- Ballew BJ, Yeager M, Jacobs K, Giri N, Boland J, et al. (2013) Germline mutations of regulator of telomere elongation helicase 1, RTEL1, in Dyskeratosis congenita. Hum Genet132(4):473-480.
- Guo Y, Kartawinata M, Li J, Pickett HA, Teo J, et al. (2014) Inherited bone marrow failure associated with germline mutation of ACD, the gene encoding telomere protein TPP1. Blood124(18):2767-2774.
- Tummala H, Walne A, Collopy L, Cardoso S, de la Fuente J, et al. (2015) Poly(A)-specific ribonuclease deficiency impacts telomere biology and causes dyskeratosis congenita. J Clin Invest125(5):2151-2160.
- Alter BP, Rosenberg PS, Giri N, Baerlocher GM, Lansdorp PM, et al. (2012) Telomere length is associated with disease severity and declines with age in dyskeratosis congenita. Haematologica97(3):353-359.
- Ruggero D, Grisendi S, Piazza F, Rego E, Mari F, et al. (2003) Dyskeratosis congenita and cancer in mice deficient in ribosomal RNA modification. Science299(5604):259-262.
- Walne AJ, Vulliamy T, Beswick R, Kirwan M, Dokal I (2008) TINF2 mutations result in very short telomeres: analysis of a large cohort of patients with dyskeratosis congenita and related bone marrow failure syndromes. Blood112(9):3594-600.
- Gramatges MM, Qi X, Sasa GS, Chen JJ, Bertuch AA (2013) A homozygous telomerase T-motif variant resulting in markedly reduced repeat addition processivity in siblings with HoyeraalHreidarsson syndrome. Blood121(18):3586-3593.
- Walne AJ, Vulliamy T, Marrone A, Beswick R, Kirwan M, et al. (2007) Genetic heterogeneity in autosomal recessive dyskeratosis congenita with one subtype due to mutations in the telomerase-associated protein NOP10. Hum Mol Genet16(13):1619-1629.
- Vulliamy T, Beswick R, Kirwan M, Marrone A, Digweed M, et al. (2008) Mutations in the telomerase component NHP2 cause the premature ageing syndrome dyskeratosis congenita. Proc Natl Acad Sci U S A105(23):8073-8088.
- Parry EM, Alder JK, Qi X, Chen JJ, Armanios M (2011) Syndrome complex of bone marrow failure and pulmonary fibrosis predicts germline defects in telomerase. Blood 117(21):5607-5611.
- Alter BP, Baerlocher GM, Savage SA, Chanock SJ, Weksler BB, et al. (2007) Very short telomere length by flow fluorescence in situ hybridization identifies patients with dyskeratosis congenita. Blood110(5):1439-1447.
- Tsilou ET, Giri N, Weinstein S, Mueller C, Savage SA, et al. (2010) Ocular and orbital manifestations of the inherited bone marrow failure syndromes: Fanconi anemia and dyskeratosis congenita. Ophthalmology117(3):615-622.
- Giri N, Lee R, Faro A, Huddleston CB, White FV, et al. (2011) Lung transplantation for pulmonary fibrosis in dyskeratosis congenita: Case Report and systematic literature review. BMC Blood Disord 11:3.
- Atkinson JC, Harvey KE, Domingo DL, Trujillo MI, Guadagnini JP, et al. (2008) Oral and dental phenotype of dyskeratosis congenita. Oral Dis14(5):419-427.
- Jyonouchi S, Forbes L, Ruchelli E, Sullivan KE (2011) Dyskeratosis congenita: a combined immunodeficiency with broad clinical spectrum--a single-center pediatric experience. Pediatr Allergy Immunol22(3):313-319.
- Jonassaint NL, Guo N, Califano JA, Montgomery EA, Armanios M (2013) The gastrointestinal manifestations of telomere-mediated disease. Aging Cell12(2):319-323.
- Dietz AC, Orchard PJ, Baker KS, Giller RH, Savage SA, et al. (2011) Disease-specific hematopoietic cell transplantation: nonmyeloablative conditioning regimen for dyskeratosis congenita. Bone Marrow Transplant46(1):98-104.
- Islam A, Rafiq S, Kirwan M, Walne A, Cavenagh J, et al. (2013)Haematological recovery in dyskeratosis congenita patients treated with danazol. Br J Haematol162(6):854-856.
- Ayas M, Nassar A, Hamidieh AA, KharfanDabaja M, Othman TB, et al. (2013) Reduced intensity conditioning is effective for hematopoietic SCT in dyskeratosis congenita-related BM failure. Bone Marrow Transplant48(9):1168-1172.






























