A 3 Year Old Case of Juvenile Mitral Stenosis- the Youngest Case Reported
Ranjan Modi1*, SV Patted2, Prabhu Halkati2, MD Dixit2 and Veeresh Manvi2
1Fortis Escorts Heart Institute, India
2KLE Hospital and MRC, JN Medical College, India
Submission: May 05, 2017; Published: June 29, 2017
*Corresponding author: Ranjan Modi, Fortis Escorts Heart Institute, Okhla, New Delhi, India, Tel: 09844917110; Email: Ranjan_Modi@Hotmail.com
How to cite this article: Ranjan M, S Patted, Prabhu H, M Dixit, Veeresh M. A 3 Year Old Case of Juvenile Mitral Stenosis- the Youngest Case Reported. J Cardiol & Cardiovasc Ther 2017; 6(2): 555682. DOI:10.19080/JOCCT.2017.05.555682
Abstract
Rheumatic heart disease is a well-known entity in the developing world. The commonest sequelae of rheumatic carditis are mitral stenosis (MS). MS can present at a very young age with severe symptoms. We describe here a case of juvenile rheumatic MS in a 3 year old child with severe pulmonary hypertension.
Background
Rheumatic fever and rheumatic heart disease (RHD) continues to be a significant cause of morbidity and mortality in developing countries including India. It constitutes the most common form of valvular heart disease in India. The reported prevalence of RHD is 1.0 to 5.4 per 1,000 school children in our country [1]. Rheumatic mitral stenosis (MS) is a common problem in young children and adolescents and it can often lead to severe symptoms [2]. MS is a condition characterized by structural abnormality of the mitral valve apparatus that results in obstruction to left ventricular inflow. The most common cause of MS is rheumatic carditis. Other causes are extremely uncommon and include congenital MS, mitral annular calcification (MAC), carcinoid syndrome, mucopolysaccharidosis, Fabry's disease, Whipple's disease, amyloidosis and methysergide therapy [1].
Recurrent and severe episodes of rheumatic fever can lead to early development of RHD that may be confused with congenital causes of mitral valve disease in the young population. RHD follows rheumatic fever (RF), as a non-suppurative manifestation of group A beta haemolytic streptococcal (GAS) pharyngitis. RF is widely accepted as an immunological disorder following GAS infection. Rheumatic valvulitis most commonly affects the mitral valve (70% to 75%) followed by combined mitral and aortic involvement (20% to 25%) [1,2].
Case Report
Our patient a 3 year old boy, weighing 9Kgs, with a history of recurrent cough with expectoration since last one year presented with recent worsening of dyspnoea associated with paroxysmal nocturnal dyspnea. His medical history did not have any history suggestive of rheumatic fever. On examination patient was dyspneic at rest with marked tachycardia. The precordial examination revealed precordial buldge, parasternal and epigastic pulsations, loud S1, parasternal Heave with palpable and loud P2, with a long Mid-diastolic murmur with pre systolic attenuation at the apex.
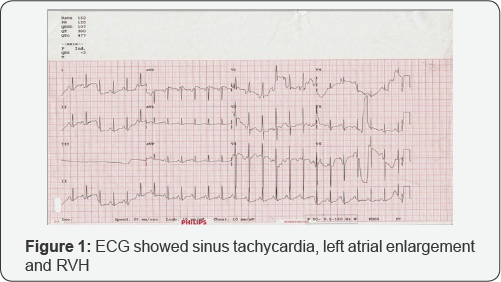
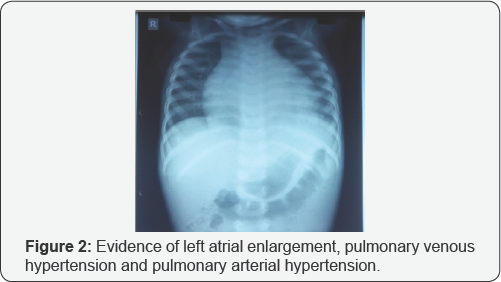
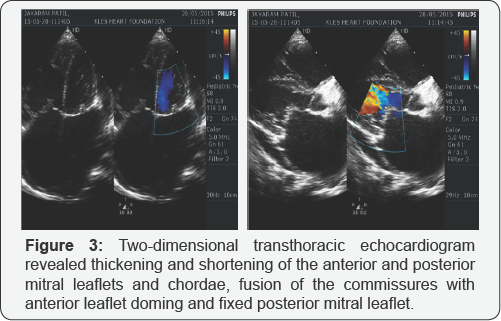
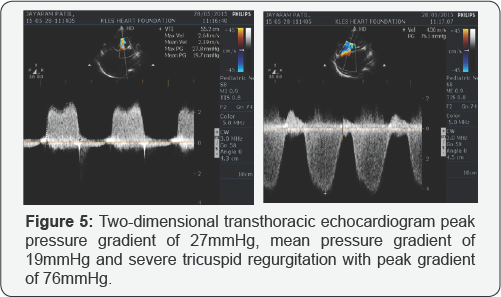
The electrocardiogram (ECG) showed sinus tachycardia with rightaxis deviation (+110°), left atrial enlargement and right ventricular hypertrophy (RVH) (Figure 1). The chest x-ray showed evidence of left atrial enlargement, pulmonary venous hypertension and pulmonary arterial hypertension (Figure 2) . The two-dimensional transthoracic echocardiogram (TTE) revealed thickening and shortening of the anterior and posterior mitral leaflets and chordae, fusion of the commissures with anterior leaflet doming and fixed posterior mitral leaflet (Figure 3) , turbulent mitral inflow jet, severe subvalvular stenosis with peak pressure gradient of 27mmHg, mean pressure gradient of 19mmHg and mitral valve opening of 0.35cm2 by planimetry (Figure 4). The patient also had severe tricuspid regurgitation with peak gradient of 76mmHg (Figure 5) and severe pulmonary hypertension, estimated right ventricular systolic pressure 91mmHg. With all these echocardiographic evidences and clinical condition of congestive cardiac failure, a diagnosis of severe MS and severe pulmonary artery hypertension (PAH) was concluded. The patient clinical condition was initially stabilized by strict bed rest and decongestive therapy with diuretics. After intial stabilization the patient was taken for commissurotomy.

The patient was taken for commissurotomy followed by mitral valve repair. During operative repair inspection revealed pericardial inflammation with thickened, scarred, severe commissural and subvalvular fusion, which were suggestive of RHD. Commissurotomy was done with annuloplasty using 18mm Goretex Ring. Mitral valve replacement was done using 18mm Medtronic aortic valve in inverted position. Post operatively the patient was not doing well and expaired ofter 3day of surgary.
Discussion
In most of the developed countries the prevalence of rheumatic fever has declined in past decades, but in the developing countries like India, the disease is still prevalent. Isolated severe rheumatic mitral stenosis in children and young adults is frequently encountered up to 25% of patients. The term Juvenile mitral stenosis (JMS) stands for patients younger than 20 years of age [3].
JMS is characterized by severe stenosis of the mitral valve, a high prevalence of severe PAH and pulmonary venous hypertension, less often has Atrial Fibrillation and Left Atrium Dilatation [4]. Severe subvalvular pathology is almost universally extensive and is grade 3 or 4 in most of these patients [5]. Severe PAH is seen in over one-third of these patients. Recurrence of RF is more common in these patients, given their age. Balloon Mitral Valvotomy, closed surgical commissurotomy and Mitral Valve surgery are approaches available for this subgroup of patient of Juvenile Mitral Stenosis [6,7].
Recurrence of RF is more common in these patients, given their age. The results of percutaneous transluminal mitral commissurotomy (PTMC) are similar to those in adults [8], though the incidence of restenosis may be higher, especially in those who have active disease at the time of the intervention [9]. Mitral valve surgery carries the risk of acute complications, and children and adolescents may require reoperation 10 to 15 years later.
Many articles in the past have defined Juvenile MS suggesting that the age of presentation of these individuals has been decreased with each passing year. This advancement in detection of these patients is attributable to improvement in the imaging techniques of echocardiography, improved knowledge of the clinician and intuition regarding this entity.
Our patient was aged only 3 years at the time of presentation with Juvenile Mitral Stenosis which is very unusual. The presentation of any patient at such a young age has been not previously documented in literature.
References
- Manjunath CN. Valvular heart disease. API Text book of medicine 9th edition.
- (2004) Rheumatic fever and rheumatic heart disease. World Health Organ Tech Rep Ser 923: 1-122.
- Shrivastava S, Tandon R (1991) Severity of rheumatic mitral stenosis in children. Int J Cardiol 30(2): 163-167.
- Roy SB, Bhatia ML, Lazaro EJ, Ramalingaswami V (1963) Juvenile mitral stenosis in India. Lancet 2(7319): 1193-1195.
- Wilkins GT, Weyman AE, Abascal VM, Block PC, Palacios I (1988) Percutaneous balloon dilatation of the mitral valve: An analysis of echocardiographic variables related to outcome and the mechanism of dilatation. Br Heart J 60(4): 299-308.
- Bahl VK, Chandra S, Kothari SS, Talwar KK, Sharma S, et al. (1994) Percutaneous transvenous mitral commissurotomy using Inoue catheter in juvenile rheumatic mitral stenosis. Cathet Cardiovasc Diagn Suppl 2: 82-86.
- Harikrishnan S, Nair K, THarakan JM, Titus T, Kumar VK, et al. (2006) Percutaneous transmitral commissurotomy in juvenile mitral stenosis- comparison of long term results of Inoue balloon technique and metallic commissurotomy. Catheter Cardiovasc Interv 67(3): 453-459.
- Kothari SS, Kamath P, Juneja R, Bahl VK, Airan B (1998) Percutaneous transvenous mitral commissurotomy using Inoue balloon in children less than 12 years. Cathet Cardiovasc Diagn 43(4): 408-411.
- Kothari SS, Ramakrishnan S, Juneja R, Yadav R (2006) Percutaneous transvenous mitral commissurotomy in patients with severe mitral stenosis and acute rheumatic fever. Pediatr Cardiol 27(3): 347-350.






























