Abstract
Background and Objective: The postpartum period is a time of high vulnerability to psychiatric disorders, with postpartum depression (PPD) being the most prevalent. This study aimed to investigate the association between mode of delivery (vaginal or cesarean), perceived psychological trauma during labor, and risk of developing PPD.
Methods: A total of 336 women were evaluated during antenatal care at Hospital das Clínicas of UFMG, and 224 were reassessed postpartum. Sociodemographic variables, depressive symptoms (via clinical assessment and Mini International Neuropsychiatric Interview Plus 5th edition – MINI-Plus 5.0), and pregnancy/delivery aspects were collected. Perceived psychological trauma during labor was assessed through a semi-structured questionnaire, considering subjective traumatic birth experience and DSM-5 Criterion A for PTSD.
Results: The incidence of PPD was 19.8% (95% CI: 14.5–25.1%). Psychological trauma during labor was reported by 21.6% of participants and was significantly associated with increased PPD risk (OR = 2.68, 95% CI: 1.23–5.87). Additional risk factors included lack of family support, high gestational risk, unplanned pregnancy, desire for abortion, history of PPD, and lifetime major depressive disorder (p < 0.05).
Conclusion: Psychological trauma during labor was significantly associated with PPD, while mode of delivery was not. These findings highlight the importance of addressing women’s subjective experiences of childbirth, beyond medical outcomes, in the prevention of PPD. Future studies with diverse populations and stronger control of confounding variables are needed to clarify the complex interplay between delivery characteristics, trauma perception, and maternal mental health.
Keywords: Postpartum depression; Trauma; Mode of delivery
Abbreviations:DSM-5: The Diagnostic and Statistical Manual of Mental Disorders; 5th edition MINI-Plus 5.0: Mini International Neuropsychiatric Interview Plus 5th edition; PPD: Postpartum depression; PTSD: Pos-traumatic stress disorder; UFMG: Federal University of Minas Gerais
Introduction
The postpartum period is a period of high vulnerability to the incidence of psychiatric disorders in a woman’s life, and the postpartum depression (PPD) is the most prevalent one. The Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5) [1] defines PPD as the occurrence of depressive symptoms within up to four weeks after labor. However, updated clinical studies suggest that symptoms may arise from pregnancy up to one year postpartum [2-4], aligning with the updated DSM-5 concept of “perinatal depression”. Symptoms of PPD include sleep disturbances, decreased libido, tearfulness, anxiety, irritability, mood lability, appetite changes, and even suicidal and infanticidal ideations [5]. PPD is a serious - yet often underdiagnosed - mental health condition associated with intense maternal suffering, depressive mood, cognitive and social impairment and negative effects on the mother-infant relationship and potentially leading to long-term psychiatric disorders in children [3,6,7]. PPD prevalence varies by geographical region and study methodology, with estimates suggesting it affects an average of 1 in every 5 to 7 women within the first year postpartum, corresponding to approximately 10% to 20% of mothers [8-10]. Suicidal ideation can be present in up to 50% of women diagnosed with PPD [11], and perinatal suicide is among the leading causes of maternal death.
The primary predictors of PPD are biopsychosocial and include a prior diagnosis of depression or perinatal anxiety, a family history of mood disorders, a troubled marital relationship, perinatal loss, preterm birth, gestational diabetes, unplanned pregnancy, unemployment, low socioeconomic status, domestic violence, sexual abuse, obstetric violence, medical negligence, and age under 25 years [12,13]. These predictors highlight the increased risk of PPD among women in situations of greater socioeconomic vulnerability with weakened support networks, who are exposed to high levels of daily stressors. Other less evident factors, however, seem to influence the onset of depressive symptoms during the postpartum period, such as the occurrence or perception of trauma during childbirth, the mode of delivery, and maternal frustrations related to preferences between vaginal and cesarean delivery [14]. Childbirth, while eagerly anticipated by many women, can be a highly stressful and, in some cases, traumatic experiences. When childbirth is perceived as traumatic, it may contribute to the onset of neuropsychiatric disorders, including mood disturbances and anxiety symptoms. Several factors surrounding childbirth can serve as relevant risk factors, including the woman’s fear of epidural anesthesia, traumatic vaginal delivery, and emergency cesarean sections, all of which have been associated with emotional destabilization during the perinatal period [15-17]. Current research indicates that medical interventions, obstetric complications, and emergency cesarean sections are strongly associated with the perception of a traumatic delivery. Pain during childbirth may also be linked to the development of PPD, given the well-established association between pain and depression [18,19].
It is estimated that 30% to 44% of women will experience a traumatic delivery [20], defined as an intense emotional response to the birth of a baby, with or without physical injuries, resulting in long-term psychological distress [21]. This concept is relatively new compared to definitions of traumatic events presented in previous editions of the DSM-5. Importantly, even deliveries that are considered medically normal-based on factors such as fetal position, maternal-fetal conditions, cervical dilation, and fetal heart rate may still be perceived as traumatic by the patient, often making its identification challenging due to its subjective nature. This study aims to contribute to the understanding of the association between delivery characteristics and PPD within a specific high-risk population, particularly focusing on the role of perceived psychological trauma, while acknowledging the existing literature on mode of delivery. The mode of delivery may also be linked to postpartum depressive symptoms, although scientific evidence remains controversial. While labor and postpartum pain related from vaginal delivery have been identified as risk factors for PPD [22], a stronger and more frequently documented association exists between cesarean deliveries - particularly emergency cesareans - and increased PPD risk [23]. The objective of this study is to investigate the association between the mode of delivery (vaginal or cesarean), psychological trauma during childbirth, and the risk of developing PPD. These factors remain relatively underexplored in the context of the studied population and methodological approach and may provide valuable insights into the development of postpartum depressive symptoms.
Methods and Materials
Sample and Study Design
This study is part of a large prospective cross-sectional research project conducted at the Federal University of Minas Gerais (UFMG) since January 2011, which remains ongoing. The participating women were recruited from the prenatal care unit of the Hospital das Clínicas (HC) at UFMG, located in Belo Horizonte, Minas Gerais, Brazil. The research comprises multiple stages, including structured interviews, clinical assessments during the prenatal and postpartum periods, and, in its latest phase since 2018, neuropsychological tests and neuroimaging examinations during the postpartum period. A total of 336 women were evaluated between January 2011 and November 2016. All participants provided informed consent and received detailed explanations regarding the study. There were no age restrictions for participation, but pregnant women without the cognitive capacity to read the questionnaires and understand the research project were excluded. The sample group for the present study consists of 224 women who completed both stages of the assessment (prenatal and postpartum). The study was approved by the local research ethics committee and was conducted in accordance with the Declaration of Helsinki [24].
Instruments
Structured interviews were conducted with eligible participants, incorporating questionnaires covering sociodemographic information and delivery details, such as maternal age, educational level, pregnancy planning, marital status, history of miscarriage, complications, perceived psychological trauma during labor and delivery mode. Clinical assessments were performed by trained psychiatrists using the translated version of the Mini International Neuropsychiatric Interview-Plus (MINI-Plus) 5.0 [25]. This tool has high validity and reliability and is composed of modules assessing various psychiatric disorders, being used both for screening these conditions and diagnosing PPD. The interviews were conducted at two time points: during the second trimester of pregnancy and postpartum.
The concept of “psychological trauma during labor” was assessed through a semi-structured questionnaire, which included a specific section where the mother rated her birth as a traumatic experience. Specifically, participants were asked, “Did you perceive your delivery as traumatic?” The criteria used to categorize an experience as “psychologically traumatic” involved a subjective report of distress meeting certain intensity/ duration thresholds, further substantiated by the presence of DSM-5 Criterion A and B for Post-Traumatic Stress Disorder (PTSD), as assessed during the postpartum administration of the Mini International Neuropsychiatric Interview (MINI-Plus 5.0). This approach allowed for the identification of participants who subjectively experienced their birth as traumatic, regardless of medical complications, and met preliminary screening criteria for a traumatic event. This comprehensive approach acknowledges the subjective nature of trauma perception while providing a consistent framework for its identification within this study.
Statistical Analysis
Descriptive statistics (mean, standard deviation, median, and quartiles) were initially calculated for continuous variables. For categorical variables, frequency and proportion were estimated. Crude and adjusted risk ratios with 95% confidence intervals were calculated. The Mann-Whitney and Fisher’s tests were used to assess the association between the analyzed variables. Statistical analyses were performed using Stata software (STATA Corporation, College Station, Texas), version 12.0. A p-value less than 0.05 was considered statistically significant. To control for potential confounding, a multivariate logistic regression model was employed. Variables included in the adjusted models were those that showed statistical significance in bivariate analysis (p < 0.25) or were considered clinically relevant based on existing literature. Specifically, potential confounders such as lack of family support, higher gestational risk, unplanned pregnancy, desire for abortion, history of PPD, and lifetime major depressive disorder were included in the adjusted models, as detailed in Table 2. However, due to the nature of the data collection, direct measures of obstetric violence were not explicitly included as an independent variable in the statistical model, though its implications are discussed. The presence of social support was assessed and included in the multivariate analysis to account for its known influence on PPD development. The final model aimed to isolate the independent effects of the mode of delivery and psychological trauma during labor on PPD, while accounting for a range of biopsychosocial factors.
Results
The study population consisted of a cohort of 336 pregnant women who were first interviewed during the second trimester of pregnancy. A total of 224 women (66.6%) participated in both evaluations, completing all forms and interviews, thus becoming eligible for this study. The participants had a mean age of 30 years, 23.2% required hospitalization after childbirth, 20.7% experienced breastfeeding difficulties, 27.1% reported a psychologically traumatic delivery, and 21.5% had complications during childbirth. More than half of the women (53.7%) reported depressive symptoms postpartum. According to the MINI-Plus 5.0 scores, 73.3% of women who underwent cesarean sections did not exhibit depressive symptoms, 8% showed few symptoms, 15.2% had moderate depression, and 2.8% were severely depressed. In contrast, 76% of women who had vaginal deliveries did not show depressive symptoms, 7.2% had few symptoms, 13% had moderate depression, and 3.6% were seriously depressed. Breastfeeding became a difficulty for 20.7% of the women assessed in the postpartum period.
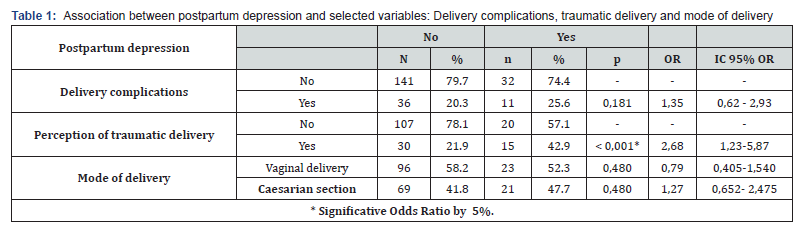
The (Table 1) demonstrates the association between postpartum depression and history of complications during delivery, a psychologically traumatic delivery, delivery mode preference and mode of delivery.
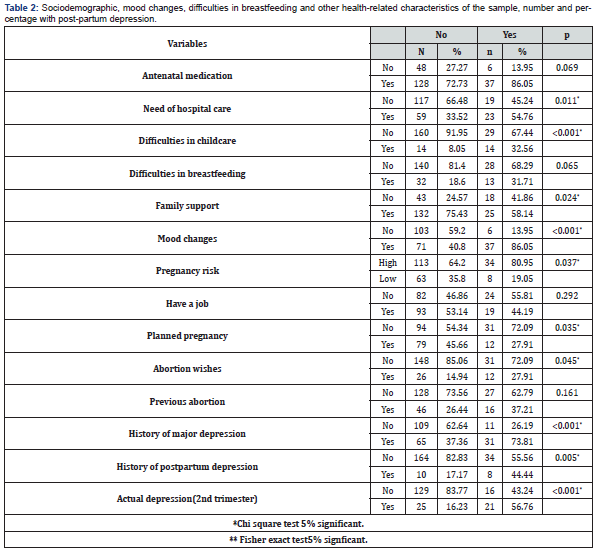
Women who reported a perceiving trauma during childbirth were 2.68 times more likely to develop postpartum depression compared to women who did not experience trauma (OR = 2.68, 95% CI= 1.23-5.87). The study identified a significant association between the occurrence of trauma during childbirth and postpartum depression. Additionally, lack of familial support, high gestational risk, unplanned pregnancy, desire for abortion, a history of postpartum depression, and a lifetime history of major depressive disorder (MDD) were also associated with current PPD (see Table 2).
Discussion
The prevalence of PPD identified in the present study was 19.8% (95% CI: 14.5% to 25.1%), a value consistent with the literature, which reports rates ranging from 10% to 20%. The high upper limit of the confidence interval can be attributed to the inclusion of many high-risk pregnant women, a group in which postpartum depression tends to be more prevalent. No significant differences were found linking the mode of delivery to an increased risk of postpartum depression in our specific cohort. On the other hand, previous studies have demonstrated a closer association between cesarean delivery and a heightened risk of PPD [26-28], particularly emergency cesarean sections. It is possible that cesarean section increases susceptibility to PPD due to its association with hemorrhage and infant mortality risk, as well as causing biological changes in the mother, such as decreased serum prolactin levels [29]. The apparent discrepancy between our findings and existing literature might be attributed to several factors. First, our study population primarily comprised women attending a university hospital prenatal clinic, which may introduce a specific profile of patients (e.g., higher-risk pregnancies, access to specialized care) that could influence outcomes differently from general populations. Second, our assessment of mode of delivery did not differentiate between elective and emergency cesarean sections, a distinction that has been shown to be critical in other studies for its association with PPD risk. It is possible that the traumatic nature associated with emergency interventions, rather than the mode of delivery itself, is the primary driver of PPD risk, as suggested by some authors. Our focus on perceived trauma during labor might have captured this underlying mechanism more directly, overshadowing an independent effect of the delivery mode. Furthermore, variations in study design, cultural context, and definitions of PPD or traumatic delivery across different studies could also contribute to these diverging results.
In the present study, 21.6% of participants reported experiencing trauma during childbirth, and these women were significantly more likely to be diagnosed with postpartum depression (OR = 2.68, 95% CI 1.23-5.87). Scientific evidence suggests a significant association between gestational depression and the occurrence of postpartum PTSD [30,31], indicating a bidirectional relationship between perinatal depression and PTSD throughout the perinatal period. Studies on the prevalence of PTSD in the perinatal period have found results ranging from 2.9% to 6% [32,33]. Thus, it is possible that a traumatic experience contributes to the emergence of depressive symptoms, such as low mood, reduced interest or pleasure in most activities (anhedonia), fatigue, difficulty concentrating, feelings of worthlessness or excessive guilt, and thoughts of death and suicidal ideation. PTSD symptoms have also been associated with emergency cesarean sections, reinforcing the traumatic nature of such interventions, although these findings were not confirmed in this study.
Despite not specifically addressed in this study, obstetric violence represents an important variable when analyzing the occurrence of traumatic childbirth. This form of violence can be verbal, physical, or psych affective and is considered a severe medical malpractice, leading to significant psychological suffering for the mother. A Brazilian study conducted in Pelotas found that women who suffered abuse and disrespect in healthcare institutions were more likely to develop PPD [34]. This mistreatment often involved violations of the pregnant woman’s autonomy, such as failure to respect the agreed-upon mode of delivery with the attending physician, and verbal obstetric violence [35]. The presence of support during pregnancy and the postpartum period is an important protective factor for PPD; therefore, it is crucial for healthcare professionals to provide the necessary support and care during this period. Finally, it is essential for healthcare professionals to conduct a thorough investigation into the patient’s experiences regarding childbirth to ensure proper care and monitoring of women in the postpartum period, particularly when there is suspicion of PPD or PTSD.
The limitations of this study include difficulties with participant adherence to postpartum assessments, with a total of 112 dropouts, representing 33.4% of the women initially recruited. This high dropout rate may introduce selection bias and could impact the internal validity of the findings, as women who dropped out might have differed systematically from those who completed the study, potentially affecting the observed prevalence and associations. Additionally, the inclusion of high highrisk pregnancies, which showed a prevalence of 64.2% for PPD and an overall mean age of 30 years, significantly limits the generalizability (external validity) of our findings to a broader population of pregnant and postpartum women. While providing valuable insights into this specific vulnerable group, the results may not be directly applicable to low-risk or general pregnant populations. Furthermore, the use of scales to assist in the diagnosis can be useful for screening depression, but it may overestimate postpartum depression rates with false-positive results [36]. Another limitation pertains to the definition and measurement of “psychological trauma” during delivery. While an attempt was made to capture subjective experience, the absence of a formally validated psychometric tool for this specific construct within the study design may affect the precision and comparability of this finding with other studies employing standardized trauma assessments. Finally, while several confounding variables were included in the statistical models, the direct and comprehensive assessment of obstetric violence as a distinct variable was not fully incorporated into the statistical analysis, representing a potential unmeasured confounder given its strong association with traumatic birth experiences.
Conclusion
This study investigated the relationship between childbirth characteristics, such as the mode of delivery and the perception of trauma, and the risk of postpartum depression (PPD). While the mode of delivery was not associated with PPD, in this specific high-risk sample, perceiving birth as traumatic was significantly linked to its development. Other factors associated with an increased risk of PPD identified in the study were gestational risk, unplanned pregnancy, desire for abortion, history of PPD, and lifetime major depressive disorder. These findings underscore the importance of a careful and supportive approach by healthcare professionals and obstetricians during the perinatal period. Given the potential psychological impact of childbirth, it is crucial to ensure appropriate care for postpartum woman by providing emotional support, respecting their autonomy in decision-making, and detecting early symptoms of PPD and PTSD.
Further investigations are necessary to enhance the understanding of the association between the mode of delivery and the development of postpartum depression, particularly in relation to persistent postpartum pain and the effectiveness of analgesic interventions. Future studies should also aim to employ standardized measures for psychological trauma during birth and incorporate comprehensive assessments of obstetric violence, while also recruiting more diverse populations to enhance external validity.
Acknowledgement
We would like to acknowledge all study participants for their voluntary participation in the study.
Funding
This study was partially funded by the National Council for Scientific and Technological Development (CNPq, 304457/2023- 0) and the Research Support Foundation of the State of Minas Gerais (FAPEMIG, APQ - 01600-18). This work was supported by an academic research grant from CNPq and FAPEMIG. The funding source had no role in the analysis, writing, conclusion, or review of the research.
References
- American Psychiatric Association(2013) Diagnostic and Statistical Manual of Mental American Psychiatric Association.
- Yu H, Shen Q, Bränn E, Yang Y, Oberg AS, et (2024) Perinatal Depression and Risk of Suicidal Behavior. JAMA Netw Open 7(1): e2350897.
- Sanni SO, Adeoye IA, Bella-Awusah TT, Bello OO(2024) Influence of postpartum depression on maternal-infant bonding and breastfeeding practices among mothers in Abeokuta, Ogun Discover Mental Health 4(1): 46.
- Lee MS, Lee JJ, Park S, Kim S, Lee H (2023) Is social support associated with postpartum depression, anxiety and perceived stress among Korean women within the first year postpartum? Journal of Psychosomatic Obstetrics & Gynecology 44(1): 2231629.
- Wang Z, Liu J, Shuai H, Cai Z, Fu X, et (2021) Mapping global prevalence of depression among postpartum women. Transl Psychiatry 11(1): 543.
- Egmose I, Tharner A, Liebenberg KB, Steenhoff T, Væver MS (2022) Long-term effects of maternal postpartum depression on mothers’ and fathers’ parenting Early Child Dev Care. 192(2): 220-32.
- Peñacoba Puente C, Suso-Ribera C, Blanco Rico S, Marín D, San Román Montero J, et al. (2021) Is the Association between Postpartum Depression and Early Maternal–Infant Relationships Contextually Determined by Avoidant Coping in the Mother? Int J Environ Res Public Health 18(2): 562.
- Bradshaw H, Riddle JN, Salimgaraev R, Zhaunova L, Payne JL (2022) Risk factors associated with postpartum depressive symptoms: A multinational J Affect Disord 301: 345-51.
- Fish-Williamson A, Hahn-Holbrook J (2023) Nutritional factors and cross-national postpartum depression prevalence: an updated meta-analysis and meta-regression of 412 studies from 46 countries. Front Psychiatry 14: 1193490.
- Sidebottom AC, Vacquier M, LaRusso E, Schulte AK, Nickel A (2023) Prenatal and postpartum depression diagnosis in a large health system: prevalence and Ann Med 55(2): 2281507.
- Chen C, Okubo R, Okawa S, Hagiwara K, Mizumoto T, et (2023) The prevalence and risk factors of suicidal ideation in women with and without postpartum depression. J Affect Disord 340: 427- 434.
- Silva RS, Junior RA, Sampaio VS, Rodrigues KO, Fronza M (2021) Postpartum depression: a case-control study. The Journal of Maternal-Fetal & Neonatal Medicine 34(17): 2801- 2806.
- Zhao X hu, Zhang Z hua (2020) Risk factors for postpartum depression: An evidence-based systematic review of systematic reviews and meta-analyses. Asian J Psychiatr 53: 102353.
- Beck-Hiestermann FML, Hartung LK, Richert N, Miethe S, Wiegand-Grefe S (2024) Are 6 more accurate than 4? The influence of different modes of delivery on postpartum depression and PTSD. BMC Pregnancy Childbirth 24(1): 118.
- Bay F, Sayiner FD (2021) Perception of traumatic childbirth of women and its relationship with postpartum depression. Women Health 61(5): 479-89.
- Mo J, Ning Z, Wang X, Lv F, Feng J, Pan L (2022) Association between perinatal pain and postpartum depression: A systematic review and meta-analysis. J Affect Disord 312: 92-9.
- Smithson S, Mirocha J, Horgan R, Graebe R, Massaro R, et al. (2022) Unplanned Cesarean delivery is associated with risk for postpartum depressive symptoms in the immediate postpartum period. The Journal of Maternal-Fetal & Neonatal Medicine 35(20): 3860-3866.
- Yao C, Zhang Y, Lu P, Xiao B, Sun P, et (2023) Exploring the bidirectional relationship between pain and mental disorders: a comprehensive Mendelian randomization study. J Headache Pain 24(1): 82.
- Fonseca-Rodrigues D, Rodrigues A, Martins T, Pinto J, Amorim D, et (2021) Correlation between pain severity and levels of anxiety and depression in osteoarthritis patients: a systematic review and meta-analysis. Rheumatology 61(1): 53-75.
- Hüner B, Friedl T, Schütze S, Polasik A, Janni W, et al. (2023) Post-traumatic stress syndromes following childbirth influenced by birth mode-is an emergency cesarean section worst? Arch Gynecol Obstet 309(6): 2439-2446.
- Greenfield M, Jomeen J, Glover L (2016) What is traumatic birth? A concept analysis and literature review. Br J Midwifery 24(4): 254- 67.
- Du W, Bo L, Xu Z, Liu Z (2022) Childbirth Pain, Labor Epidural Analgesia, and Postpartum Depression: Recent Evidence and Future J Pain Res 15: 3007-3015.
- Meky HK, Shaaban MM, Ahmed MR, Mohammed TY (2020) Prevalence of postpartum depression regarding mode of delivery: a cross-sectional The Journal of Maternal-Fetal & Neonatal Medicine 33(19): 3300–3307.
- World Medical Association (2013) World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA 310(20): 2191-2194.
- Amorim P (2000) Mini International Neuropsychiatric Interview (MINI): validação de entrevista breve para diagnóstico de transtornos mentais. Revista Brasileira de Psiquiatria 22(3): 106-15.
- Grisbrook MA, Dewey D, Cuthbert C, McDonald S, Ntanda H, et (2022) Associations among Caesarean Section Birth, Post-Traumatic Stress, and Postpartum Depression Symptoms. Int J Environ Res Public Health 19(8): 4900.
- Ilska M, Banaś E, Gregor K, Brandt-Salmeri A, Ilski A, et al. (2020) Vaginal delivery or caesarean section – Severity of early symptoms of postpartum depression and assessment of pain in Polish women in the early puerperium. Midwifery 87: 102731.
- Sun L, Wang S, Li XQ (2021) Association between mode of delivery and postpartum depression: A systematic review and network meta-analysis. Australian & New Zealand Journal of Psychiatry 55(6): 588-601.
- Rua MO, Soares GFG, Lima CS de A, Martins ER, Pereira LF, et al. (2021) Cesarean section and postpartum depression: a review of risk factors. Electronic Journal Scientific Collection 18: e5727.
- Ertan D, Hingray C, Burlacu E, Sterlé A, El-Hage Post-traumatic stress disorder following childbirth. BMC Psychiatry 2021 21(1): 155.
- Liu Y, Zhang L, Guo N, Jiang H (2021) Postpartum depression and postpartum post-traumatic stress disorder: prevalence and associated factors. BMC Psychiatry 21(1): 487.
- Steetskamp J, Treiber L, Roedel A, Thimmel V, Hasenburg A, et al. (2022) Post-traumatic stress disorder following childbirth: prevalence and associated factors-a prospective cohort Arch Gynecol Obstet 306(5): 1531-1537.
- Lai X, Chen J, Li H, Zhou L, Huang Q, et al. (2023) The incidence of post‐traumatic stress disorder following traumatic childbirth: A systematic review and meta‐analysis. International Journal of Gynecology & Obstetrics 162(1): 211-221.
- Silveira MF, Mesenburg MA, Bertoldi AD, De Mola CL, Bassani DG, et (2019) The association between disrespect and abuse of women during childbirth and postpartum depression: Findings from the 2015 Pelotas birth cohort study. J Affect Disord 256: 441-447.
- Martinez-Vázquez S, Hernández-Martínez A, Rodríguez-Almagro J, Delgado-Rodríguez M, Martínez-Galiano JM (2022) Relationship between perceived obstetric violence and the risk of postpartum depression: An observational study. Midwifery 108: 103297.
- Cantilino A, Zambaldi CF, Albuquerque TLC de, Paes JA, Montenegro ACP, (2010) Postpartum depression in Recife - Brazil: prevalence and association with bio-socio-demographic factors. J Bras Psiquiatr 59(1): 1-9.






























