Massive Hemoperitoneum from a Ruptured Corpus Luteal Cyst
Kishore Pandit1*, Shital Potdar1, Sunita Pandit1, Harshal Tukaram Pandve2 and Shravasti Pandit2
1Aundh Institute of Medical Sciences Hospital & Research Center, India
2SMT Kashibai Navale Medical College, India
Submission: January 16, 2017; Published: January 23, 2018
*Corresponding author: Kishore Pandit, AIMS Hospital & Research Center, Aundh, Pune, Maharashtra, Pin code: 411007, india, Email: drkspandit@gmail.com
How to cite this article: Kishore P, Shital P, Sunita P, Harshal T P, Shravasti P. Massive Hemoperitoneum from a Ruptured Corpus Luteal Cyst. JOJ Case Stud. 2018; 5(5) : 555672. DOI: 10.19080/JOJCS.2018.05.555672.
Abstract
Corpus luteum cysts are functional cysts of the ovary. If conception does not occur, the corpus luteum typically dissipates; however, they may collect with fluid or blood and form a cyst that can rupture. Although cyst rupture is generally benign, causing mild pain to the patient, it can result in massive hemoperitoneum requiring emergent surgical intervention. While hemorrhagic ovarian cysts are quite common, rupture leading to spontaneous severe hemoperitoneum is much more rare, and it can be a life-threatening event. We have discussed2 cases of patients presenting with acute abdominal pain, and large-volume hemoperitoneum and anemia which were found to have a hemorrhagic corpus luteal cyst at laparoscopic exploration.
Introduction
The corpus luteum is a temporary hormone secreting remnant of a mature ovarian follicle after it ruptures to release an ovum into the fallopian tube. Its main function is to secrete progesterone to maintain early pregnancy till placenta is developed by 8-10 weeks. If fertilization does not occur, the corpus luteum involutes several days after ovulation (corpus albicans), shrinks and stops producing progesterone, resulting in menstruation. However, the corpus luteum may fill with blood or other fluids forming a cyst and rupture [1]. Abdominal pain caused by a ruptured corpus luteum cyst is a common complaint in a woman of childbearing age. The complaints are usually self-limited to pain. Only in rare cases they can lead to massive hemoperitoneum requiring surgical management.
Prompt and appropriate evaluation of acute abdomen is always a priority because of the potential need for emergent surgery. In women of reproductive age, the differential diagnosis includes a number of gynecologic conditions, and ultrasound findings may closely mimic ectopic pregnancy [2].
Spontaneous massive hemoperitoneum secondary to a hemorrhagic corpus luteum cyst is an exceedingly rare, but potentially life-threatening presentation, with few cases reported in the literature. Herewith is a mention of two cases of ruptured corpus luteal cyst with massive hemoperitoneum, which presented as acute abdomen and were managed efficiently by laparoscopic intervention.
Case Report 1
A 24-year-old female presented to an emergency department with emesis and severe abdominal pain for the previous 4-6h. Her last menstrual date was about 20 days ago, with regular menstrual history; and moderate flow.
Her initial heart rate was 100 beats/minute, feeble, with a measured blood pressure of 100/60 mm Hg. On examination, she was very pale, and was noted to have diffuse tenderness and guarding on per abdominal examination. However there were no signs of abnormal coagulation profile.
On initial laboratory work-up, she was noted to have a hemoglobin (Hgb) of 7g/dL, hematocrit of 23.6%, and platelet count of 2.5L; with normal prothrombin time and activated partial thromboplastin time. Urine pregnancy test was negative. She was started with intravenous fluid resuscitation and 2 packed red blood cells were transfused with 4 units of fresh frozen plasma.
An ultrasound scan of the abdomen and pelvisdone revealed a thick walled cystic lesion of approx. size 54 x 46mm seen in right adnexa abutting the uterus showing extensive peripheral vascularity, echogenic mural component also seen within the cyst. Heterogeneous area suggestive of organized hematoma was seen surrounding the right adnexal cyst. Moderate hemorrhagic fluid was seen in peritoneal cavity. It was masquerading a ruptured ectopic gestation with massive hemopertoneum.
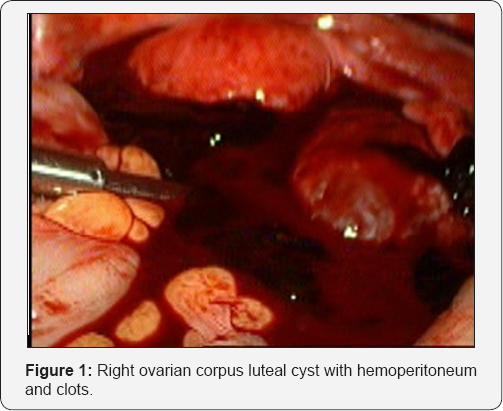
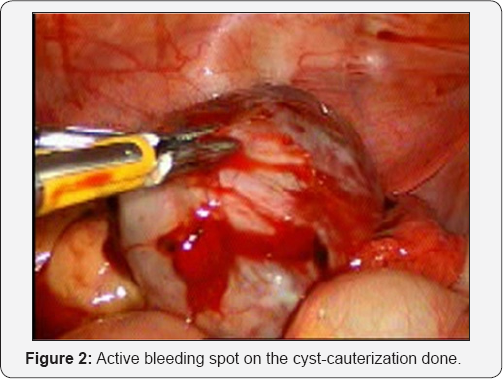
After the patient was resuscitated and hemodynamically stable, she was taken to the operating room for a laparoscopy. On exploration, the patient was found to have approximately 2L of hemoperitoneum, about 500cc clots, 4cm x 5cm large right ovarian corpus luteal cyst (Figure 1) was noted with rupture. Active bleeding was noted from cyst capsule (Figure 2).
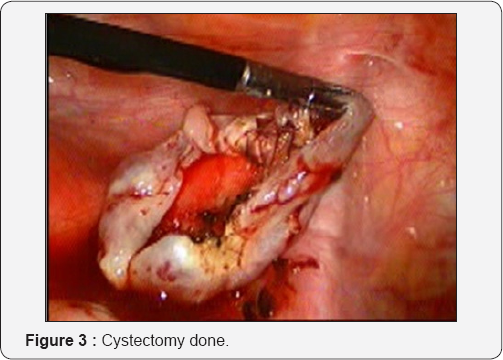
Post-operatively, the patient recovered well with stabilization of her hematocrit and platelet count. She had appropriate return of bowel function and was discharged on post-operative day two. Peripheral blood counts at discharge showed aHgb of 9.2g/ dL, WBC 8,900 c and platelets 1.88L. The patient had a scheduled outpatient follow-up appointment with the hematology service two weeks after discharge. She had not suffered any further bleeding episodes or abdominal complaints. Coagulation profile, coagulation factors were normal.
Case Report 2
A 45-year old female presented to the emergency department with complaints of lower abdominal pain along with 2-3 episodes of emesis with onset approximately 4-5 hours prior toad mission. Over the next several hours, she experienced several similar episodes of pain of variable intensity that were also associated with eating. She also complained of constipation and inability to pass flatus. Her last menstrual period was nine days prior and normal in timing and duration. She was sexually active and did not use birth control. She denied vaginal bleeding and had no known gynecologic problems. She denied urinary symptoms and reported no previous abdominal surgeries. She was a known case of ischaemic heart disease, with angioplasty done a month ago and was on antiplatelet medications since then.
Vital signs upon arrival revealed a temperature of 36.9°C, blood pressure 106/64mmHg, heart rate 84bpm,respiratory rate 16bpm, and SaO2 100% on room air, no pallor. Her abdominal examination was remarkable for diffuse tenderness throughout the entire abdomen with sluggish bowel sounds. Voluntary guarding with palpation was noted.
Pertinent laboratory results included white blood cell count 10,500/uL with hemoglobin 10.3g/dL. Serum electrolytes, liver function tests, lipase and urinalysis were normal. Coagulation profile was normal. Urine pregnancy test was negative and serum beta-HCG was <10IU (non-pregnant <10IU).
Abdominal ultrasound revealed a large subserosal fibroid of approx. size 84 x 55 x 103mm seen along the fundus of uterus. On clinical suspiscion of intestinal obstruction caused due to the fibroid, abdominal erect X-ray was done but no significant air fluid levels were seen. The clinical findings were not consistent with the ultrasound findings, therefore MRI scan of the abdomen/pelvis was recommended to better delineate possible intra abdominal and/or pelvic pathology. This study revealed a complex left ovarian mass and a large amount of intraperitoneal fluid with a radio density of blood. Tumour markers Ca 125, CEA, AFP and BhCG were noted to be normal.
After reviewing the laboratory, ultrasound and MRI studies the diagnosis was a possible ruptured ovarian cyst and recommended emergent exploratory laparoscopy. Upon exploration of the abdomen, organised hematoma 10cm x 10cm was noted in the pelvis. Hemoperitoneum with old dark red blood about 1.5 litres was evacuated. Right side ruptured corpus luteal cyst was seen with no evidence of active bleeding. Bilateral tubes, left ovary and uterus were normal. The liver and abdominal organs were normal.
The patient did not need blood transfusion. Postoperative hemoglobin levels remained stable and pain improved. The patient was discharged on the second postoperative day with restarting her antiplatelet medications as per the cardiologist. When seen in the OBGYN clinic two weeks later she was symptom-free and her hemoglobin level was similar to the day of hospital discharge.
Discussion
Ovarian cysts occur commonly in menstruating women aged 18-35 years and are commonly identified by ultrasound. Two types of functional ovarian cysts are described- follicular cysts and corpus luteum cysts. The corpus luteum is a highly vascular structure. The rate of blood flow to the corpus luteum exceeds any other adult organ (per unit of tissue); the increased blood flow is needed to deliver substrates for hormone production and to nurture the rapidly dividing luteal cells [3]. The highly vascular nature of the corpus luteum is reflected by its oxygen consumption which is estimated to be 2-6 times that of the liver, kidney and heart (per unit of tissue) [1,4].
Corpus luteum cysts are thin-walled, functional vascular structures, and most of them are predisposed to rupture [5]. Rupture of corpus luteum cyst is one of the major gynecologic causes of hemoperitoneum. The etiology for cyst rupture is not known, although it has been suggested that the increased vascularity of the ovary in the luteal phase and pregnancy may predispose to rupture of a corpus luteal cyst. Corpus luteal cysts arise due to the rapid growth and high vascularity of the corpus luteum resulting in intraluteal hemorrhage and the formation of a hemorrhagic cyst. Ongoing bleeding into the cyst can result in rapid enlargement, spontaneous rupture and leakage of blood into the peritoneal cavity.
While some hemorrhage associated with ovarian cyst rupture has unclear etiology, there are recognized risk factors. These include abdominal trauma and anticoagulation therapy [4]. The right ovary seems predisposed to rupture more than the left one, as seen in both of our cases [5]. One of the possible explanations for this predisposition is the protection of left ovary from trauma by the cushioning of the recto-sigmoid colon [6].
Typically at the time of rupture, there may be sharp and sudden onset of pain, which has no typical characteristics. Blood loss can vary from very little bleeding to hypovolemic shock [6]. Abdominal and/or pelvic pain may occur with any of these complications. The incidence of this complication is not reported; practicing gynecologists relate this as rare but recognized. More recent case reports of massive hemoperitoneum from a ruptured corpus luteum cyst are associated with systemic anticoagulation, coagulation disorders, von Willebrand disease, and sickle cell anemia [3,7-9]. Hallatt et al. [6] described the first large series of patients with corpus luteum hemorrhage and hemoperitoneum [6]. They noted that this entity occurs at all stages of a woman's reproductive life, and that a wide range of volumes of hemoperitoneum can be found at the time of exploration. Corpus luteum hemorrhage may be a cause of spontaneous hemoperitoneum in patients with bleeding disorders.
Taking a detailed bleeding history on all surgical patients is critical, and maintaining a wide differential diagnosis can aid in appropriate work-up and optimize peri-surgical management. In patients presenting with corpus luteum cyst with significant bleeding, a hematology consult should be considered.
According to Hallatt et al. [6] the hemorrhage from a ruptured corpus luteum cyst is likely to be less than in an ectopic pregnancy and likely to be non-recurrent once it stops. Corpus luteal cysts are commonly identified as incidental structures on pelvic ultrasound studies.
Multiple sonographic patterns have been defined for hemorrhagic ovarian cyst and it has also been called the "great imitator" [10]. Corpus luteum cyst rupture with intra-abdominal hemorrhage may appear ultrasonographically identical to a ruptured ectopic pregnancy as in our case a negative serum pregnancy test may be a discerning feature [6,11]. Computed tomography scan of the abdomen/pelvis is of limited value and usually supports the diagnosis of ruptured ectopic pregnancy- again a negative serum pregnancy test should suggest an alternate diagnosis [12].
Although the sonographic patterns of hemorrhage within an ovarian cyst have been well known, the findings related with cyst rupture and hemorrhage have not been well described in the literature [11].
Consequently, patients with a ruptured ovarian cyst are frequently misdiagnosed with unrelated disorders [2]. In one study, the hemoperitoneum was found to be the dominant imaging feature rather than the cyst itself [11]. Hemoperitoneum from a ruptured hemorrhagic ovarian cyst exhibits imaging features similar to those of hemoperitoneum from other sources such as ruptured ectopic pregnancy [13].
Hemoperitoneum resulting from ruptured corpus luteum cyst have been described since the early 1900s and is frequently misdiagnosed as ruptured ectopic pregnancy, acute appendicitis, ovarian torsion and endometriosis [14,15].
The diagnosis is mainly based on high clinical suspicion, laboratory data and ultrasound findings. Historically, the major differential diagnosis is ectopic pregnancy.
Furthermore, coincidental presence of corpus luteum cyst rupture with ectopic pregnancy has been reported [2,10,11]. Therefore, the possibility and occurrence of corpus luteum cyst rupture should be kept in mind even when the presence of intrauterine or extrauterine pregnancy is confirmed.
Management of corpus luteum haemorrhage is conservative or surgical [16,17,18]. Therapy for ruptured corpus luteal cysts with intraabdominal hemorrhage must be tailored to the patient. Our patients presented with symptoms and findings suggestive of acute abdominal pain mimicking ectopic pregnancy in first case and intestinal obstruction in the second. Other common differentials for a young female with abdominal pain include gastritis, peptic ulcer disease, gastroesophageal reflux disease, ectopic pregnancy, pyelonephritis, pancreatitis, and ovarian related conditions such as pelvic inflammatory disease, ovarian torsion, and cyst rupture.
Observation, pain control and serial hemoglobin monitoring may be appropriate for select cases as in our second case where in the patient was hemodynamically stable, but signs of blood loss or hypovolemic shock should prompt immediate laparoscopic intervention as was done in our first case.
Ultrasonic evidence of large amounts of peritoneal fluid and severe pain is indication for operative intervention [16-18]. In corpus luteum haemorrhage, oophorectomy is rarely necessary [18]. This form of minimally invasive surgery provides potential benefits for improved cosmetic appearance, shorter hospital stay, reduced postoperative pain, and earlier postoperative return to daily activities. In patients with recurrent corpus luteum haemorrhage, oral contraceptives are used to suppress ovulation [17].
Conclusion
Massive hemoperitoneum resulting from a ruptured corpus luteum cyst is rare, but potentially life-threatening if not diagnosed and treated emergently. Abdominal pain in a young female is a frequent complaint in the emergency department and massive hemoperitoneum from a ruptured corpus luteum cyst should be in the differential diagnosis for all females of child bearing age presenting with abdominal pain, regardless of the location.
The differential diagnosis should include ectopic pregnancy, acute trauma, in certain patients; an underlying hematologic condition should be suspected and ruled out. Although most patients require only observation, some need analgesics for pain control and laparoscopy or laparotomy for diagnosis or to achieve hemostasis.
References
- Niswender GD, Juengel JL, Silva PJ, Rollyson MK, McIntush EW (2000) Mechanisms controlling the function and life span of the corpus luteum. Physiol Rev 80(1): 1-29.
- Raziel A, Ron-El R, Pansky M, Arieli S, Bukovsky I, et al. (1993) Current management of ruptured corpus luteum. Eur J Obstet Gynecol Reprod Biol 50(1): 77-81.
- Swann RT, Bruce NW (1987) Oxygen consumption, carbon dioxide production and progestagen secretion in the intact ovary of the Day-16 pregnant rat. J Reprod Fertil 80(2): 599-605.
- Gupta N, Dadhwal V, Deka D, Jain SK, Mittal S (2007) Corpus luteum hemorrhage: rare complication of congenital and acquired coagulation abnormalities. J Obstet Gynaecol Res 33(3): 376-380.
- Tang LC, Cho HK, Chan SY, Wong VC (1985) Dextropreponderance of corpus luteum rupture. A clinical study. J Reprod Med 30(10): 764-768.
- Hallatt JG, Steele CH, Snyder M (1984) Ruptured corpus luteum with hemoperitoneum: a study of 173 surgical cases. Am J Obstet Gynecol 149(1): 5-9.
- Hackethal A, Ionesi-Pasacica J, Kreis D, Litzlbauer D, Tinneberg HR, et al. (2011) Feasibility of laparoscopic management of acute haemoperitoneum secondary to ruptured ovarian cysts in a haemodynamically unstable patient. Minim Invasive Ther Allied Technol 20(1): 46-49.
- Terzic M, Likic I, Pilic I, Bila J, Knezevic N (2012) Conservative management of massive hematoperitoneum caused by ovulation in a patient with severe form of von Willebrand disease--a case report. Clin Exp Obstet Gynecol 39(4): 537-540.
- Andikyan V, Ronald J, Bowers C (2010) Massive hemoperitoneum secondary to ruptured corpus luteum cyst of pregnancy in 17-year old female with hemoglobin SC disease. The Internet Journal of Gynecology and Obstetrics 12(2).
- Jeffrey RB, Laing FC (1982) Echogenic clot: a useful sign of pelvic hemoperitoneum. Radiology 145(1): 139-141.
- Yoffe N, Bronshtein M, Brandes J, Blumenfeld Z (1991) Hemorrhagic ovarian cyst detection by transvaginalsonography: The great imitator Gynecol Endocrino l5(2): 123-129.
- Swire MN, Castro-Aragon I, Levine D (2004) Various sonographic appearances of the hemorrhagic corpusluteum cyst. Ultrasound Q 20(2): 45-58.
- Hertzberg BS, Kliewer MA, Paulson EK (1999) Ovarian cyst rupture causing hemoperitoneum: imaging features and the potential for misdiagnosis. Abdom Imaging 24(3): 304-308.
- Waters CH (1918) Hemorrhage into an ovarian cyst simulating ectopic pregnancy. JAMA 70(5): 295-296.
- Phaneuf LE (1924) Intraperitoneal hemorrhage from ruptured ovarian cyst. JAMA 83(9): 658-662.
- Hoffman R, Brenner B (2009) Corpus luteum hemorrhage inwomen with bleeding disorders. Womens Health (Lond) 5(1): 91-95.
- Payne JH, Maclean RM, Hampton KK, Baxter AJ, Makris M (2007) Haemoperitoneum associated with ovulation in women with bleeding disorders: the case for conservative management and the role of the contraceptive pill. Haemophilia 13(1): 93-97.
- Jamal A, Mesdaghinia S (2002) Ruptured corpus luteum cysts and anticoagulant therapy. Int J Gynaecol Obstet 76(3): 319-320.






























