Impact of Prenatal Diagnosis on the Outcome of Pulmonary Atresia with Intact Ventricular Septum
Abdullah Al Abdulgader1,2* and Lamees Abdullah Al Abdulgader3
1Congenital Cardiologist & Invasive Electro physiologist, Prince Sultan Cardiac Center, Saudi Arabia
2HeartMath Institute, Saudi Arabia
3College of Medicine-King Faisal University, Saudi Arabia
Submission: August 08, 2017; Published: August 29, 2017
*Correspondence author: Abdullah Al Abdulgader, Congenital Cardiologist & Invasive Electro physiologist, Prince Sultan Cardiac Center, P.O.Box 9596, Hofuf, Al-Ahsa 31982, Saudi Arabia, Tel: 00966505920398; Email: kidsecho@yahoo.com
How to cite this article: Abdullah A A, Lamees A A A. Impact of Prenatal Diagnosis on the Outcome of Pulmonary Atresia with Intact Ventricular Septum. J Cardiol & Cardiovasc Ther 2017; 7(3): 555715. DOI: 10.19080/JOCCT.2017.07.555715.
Abstract
Prenatal diagnosis of pulmonary atresia with intact ventricular septum (PAIVS) was useful for planning delivery. It was hypothesized that it can be of benefit on postnatal outcome. The objective of this study was to compare the outcome of prenatal versus postnatal diagnosis of PAIVS in terms of mortality and morbidity. This is a retrospective study of the outcome of all cases of PAIVS presenting in utero and in the postnatal life during the period between January 2011 and December 2016 in a tertiary referral center. Twenty -eight patients with PAIVS were included in this study and distributed equally within two groups prenatal and postnatal. The main outcome measure was survival rate in first 12 months of postnatal life in a clinically well doing status. Three mortalities was the outcome in postnatal group compared to one mortality in the prenatal group. On the other hand, morbidity was higher in the prenatal group (4 vs 2 patients). The number of clinically well doing patients following operative interference was equal in both group (9 patients in each). It can be concluded that the impact of antenatal diagnosis can be restricted on the increased incidence of morbidities at the expense of mortalities with no effect on the number of well being infants.
Background
Pulmonary atresia intact with ventricular septum (PAIVS) is a rare congenital cardiac lesion characterized by heterogeneous right ventricular development, imperforate pulmonary valve, and possible extensive ventriculocoronary connections. PAIVS occurs in 4.5-8 per 100,000; live births [1] and 0.7-3.1% of patients with congenital heart disease. The overall probability of survival for patients with PAIVS is approximately 65-82% at age of one year and 76% at age 5 years [2]. The strategies of biventricular repair, single ventricle palliation, and heart transplantation allow for equal outcome among all anatomic subtypes [3]. Prenatal diagnosis (PRD) was useful for planning delivery; it was hypothesized that it can be benefit on postnatal outcome [4].
Objective
The aim of this study is to compare the outcome of PRD of PAIVS versus only postnatal diagnosis (PTD) as regards for mortality and morbidity.
Setting
Tertiary referral center for pediatric cardiology and cardiac surgery.
Design
This is a retrospective study reviewing and comparing the outcome of prenatal diagnosis (PRD) versus postnatal diagnosis (PND) of PAIVS during the period between January 2011 and December 2016.
Patients
Twenty-eight patients equal gender distribution 14 females and 14 males with diagnosed with PAIVS were included in this study. PRD was performed in 14 patients and the diagnosis was confirmed during postnatal period, while only PND was performed in another 14 patients. PRD was done during the period between 12th and 20th weeks of pregnancy
Main outcome measure
Survival up to 12 months of postnatal life and doing reasonable as regard for disappearance of cyanosis, absence of heart failure, lack of significant respiratory symptoms, good feeding and reasonable weight gain. Descriptive data analysis and comparison of outcome was performed. Chi squared test was used to detect any significant difference between categorical variables. P value level was set significant at <0.05.
Results
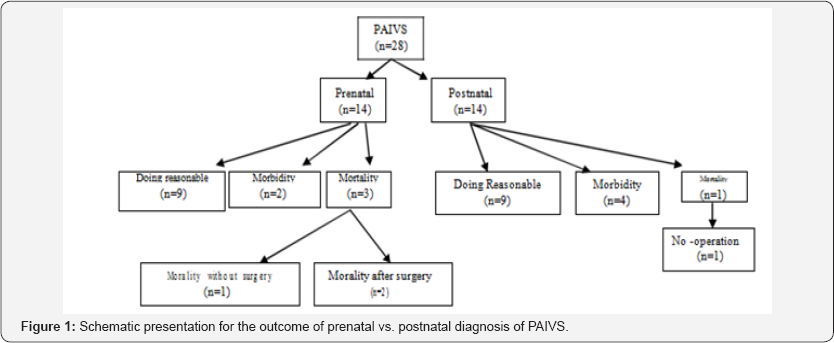
Twenty -eight patients' equal gender distribution 14 females and 14 males with diagnosed with PAIVS were included in this study. PRD was performed in 14 patients and the diagnosis was confirmed during postnatal period, while only PND was performed in another 14 patients Figure 1.
All patients were delivered at term and the mode of delivery of babies was [28(87%) versus 4(15%); P,0.0001] for normal vaginal delivery and caesarean section respectively. About 7% of patients in both groups were born with low birth weight ,2.5kg. Apgar scores at 5 and 10 minutes are normal for all babies. Extra -cardiac anomalies were found in tow patients (asplenia in one patient and omphalocele in another). All cases were subjected to surgical procedures by one surgeon.
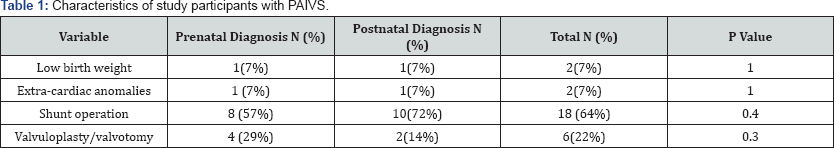
Eighteen patients (64%) in study were subjected to shunt operations (57% versus 72%) for (72%) in the PRD and PTD group respectively. There was no statistically significant difference between the two groups in number of patient who underwent shunt operation (P=0.4). Additionally, 6 patients were subjected to valuloplasy/valvuotomy, of them (29% versus. 14%) for PRD and PND respectively. There was no statistically significant difference between the two groups in proportion of patient who had the last procedure (P=0.3), Table 1.
Three deaths occurred in the PRD group; two patients died at age of one week without prior operation and the third patient died at age of 9 months as status post-shunt operation. In PRD group only one patient died at the age of one week without prior operation. On the other hand, morbidity was higher in the PND group compared to PRD group (28.6% vs. 14.3%; P=0.4), but the difference was no statistically significant. The number of clinically well doing patients following operative interference was equal in both groups. There was no significant difference in clinically doing reasonable, morbidity and mortality between the two study groups.
Discussion
PRD has important implications for pregnancy outcome, in particular for univentricular lesions. However, the present mode of obstetric routine ultrasound scanning fails to identify most ductus arteriosus dependent cardiac lesions with a predictable need for early postnatal intervention [5]. The easiness of prenatal detection of a ductus-dependent pulmonary circulation is a strong indication of the presence of severe pulmonary stenosis or artesia. Its diagnosis allows avoidance of maternal administration of durgs with constrictive effects upon the ductus, interdisciplinary planning of perinatal management, early postnatal confirmation of the diagnosis, and early postnatal intervention, in particular administration of prostaglandins to prevent life-threatening ductal closure [6]. Fetal hemodynamic information was useful for making decisions not only after birth, but also in utero, and may eventually result in improving the prognosis of babies with PA/CPS (critical pulmonary stenosis)as well as it may suggest the possible pathogenesis of PA/CPS in utero [7].
In our study, one year survival rate in the PND group was higher than in the PRD (93% vs. 78%; P=0.3) though it was not statistically significant. However, patients who were in a clinically good status were equal in both groups (64%). This means that the positive impact of antenatal diagnosis can be restricted on the increased incidence of morbidities at the expense of mortalities after delivery. The lack of significant outcome difference between both groups can be attributed to the better growing health services and medical experiences for early picking up of patients with congenital heart lesions particularly the cyanotic types. In an English study, done by Daubeny et al. [8], they reported that termination of pregnancy has resulted in an important reduction in the live-born incidence in Mainland Britain and the probability of survival at one year was 65% and was the same for live-born infants whether or not a fetal diagnosis had been made. In another study by Rychik et al. [3], one year survival rate was 82% after surgical correction of PAVIS. Tzifa et al. [9], in their report showed that postnatal diagnosis of pulmonary atresia was associated with greater cyanosis at presentation, but this does not translate into greater neonatal morbidity or mortality provided that early recognition and prompt initiation of prostaglandin E therapy occur
Patient of low birth weight may have higher risk factor for death, regardless whether the patient underwent an operation. Weight at the time ofthe surgical procedure has been recognized by several studies of large sample sizes as an independent risk factor, and population-based study has been identified low birth weight as a risk factor [10-14]. In some centers there was a strategy of immediate operation while in others, a chance was given for them to grow, unfortunately both trials had poor outcome. Current reports recommend that early surgical intervention in infants born with low weight is technically possible with good results and indeed is a better choice [15].
Some anomalies were found to be a poor prognostic indicators such as major RV dilatation, abnormalities of the TV, such as dysplasia and Ebstein's malformation, and hypoplastic pulmonary arteries [16]. Coles et al. [10], 11 found that the presence of Ebstein's malformation was an independent risk factor for poor outcome. Low weight at the time of surgical intervention is associated with increased mortality in patients undergoing several types of cardiovascular procedures. These data do not allow assessment of specific risks or benefits of any particular treatment strategy. However, they do support the need for prospective analysis of specific treatment strategies for these high-risk patients [17]. Polat T et al. [18], reported that prenatal intervention for fetuses with PA/IVS has the potential to improve growth of the RV and the prospect of a biventricular outcome after birth when valvulotomy of the pulmonary valve was performed in a fetus with PA/IVS at 28 weeks. Following the procedure there was an improvement in fetal hemodynamic. They concluded that in utero perforation and dilation of the PV in mid gestation fetuses with PA/IVS is technically feasible and this results are promising and may be associated with improved right heart growth and postnatal outcome [18].
Conclusion
This study does not show significant difference in outcome between prenatal diagnoses in term of morbidity, mortality and survival of pulmonary atresia. Since prenatal group constitute the sever spectrum of the disease. The degree of severity was conceivably the reason behind the easiness prenatal detection. The absence of statistical significance was due to relative severity of disease and malformation in both groups. Because of this prenatal diagnosis is still conceivably of favorable outcome. Larger volume studies of this sub type of congenital heart disease with native anatomical comparisons are highly needed to increase the weight of evidence in this direction. The value of critical autopsy dissection and evaluation is also of paramount significance in comparison of prenatal and postnatal groups of pulmonary atrisa intact ventricular septum.
Even though, prenatal diagnosis has other benefits which include parental counseling, delivery planning, postnatal care plan for neonate, early referral to specialized center, improvements in preoperative condition and early surgical intervention.
Acknowledgement
This study was carried out as a limb project of: The international project of Genetic and environmental risk factors of Congenital Heart Diseases in Arabian Peninsula including: Kingdom of Saudi Arab, Arab Gulf Countries and Republic of Yemen
Reference
- Leonard H, Derrick G, O'Sullivan J, Wren C (2000) Natural and unnatural history of pulmonary atresia. Heart 84(5): 499-503.
- Kutsche LM, Van Mierop LH (1983) Pulmonary atresia with and without ventricular septal defect: a different etiology and pathogenesis for the atresia in the 2 types? Am J Cardiol 51(6): 932-935.
- Rychik J, Levy H, Gaynor JW, DeCampli WM, Spray TL (1998) Outcome after operations for pulmonary atresia with intact ventricular septum. J Thorac Cardiovasc Surg 116(6): 924-931.
- Favilli S, Giusti S, vangi V, Pollini I, Redaelli S (2003) Pulmonary atresia or critical pulmonary stenosis with intact interventricular septum diagnosed in utero: echocardiographic findings and post-natal outcome. Pediatr Med Chir 25(4): 266-268.
- Jaeggi ET, Sholler GF, Jones ODH, Cooper SG (2001) Comparative analysis of pattern, management and outcome of pre-versus postnatally diagnosed major congenital heart disease: a population-based study. Ultrasound Obstet Gynecol 17(5): 380-385.
- Mielke G, Steil E, Kendziorra H, Goelz R (1997) Ductus arteriosus- dependent pulmonary circulation secondary to cardiac malformations in fetal life. Ultrasound Obstet Gynecol 9(1): 25-29.
- Nishibatake M, Matsuda Y, Kamitomo M, Ibara S, Sameshima H (1999) Echocardiogrophic findings of pulmonary atresia or critical pulmonary stenosis and intact ventricular septum in utero. Pediatr Int 41(6): 716721.
- Daubeney PE, Sharland GK, Cook AC, Keeton BR, Anderson RH (1998) Pulmonary atresia with intact ventricular septum: Impact of fetal echocardiography on incidence at birth and postnatal outcome. UK and Eire Collaborative study of pulmonary Atresia with intact ventricular septum 98(6): 562-566.
- Tzifa A, Barker C, Tibby S, Simposn J (2007) Prenatal diagnosis of pulmonary atresia: Impact on clinical presentation and rarly outcome. Arch Dis Child Fetal Neonatal Ed 92(3): F199-F203.
- Coles JG, Freedom RM, Lightfoot NE, Dasmahapatra HK, Williams WG, et al. (1989) Long-term results in neonates with pulmonary atresia and intact ventricular septum. Ann Thorac Surg 47(2): 213-237.
- Bull C, Kostelka M, Sorensen K, de Leval M (1994) Outcome measures for the neonatal management of pulmonary atresia with intact ventricular septum. J Thorac Cardiovasc Surg 107(2): 359-366.
- Hanley FL, Sade RM, Blackstone EH, Kirklin JW, Freedom RM, et al. (1993) Outcomes in neonatal pulmonary atresia with intact ventricular septum. J Thorac Cardiovasc Surg 105(3): 406-427.
- Ekman Joelsson BM, Sunnegardh J, Hanseus K, Berggren H, Jonzon Jogi P, et al. (2001) The outcome of children born with pulmonary atresia and intact ventricular septum in Sweden from 1980 to 1999. Scand Cardiovasc J 35(3): 192-198.
- Daubeney PE, Delany DJ, Anderson RH, Sandor GG, Slavik Z, et al. (2002) Pulmonary atresia with intact ventricular septum: range of morphology in a population-based study. J Am Coll Cardiol S9(10): 1670-1679.
- Ashburn MD, Blackstone EH, Wells WJ, Jonas RA, Pigula FA, et al. (2004) Determinants of mortality and type of repair in neonates with pulmonary atresia and intact ventricular septum. J Thorac Cardiovasc Surg 127(4): 1000-1007.
- Starnes VA, Pitlick PT, Bernstein D, Griffin ML, Choy M, et al. (1991] Ebstein's anomaly appearing in the neonate. A new surgical approach. J Thorac Cardiovasc Surg 101(6): 1082-1087.
- Curzon CL, Milford-Beland S, Li JS, O'Brien SM, Jacobs JP, et al. (2008) Cardiac surgery in infants with low birth weight is associated with increased mortality: analysis of the Society of Thoracic Surgeons Congenital Heart Database. J Thorac Cardiovasc Surg 135(3): 546-551.
- Polat T, Danisman N (2012) Pulmonary valvulotomy in a fetus with pulmonary atresia with intact ventricular septum: First experience in Turkey. Images Paediatr Cardiol 14(3): 6-11.






























