Late presentation of Two Rare Sacral Spine Tumors challenges of Diagnosis and Treatment in a Low Resource Setting
Alexis DB Buunaaim1,2,*, Anwar Sadat Seidu1,2, Emmanuel Akorli3, Yempabe Tolgou1 and Der EM4
1Orthopedic Unit, Tamale Teaching Hospital, Ghana
2Department of Surgery, University for Development Studies, Ghana
3Department of Radiology, Tamale Teaching Hospital, Ghana
4Department of Pathology, University for Development Studies, Ghana
Submission: September 18, 2020; Published: September 25, 2020
*Corresponding author: Dr. Alexis Dun Boib Buunaaim, Tamale Teaching Hospital, Tamale, Ghana
How to cite this article: Alexis DB B, Anwar S S, Emmanuel A, Yempabe T, Der E. Late presentation of Two Rare Sacral Spine Tumors challenges of Diagnosis and Treatment in a Low Resource Setting. JOJ Case Stud. 2020; 11(4): 555818. DOI: 10.19080/JOJCS.2020.11.555818.
Abstract
Lower back pain with or without an associated mass should be examined thoroughly by physical examination aided with radiological imaging. Described here are two young male adults; 29 and 30 years of age with lower back pain associated with lumbar masses. These patients initially treated themselves with herbal preparations without success. Diagnoses of chordoma and myxopapillary ependymoma were made in the 29 and 30-year old patients respectively after physical examination and imaging. These diagnoses were confirmed by histopathological investigation. Both patients requested discharge against medical advice. Unfortunately, they died at home within one month after discharge.
The diagnosis of chordoma and myxopapillary ependymoma can be very challenging and requires a multidisciplinary approach involving a radiologist, pathologist, oncologist and an orthopedic surgeon.
The poor outcomes in both patients could be attributed to ignorance, entrenched cultural beliefs, late diagnosis from low index of suspicion and lack of requisite diagnostic tools. This indicates that patients are still dying of treatable conditions in low- and middle-income countries especially in Africa. We propose awareness creation among clinicians, and a fund to be established both locally and globally to help with the diagnosis and treatment of sacral tumors.
Keywords:Sacral chordoma; Myxopapillary ependymoma; Late presentation; Spinal tumors
Abbreviations: CT: Computed Tomography; MRI: Magnetic Resonance Imaging; CNS: Central Nervous System; MPE: Myxopapillary Ependymoma; CBC: Complete Blood Count; LFT: Liver Function Test; RFT: Renal Function Test; ESR: Erythrocyte Sedimentation Rate
Introduction
Chordomas are rare slow growing malignant bone tumors that arise from embryonic notochordal remnants [1,2]. They account for 1-4% of all malignant bone neoplasms [3,4]. They occur in various anatomic locations with the sacral region being the most predominant site and lumbar spine being the least (sacrum 60%, spheno-occipital 25%, cervical 10% and thoracolumbar 5%) [5]. Symptoms generally depend on their location but patients typically present with pain at the initial stages [4,6-11]. Some patients may present with constipation, urine and or fecal incontinence due to autonomic nervous system involvement [6].
Chordomas pose diagnostic challenges to physicians [1,4]. However, diagnosis can be made through the use of CT and MRI, but histopathology is the mainstay of establishing diagnosis [1,2,4,6,12]. Surgical resection (marginal en bloc) with or without adjuvant radiotherapy is the treatment of choice [1,2,6,13,14]. Chordomas have poor prognosis because of local recurrence and metastasis [6,12], hence require yearly follow up even after 20-years of surgical resection [12].
Ependymomas are primary central nervous system (CNS) tumours that arise from the ependymal cells of the choroid plexus. They account for 2% of all primary CNS tumors [15]. They are divided into 5 subtypes: sub-ependymoma (grade I), myxopapillary ependymoma (grade I), ependymoma (grade II), RELA fusion-positive ependymoma (grade II or III), and anaplastic ependymoma (grade III) [16]. It is twice as common in men than women with an average age of presentation of 36yrs [16].
Myxopapillary ependymoma (MPE) commonly occur in the conus medullaris, cauda equina and filum terminale of the spinal cord [17]. MPE are grade I tumours and so they tend to grow slowly [18]. They have a high survival rate (98.4%) if early surgical intervention is performed [18].
We present two cases of rare spinal tumours; chordoma and myxopapillary ependymoma in Northern Ghana, who presented late to our institution for care when the initial herbal medical treatment failed. Clinical examination aided by imaging resulted in the suspicion of tumor. Histopathological examination of biopsy samples taken were confirmed as chordoma and myxopapillary ependymoma. We lost both patients a month after discharge against medical advice. This case report illustrates how late presentation and misdiagnosis results in poor outcomes of patients in low and middle resource settings.
Case One
Clinical history and physical examination
A 30-year old male presented with low back pain of 15 months duration. He also had a fungating lower back mass of 6-month duration. The patient initially managed the pain with over the counter analgesics until 10-months prior to presentation when he noticed a mass in his lower back. He went to a traditional healer where he was treated with herbal medications for 6-months because he thought it was a spiritual ailment. During this period, he began to experience a gradual loss of power in the lower limbs and this was associated with urine and faecal incontinence. He was bedridden and thus developed decubitus ulcers and the mass became ulcerated. He reported to a primary health facility because of the fungating mass and inability to move his lower limbs, where he was referred to our facility (tertiary).
On examination, he was a chronically ill looking man who had conjunctiva pallor, anicteric and mildly dehydrated. Systemic examination was essentially normal. He had a fungating lower back mass measuring 9×6cm, hard with irregular edges. The power in his lower limbs was 0/5 with lax anal sphincter tone.
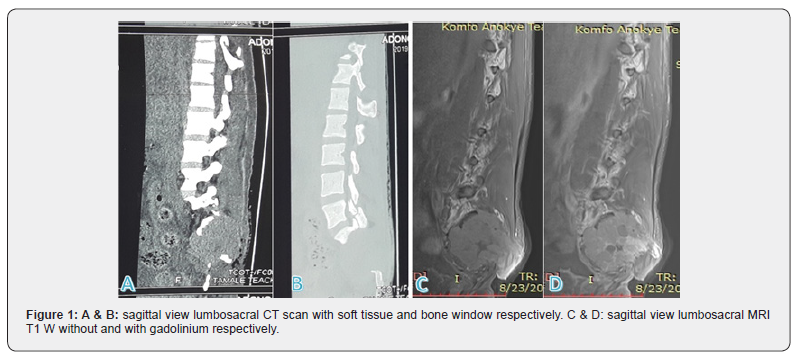
Imaging results
Lumbosacral CT scan showed a heterogenous sacral mass measuring 5.8×6.5×6.2cm with bony distraction of the sacrococcygeal spine (Figures 1A & 1B). Lumbosacral MRI showed a 6.8×7.0×6.8cm lobulated heterogenous T1W hypointense and T2W hyperintense right sided mass involving the vertebral bodies, laminae and pedicles of S1, S2 and S3. The mass extends across the sacroiliac joint and involves the right iliac bone. It encases the right S1-S3 nerve roots with attendant severe canal stenosis. There is also infiltration of the right erector spinatus muscle posteriorly (Figures 1C & 1D).
Hematology and biochemistry results
Complete blood count (CBC) showed a low hemoglobin. Renal function and liver function tests (RFT and LFT) were essentially normal and the erythrocyte sedimentation rate (ESR) was elevated.
Histopathology results
Histopathology from an incision biopsy showed a cellular lesion with bubbly myxochondroid stroma. The cells were illdefined with round oval nuclei. Some of the cells had vacuolated cytoplasm and prominent vesicular nuclei while others had small with inconspicuous nuclei and no visible nucleoli. The stroma was infiltrated with inflammatory cells. The histopathological findings confirmed the diagnosis of Chordoma in line with the clinical diagnosis. Immunohistochemical examination could not be performed by our laboratory.
While conducting a metastatic workup patient requested to be discharged against medical advice for care at home and died a month afterwards.
Case Two
Clinical history and physical examination
A 29-year old male who presented with a 12-month history of low back pain and a slowly growing mass in the lower back. The pain increased in intensity over the period and was associated with lower limb weakness and urine and fecal incontinence. He resorted to herbal medications as well as over the counter drugs for 7 months. He presented to a Primary health facility where he was misdiagnosed as Pott’s disease and treated with antituberculous drugs for 5 months before referral to our facility because of lower limb weakness.
On examination, he was a chronically ill looking man who was moderately dehydrated. Systemic examination was essentially normal. He had a mass in his lower back measuring 7×5cm, it was hard, nodular, tender with irregular edges. The power in his lower limbs was 4/5 and anal sphincter tone was good.
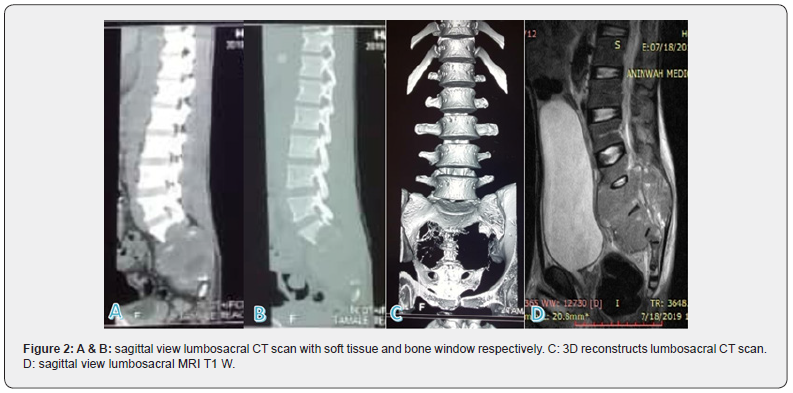
Imaging results
Lumbosacral CT scan showed a heterogenous soft tissue mass involving the sacrococcygeal spine with bony distraction. It invaded the distal spinal canal and the surrounding soft tissue. The lumbar vertebral bodies and their intervertebral disc were normal (Figure 2A, 2B & 2C). Lumbosacral MRI showed an ill-defined sacrococcygeal tumour measuring 11.6×8.9×15.6cm with bony distractions of the sacrum and coccyx, extending to L3 vertebra and invasion of the distal spinal canal. There was severe spinal canal stenosis from L3 to the sacral elements with destruction of the involved vertebral bodies (Figure 2D).
Hematology and biochemistry results
CBC, RFT and LFT were essentially normal with elevated ESR.
Histopathology results
Histology from a core biopsy showed fragments of fibrocollagenous tissue infiltrated by an epithelial lesion with papillary pattern of growth. There were also areas of myxoid changes. This confirmed the diagnosis of myxopapillary ependymoma was made and this agreed with the initial diagnosis made by the clinicians. Immunohistochemical examination could not be performed by our laboratory.
The patient requested discharge against medical advice on financial grounds. He succumbed to the disease after 3 months of discharge.
Discussion
Chordomas are rare slow growing malignant bone tumors accounting for 1-4% of all malignant bone neoplasms [1,6]. Because of their slow growing nature, they are clinically dormant until later in the course of the disease [4]. The symptoms generally depend on their location with commonest being pain and neurologic symptoms [4,6-11]. For these reasons, most patients present to health facilities when the course of the disease is advanced. However, in low resource settings where the hospital is usually not the first point of call for a lot of patients (but the Traditional healer), patients present much later to the hospital when all hope is lost. This leaves the surgeon with very few options to work with. This was demonstrated as it took 15 months from the onset of symptoms, to presenting to a health facility. The patient in this current case report presented with very advanced form of the disease. In poor resource settings, most patients will resort to the Traditional healer whose services are relatively affordable compared to Orthodox health facilities, as illustrated in this case.
Mcmaster et al. [19] in 2001 reported the incidence rate of chordoma as 0.08 per 100,000 in the United States [19]. They also reported that chordomas are uncommon in blacks and people under 40yrs [19]. They observed a male predominance with an incidence rate of 0.10 as compared to females with 0.06 [19]. Murphey et al reported the male to female ratio of 2-3:1 [4]. The current case report from Northern Ghana involved a black male of 39-years of age. Being a male increased his chances of developing a chordoma, but his race and age reduced his risk. This accounts for the rarity of such cases in our settings and sometimes contribute to the low index of suspicion by most physicians. The young age group and the female sex are more likely to develop cranial chordoma [19] which contrast with the sacral presentation of case 1.
Diagnosing chordoma can be very challenging [1,4] but radiological imaging (CT and MRI) play a crucial role in preoperative diagnosis of chordoma [1,2,4,6,12]. Murphy et al illustrated that, most primary tumors of the spine present with characteristic radiologic features on CT and MRI [4]. With the aid of diagnostic images and the appropriate technical human resource, diagnosis can be made easily.
It is worth noting that plain radiographs cannot be used in diagnosing myxopapillary ependymoma (MPE). In low resource settings, primary and secondary health facilities only have access to X rays, hence the reason for misdiagnosis of case 2. The patient was misdiagnosed as Pott’s disease and received tuberculosis treatment regimen for 5 months which delayed time to definitive diagnosis. He was referred from the primary health facility to a tertiary facility for specialist care. A lumbosacral CT and MRI was done and a core biopsy taken for histopathology to confirm the diagnosis.
Both chordoma and MPE have good prognosis when they present early because they can be completely resected [4,18]. Prognosis is largely poor if both chordoma and MPE are left untreated [4,6,18].
In our opinion, poverty and ignorance is the main reason for late presentation of most patients in low resource settings of rural Ghana. Patients are more likely to resort to Traditional healers as their first point of call because their services are cheaper and are more accessible compared to orthodox health services. Also, the bureaucracies in the orthodox health services can be frustrating to patients. Our primary and secondary health services are under resourced both in diagnostic capability and human resource, which accounted for the misdiagnosis.
The lesson from these cases is for clinicians to develop a high index of suspicion and early referral of patients to appropriate centers for treatment especially when there is a suspicion of a cancer. Policy makers in low resource settings should work towards developing the referral and diagnostic capabilities of their primary and secondary health services. They also need to reduce the cost of diagnostic investigations especially for cancer through an established fund to enable patients present early to health facilities for prompt diagnosis and treatment.
Acknowledgement
Special thanks to our radiologist; Dr Patricia Akorli for the choice of images and comments.
Conflict of Interest
Authors declared no conflict of interest with respect to authorship and publication of this case report.
Author’s Contributions
ADBB conceived the idea. ASS and ADBB drafted the manuscript. EM made the radiological inputs and EMD read the histopathology. ADBB, ASS, TY critically reviewed the manuscript for academic content. All authors read and agreed on the final manuscript.
References
- Zhou Y, Hu B, Wu Z, Cheng H, Dai M, Zhang B (2018) A giant lumbar chordoma: A case report. Medicine (Baltimore). 97(25):e11128.
- Sharma H, Virdi G, McGraw I, MacDuff E, Periasamy K (2017) An Atypical Presentation of Chordoma: Case Report and Review. Orthop Muscular Syst 06(04).
- Mcpherson C, Suki D, Mccutcheon I, Gokaslan Z, Rhines L, et al. (2006) Metastatic disease from spinal chordoma: A 10-year experience. J Neurosurg Spine5(4):277-280.
- Murphey M, Andrews C, Flemming D, Temple H, Smith W, et al. (1996) From the Archives of the AFIP: Primary Tumors of the Spine: Radiologic-Pathologic Correlation. Radiogr Rev PublRadiol Soc N Am Inc16(5):1131-1158.
- Mirra JM. WHO Classification of tumours. Pathology and genetics of tumours of soft tissue and bone.
- Manasan C, Jose Carnate J (2018) Dedifferentiated Chordoma in a 53-year-old Female: A Case Report. Philipp J Pathol 3(1):12.
- Boriani S, Chevalley F, Weinstein JN, Biagini R, Campanacci L, et al. (1996)Chordoma of the spine above the sacrum. Treatment and outcome in 21 cases. Spine 21(13):1569-1577.
- Yang X, A Richard S, Zhao W, Liu J, Huang S (2019) A Giant Sacrococcygeal Chordoma: Case Report and Literature Review. Adv Biosci Clin Med7:60-63.
- Godkin O, Elkhwad H, McCabe J (2017) Large chordoma of the sacrum. Case Rep 2017.
- Rao BSS, Menezes LT, Rao AD, John SK. Sacral chordoma - a report of two cases.Case Report 67(4): 207-209.
- Endo K, Yamashita H, Nagashima H, Teshima R (2014) Sacral chordoma in an adult showing an aggressive clinical course: A case report. Oncol Lett7(5):1443-1446.
- Dubory A, Missenard G, Court C (2016) Late local recurrence, at 19 and 17years, of sacral chordoma treated by en bloc resection. OrthopTraumatol Surg Res102(1):121-125.
- Phang ZH, Saw XY, Nor NFBM, Ahmad ZB, Ibrahim SB (2018) Rare case of neglected large sacral Chordoma in a young female treated by wide En bloc resection and Sacrectomy. BMC Cancer18(1):1112.
- Hsieh PC, Xu R, Sciubba DM, McGirt MJ, Nelson C, et al. (2009) Long-Term Clinical Outcomes Following En Bloc Resections for Sacral Chordomas and Chondrosarcomas: A Series of Twenty Consecutive Patients. Spine34(20):2233-2239.
- Clover LL, Hazuka MB, Kinzie JJ (1993) Spinal cord ependymomas treated with surgery and radiation therapy. A review of 11 cases. Am J Clin Oncol16(4):350-353.
- Louis DN, Perry A, Reifenberger G, von Deimling A, Branger DF, et al. (2016) The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. Acta Neuropathol (Berl) 131(6):803-820.
- Cervoni L, Celli P, Caruso R, Gagliardi FM, Cantore GP (1997) Neurinomas and ependymomas of the cauda equina. A review of the clinical characteristics. Minerva Chir52(5):629-633.
- Pusat S, ErbaşYC, Göçmen S, Kocaoğlu M, Erdoğan E (2019) Natural Course of Myxopapillary Ependymoma: Unusual Case Report and Review of Literature. World Neurosurg121:239-242.
- McMaster ML, Goldstein AM, Bromley CM, Ishibe N, Parry DM (2001) Chordoma: incidence and survival patterns in the United States, 1973-1995. Cancer Causes Control12(1):1-11.






























