Effect Size Statistics to Inform an Exploratory Analysis of a Double-Blinded, Randomised, Placebo Controlled Pilot Clinical Study to Evaluate the Efficacy of Naticol®, Specific Fish Collagen Peptides to Alleviate Symptoms of Osteoarthritis in the Knee
Seán Lacey1*, Christelle Bonnet2, Kelly Seamans3 and Andrea Doolan3
1Department of Mathematics, Cork Institute of Technology, Ireland
2Weishardt International, France
3Atlantia Food Clinical Trials, Cork, Ireland
Submission: June 06, 2019; Published: June 17, 2019
*Corresponding author: Seán Lacey, Department of Mathematics, Cork Institute of Technology, Bishops town, Cork, T12 P928, Ireland
How to cite this article: Seán Lacey, Christelle Bonnet, Kelly Seamans, Andrea Doolan. Effect Size Statistics to Inform an Exploratory Analysis of a Double-Blinded, Randomised, Placebo Controlled Pilot Clinical Study to Evaluate the Efficacy of Naticol®, Specific Fish Collagen Peptides to Alleviate Symptoms of Osteoarthritis in the Knee. JOJ Case Stud. 2019; 10(2): 555783. DOI: 10.19080/JOJCS.2019.10.555783.
Abstract
Background: Potential effects of different doses of specific fish collagen peptides (Naticol®) on the signs of skin ageing were firstly assessed in double-blind, randomised and placebo controlled clinical studies. The studies showed benefits of fish collagen peptides (Naticol®) on skin firmness, skin hydration and wrinkle appearance. In addition to these benefits, some animal experiments have suggested that ingestion of specific fish collagen peptides (Naticol®) might also have beneficial effects on joint health such as osteoarthritis.
Aim: This pilot clinical trial study was designed to assess the safety and tolerability of daily oral doses of specific fish collagen peptides (Naticol®) in healthy subjects with knee osteoarthritis.
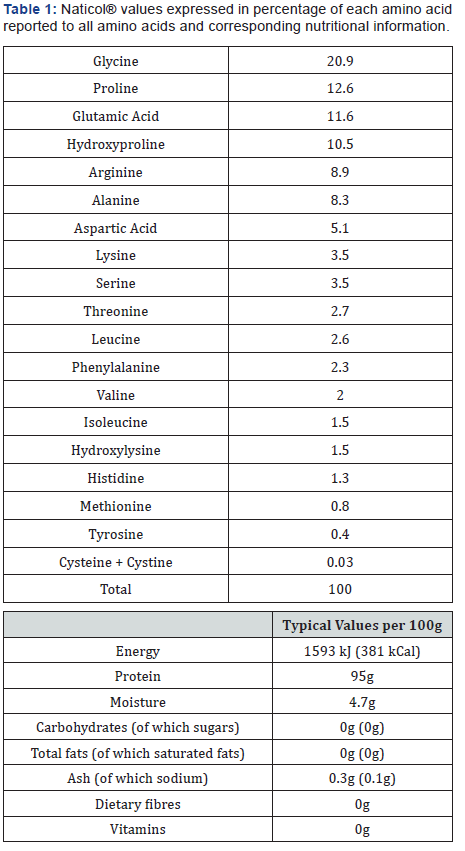
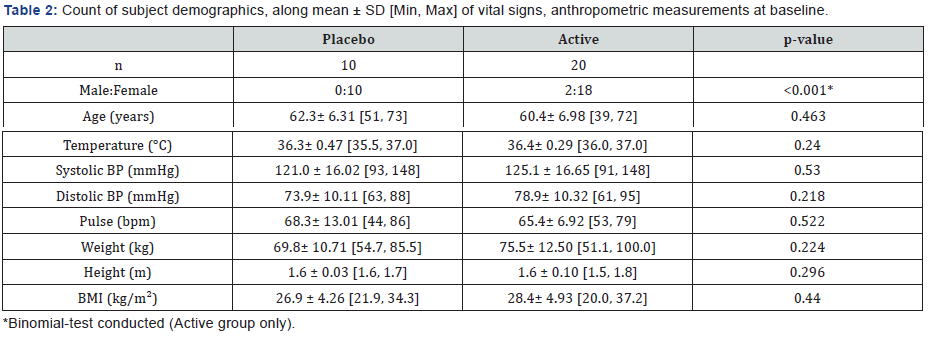
Methods: In a double-blinded, placebo controlled pilot clinical study, 30 adults (20 active; 10 placebo) consumed a 10g sachet of the investigational product (Naticol®; specific fish collagen peptides) and a comparator product (maltodextrin) daily in 20cl of cold liquid (fruit juice, milk or cold tea) 15 minutes before breakfast, for 8 weeks. Potential pain reduction was tested using the Western Ontario McMaster Universities (WOMAC) scores; Quality of Life (QOL) using the Participant Global Assessment (SF-36v2 questionnaire) and Physical performance using the Short Physical Performance Battery (SPPB) at both baseline and after 8 weeks.
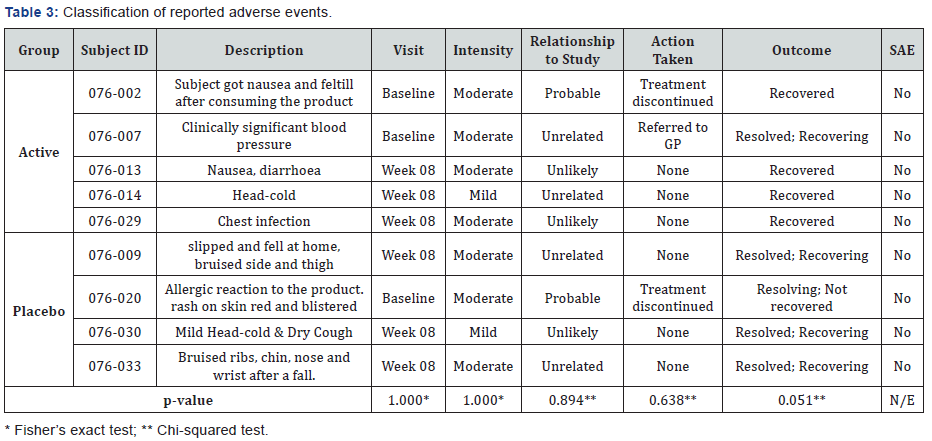
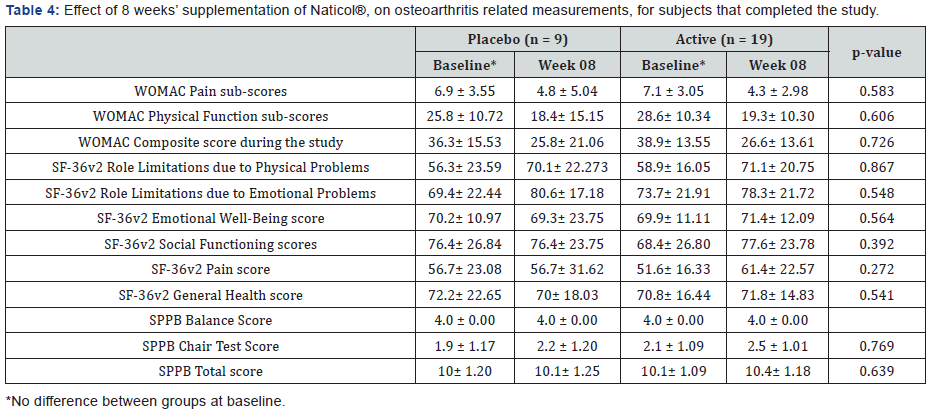
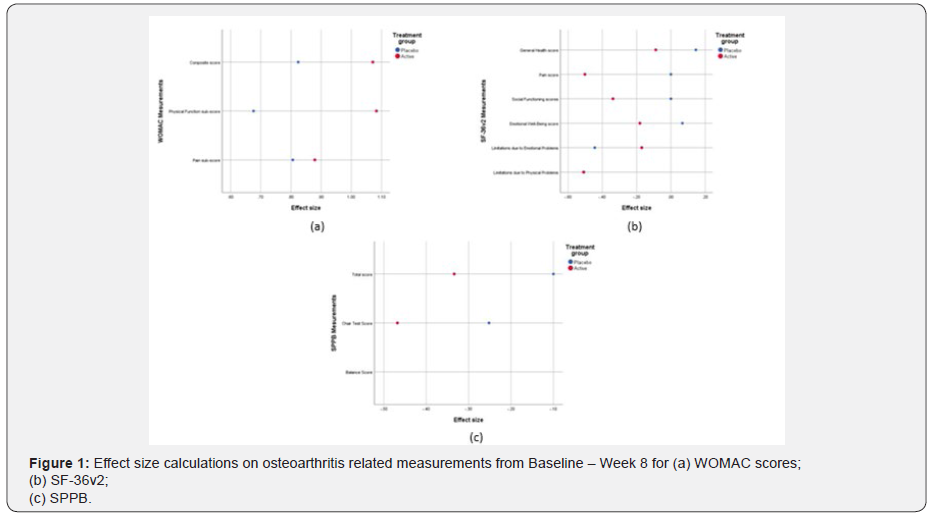
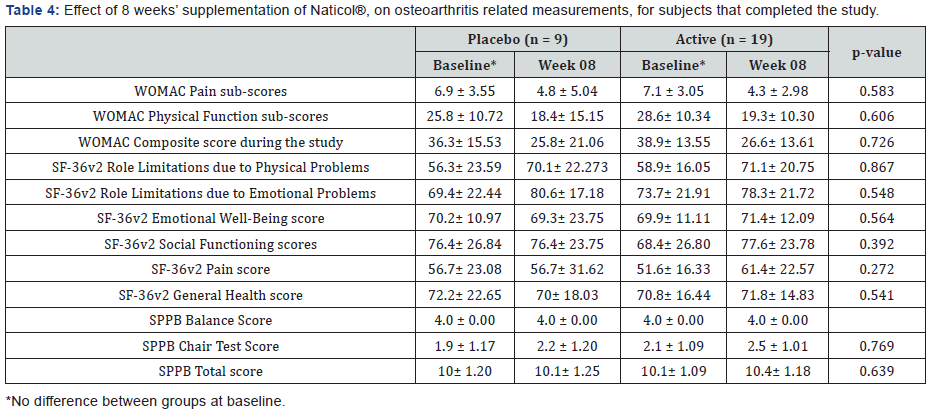
Results: From effect size statistics (Cohen’s d), subjects in the active group experienced more of an improvement across the majority of measurements than subjects in the placebo group over the 8 weeks of the study. From the WOMAC Physical Function sub-score the placebo group experienced a small improvement (d = 0.68) against the active group’s large improvement (d = 1.08). While for the WOMAC Composite score the active group experienced a large improvement (d = 1.07). In terms of the SF-36v2 Social Functioning and Pain sub scores, there was no change in score for the placebo group (d = 0.00), while the active group noticed an improvement by small (d = -0.34) and medium (d = -0.50) amounts, respectively. While for the SF-36v2 Emotional Well-Being and General Healthy Issues sub scores, the placebo-based subjects dis-improved over the 8 weeks (d = 0.07 and 0.15, respectively), while the subjects in the active group improved in both cases (d = -0.18) and -0.09, respectively). In terms of the SPPB, active group experienced an improvement in the Chair test and Total score. (d = 0.47 and d = -0.33, respectively). There was no difference in adverse events between groups (p > 0.05).
Conclusion: The results demonstrated that daily oral doses of specific fish collagen peptides (Naticol®) in healthy subjects with knee osteoarthritis has the potential to reduce pain, improve quality of life and lower body function. Further studies with a higher dosage of product for subjects with a body weight greater than 70kg should be performed.
Keywords: Clinical study; Effect size; Fish collagen peptides; Naticol®; Osteoarthritis
Abbreviations: AE: Adverse Event; ANOVA: Analysis of Variance; BMI: Body Mass Index; CH: Collagen Hydrolysates; GP: General Practitioner; OA: Osteoarthritis; QOL: Quality of Life; SAE: Serious Adverse Event; SD: Standard Deviation; SF-36v2: Short Form – 36 Version 2; SPPB: Short Physical Performance Battery; WOMAC: Western Ontario and McMaster Universities Osteoarthritis Index
Introduction
Osteoarthritis (OA) results from an imbalance of anabolism and catabolism in the joint, which may be influenced by the biological and mechanical environment. Excessive forces in specific regions of the joint surfaces and alterations in tissue responses, leading to the development of osteoarthritis are also exacerbated with abnormal loading of the knee joint due to overweight or a joint disorder [1-3].
Today, the total cost of osteoarthritis has been estimated to be between 1% and 2.5% of the total gross domestic product in western countries [4]. In Europe, over 100 million people have arthritis, and in the United States, the direct costs of arthritis were $51.1 billion in 2004 [5]. As the number of elderly people increases, osteoarthritis represents a major economic burden on the health care systems and is a serious threat to the quality of life within the populations. For instance, in the UK in 2010, there were 4.7 million doctor appointments due to knee osteoarthritis for patients over 45 years. It has been predicted that this number will increase to 6.7 million by 2051 [6].
This pilot study was designed to assess the tolerability and efficacy of oral doses of fish collagen peptides (Naticol®, 10g/day) in volunteers with knee osteoarthritis. The collagen hydrolysates or peptides (Naticol®) which were the object of this efficacy study were products derived from fish hydrolysed collagen (gelatin) suitable for use in human food. Previous clinical studies aimed at assessing the effects of oral intakes of fish collagen peptides, Naticol®, on skin firmness and hydration, and the decrease of wrinkles were conducted using different dosages (10g/day; 5g/day; 2,5g/day) [7,8]. The results from Duteil et al. [7] and Sibilla et al. [8] confirmed preclinical and clinical human trials investigating the effects of oral supplementation with collagen peptides that have indicated the possibility that dietary compounds can modulate skin function. For example, Matsuda et al. [9] reported that in pigs a 9-week oral ingestion of collagen hydrolysates (CH) induced increased fibroblast density and enhanced formation of collagen fibrils in the dermis in a proteinspecific manner. Literature also indicates benefits of collagen hydrolysates in joints as they are absorbed, distributed to joint tissues and have analgesic and anti-inflammatory properties [10-14].
The aim of the study was to determine the effect of 8 weeks’ supplementation of Naticol®, Fish collagen peptides on change in WOMAC scores; Quality of Life, using the Participant Global Assessment (SF-36v2 questionnaire) and Physical performance using the Short Physical Performance Battery (SPPB), along with supporting the safety of the product by recording any reported adverse events.
Participants and Methods
Subjects underwent an initial phone screen and were asked questions regarding their age, general health and osteoarthritis diagnosis. Forty eligible subjects were scheduled for an initial visit. The pilot study involved 2 visits over an 8-week period. At the initial visit, subjects were included if they were: Aged 30 to 75 years (inclusive); Had documented diagnosis of primary osteoarthritis (OA) of the target knee made at least 12 months prior to the visit; Had radiographic evidence of OA in the tibiofemoral compartment of the target knee with at least 1 definite osteophyte and a measurable joint space, as diagnosed by standard X-rays; Had a Kellgree-Lawrence grade 2-4. Potential female subjects were excluded if they were pregnant, lactating or wished to become pregnant during the study. Subjects were also excluded if they: Had viscosupplementation in any joint including the target knee or other joint within 6 months prior to the initial visit; Had concomitant inflammatory disease or other condition that affects the joints; Had taken any calcium supplements within the previous 4-weeks; Had a disease/illness that would preclude supplement ingestion and/or assessment of safety and the study objectives and/or had a known allergy to components of the test product; Had lost > 5% of their total body weight in the last 3 months.
The site, investigator, protocol, informed consent form and other pertinent documents for this study were approved by the Cork Research Ethics Committee of the Cork Teaching Hospitals, Lancaster Hall, 6 Little Hanover Street, Cork. All subjects gave their written consent according to the Helsinki Declaration.
Case Study
A 41-year-old Para 3, otherwise healthy woman, presented with C3H2R2 prolapse according to POP-Q testing, in aggravation since her second pregnancy. She had no urinary incontinence complaints. A conservative treatment with pessary was tried but was not found to be satisfactory. Five months before she was referred to us, she reported pain in the right iliac fossa and underwent a CT scan, that described an 80x40x30mm right pelvic homogenous fluid collection of unknown origin (Figure 1). A diagnostic laparoscopy was performed, and the only finding was a slight retroperitoneal bulging near the right uterosacral ligament, no surgical treatment was attempted, and the surgeon concluded to a venous vs lymphatic stasis. One month later, MRI imaging was performed for persisting pelvic pain and was unremarkable apart from the pelvic organ prolapse: no fluid-like collection was described (Figure 2). She was referred to our center for surgical management of the prolapse. Clinical exam confirmed C3H2R2 prolapse according POP-Q testing. She underwent laparoscopic sacrocolpopexy with concomitant subtotal hysterectomy and salpingectomy. During the surgery the slight peritoneal bulging was seen again, but not removed, because we were afraid of venous stasis. The 6-weeks postoperative clinical exam showed persistent cystocele with no recurrent hysterocele. Bulging appeared 2 weeks postoperatively and pain reappeared. A repeat MRI highlighted the presence of a large cyst of vaginal origin (Figure 3). The cyst was punctured, with aspiration of clear brownish fluid allowing a decrease of pain. We scheduled a surgical total cyst excision per vaginam (Figure 4). At her postoperative visit, the patient reported some dyspareunia. Examination presented well healed incisions and a good anterior, apical and posterior support. Histology of the lesion revealed a Müllerian cyst lined by endocervical cells, secreting mucinous fluid inside this cyst. A detailed review of the radiologic exams concluded that it was a cyst of vaginal origin with wandering fluid passing from the vagina to the right posterior fornix through an hourglass like passage located next to the cervix, at the origin of the prolapse (Figure 2).
Discussion
Vaginal wall cysts are usually seen in the third and fourth decades [4,8], their presence is noted incidentally during physical exams or radiologic imagery. It can be symptomatic when of large size: in our case the patient’s complaint was vaginal pressure and discomfort, right iliac fossa pain, and dyspareunia, which are like POP symptoms [12]. Because MRI did not describe any fluid collection, we assumed it was simply a POP. In our knowledge, there are a dozen reported cases of vaginal cyst mimicking cystocele and one accompanied with cervical elongation [1-7], but this is the first reported case of vaginal cysts associated with hysterocele.
Mullerian and Gartner cysts are benign tumors, but malignancy must be considered. Lee reported adenocarcinoma arising in a Mullerian vaginal cyst [13]. In literature there are very rare reported cases of malignant vaginal cysts, but even with an asymptomatic and small cyst this eventuality should be considered.
Cysts should be characterized by radiologic investigations, Ultrasound and computed tomography (CT) are helpful to define the cystic mass [7,11,12]. Magnetic Resonance Imaging (MRI) is the gold standard to characterize surrounding tissues and define origin and extent of the pelvic mass. In our case, the first exam was a CT. The radiologist described a pelvic homogenous fluid collection of unknown origin. Use of MRI might have allowed better characterization of the müllerian vaginal cyst.
Management of vaginal cysts depends on the associated symptoms. In the cases of incidental finding of asymptomatic vaginal cysts, conservative treatment with observation may be an option [14] Vaginal cyst discharge by fluid aspiration reduces volume and pain as in one case describing a vaginal cyst discovered during pregnancy. This fluid aspiration permitted vaginal birth [2]. In 1991 Raddo [15] described a non- surgical management with use of 5% tetracycline sclerotherapy after cyst aspiration with good results.
Conventionally the management is surgical including marsupialization in rare cases and more often complete surgical excision [14]. In our case after sacrocolpopexy, we discharged the cyst and a few days later we performed an excision with good anatomic results.
Conclusion
This case report highlights the need to correlate radiologic to physical exams by one referent. In our knowledge, no case report has ever described hysterocele associated with Müllerian vaginal cyst. However, it is not possible to definitively conclude if the cyst was mimicking a vaginal prolapse or whether it was a true prolapse associated with wandering content of a large Mullerian cyst.
References
- Lallar M, Nandal R, Sharma D, Shastri S (2015) Large posterior vaginal cyst in pregnancy. BMJ Case Report 2015.
- Arumugam AV, Kumar G, Si LK, Vijayananthan A (2007) Gartner duct cyst in pregnancy presenting as a prolapsing pelvic mass. Biomed Imaging Interv J 3(4): e46.
- Davidson ERW, Barber MD (2017) A Gartner Duct Cyst Masquerading as Anterior Vaginal Prolapse. Obstetrics and Gynecology 130(5): 1039-1041.
- Dilbaz B, Sengül O, Dede S, Yerebasmaz N, Akkurt O (2014) Prolapsing vaginal Mullerian cyst with cervical elongation mimicking cystocele. J Obstet Gynaecol 34(2): 212-213.
- Toz E, Sanci M, Cumurcu S, Ozcan A (2015) Müllerian Cyst of the Vagina Masquerading a Cystocele Case Reports in Obstetrics and Gynecology 2015(376834): 3.
- Inoncêncio G, Azevedo S, Braga A, Carinhas MJ (2013) Large Gartner cyst. BMJ Case report.
- Hwang JH, Oh MJ, Lee NW, Hur JY, Lee KW, et al. (2009) Multiple vaginal mullerian cysts: a case report and review of literature. Arch Gynecol Onstet 280(1): 137-139.
- Eilber KS, Raz S (2003) Begnign cystic lesions of the vagina: a literature review. J Urol 170(3): 717-722.
- Prdhan S, Tobon H (1986) Vaginal cysts: a clinicalpathological study of 41 cases. Int J Gynecol Pathol 5(1): 35-46.
- Dwyer PL, Rosamalia A (2005) Congenital urogenital anomalies that are associated with the persistence of Gartner’s duct: a review. Am J Obstet Gynecol 195(2): 354-359.
- Tiwari U, Relia N, Shailesh F, Kaushik C (2014) Gartner Duct Cyst: CT and MRI findings. J Obstet Gynaecol India 64(Suppl 1): 150-151.
- Elsayes KM, Narra VR, Dillman JR, Velcheti V, Hameed O, et al. (2007) Vaginal masses: magnetic Resonance Imaging features with Pathologic correlation. Acta Radiol 48(8): 921-933.
- Lee KS, Park KH, Lee S, Kim JY, Seo SS (2005) Adenocarcinoma arising in a vaginal mullerian cyst: a case report. Gynecol Oncol 99(3): 767-769.
- Cope AG, Laughlin-Tommaso SK, Famuyide AO, Gebhart JB, Hopkins MR, et al. (2017) Clinical manifestations and outcomes in surgically managed Gartner duct cysts. J Minim Invasive Gynecol 24(3): 473-477.
- Abd-Rabbo MS, Atta MA (1991) Aspiration and tetracycline sclerotherapy: a novel method for management of vaginal and vulval Gartner cysts. Int J Gynaecol Obstet 35(3): 235-237.






























