Rethinking Common Misdiagnoses: A Case Report and Literature Review of Giant Leiomyoma with Myxoid Degeneration
Achmadi1*, Farizky Martriano Humardani2,3, Taufan Harijanto1 and Artika Uthari1
1Regional Hospital Ibnu Sina, Indonesia
2Faculty of Medicine, University of Surabaya, Indonesia
3Magister in Biomedical Science Program, Faculty of Medicine Universitas Brawijaya, Indonesia
Submission: November 07, 2023;Published: November 15, 2023
*Corresponding author: Achmadi, Regional Hospital Ibnu Sina, Indonesia
How to cite this article: Achmadi, Farizky Martriano H, Taufan H, Artika U. Rethinking Common Misdiagnoses: A Case Report and Literature Review of Giant Leiomyoma with Myxoid Degeneration. J Gynecol Women’s Health 2023: 26(3): 556186. DOI: 10.19080/JGWH.2023.26.556186
Introduction
Introduction: Myxoid degeneration in substantial leiomyomas is an atypical transformation that complicates differential diagnosis, often mimicking malignancies like choriocarcinoma, sarcomatous changes, or even non-malignant conditions such as hydatid cysts.
Case Illustration: We document a case involving a 40-year-old patient with an uncommonly large intramural leiomyoma, which exhibited myxoid degeneration. This condition was initially misidentified through imaging modalities and the misdiagnosis persisted even after surgical intervention.
Discussion: Our analysis, augmented by a comprehensive literature review, reveals that large tumorous masses frequently lead to diagnostic errors, primarily due to a common association with malignant pathologies and the inherent difficulty in their assessment. The incidence of myxoid degeneration within leiomyomas tends to be higher among individuals aged over 40, particularly within Black and Asian demographics.
Conclusion: The potential for misdiagnosis of leiomyomas, especially those with myxoid degeneration, necessitates heightened clinical suspicion, particularly in patients of Asian descent over 40 years of age, to ensure accurate diagnosis and appropriate management.
Keywords: Leiomyoma; Myxoid, Rare; Misdiagnosis
Introduction
Leiomyoma degenerations are categorized into several types, such as cystic, hemorrhagic, fatty, hyaline, and myxoid. Uterine leiomyomas predominantly occur as the most frequent tumors in the female reproductive system, often presenting without symptoms [1]. Uncommonly, substantial leiomyomas may undergo myxoid degeneration. This rarity can complicate diagnosis, making it challenging to distinguish between conditions such as choriocarcinoma, sarcomatous transformation, or even hydatid cysts [2].
Currently, there is no universal classification for the term “giant leiomyoma.” However, according to some studies, leiomyomas that exceed 10cm in diameter have been categorized as “giant” or “huge” [3-5]. In this report, a case of a giant leiomyoma with myxoid degeneration is presented, accompanied by a comprehensive literature review to enhance the depth of our discussion.
Case Illustration
Patient NH, a 40-year-old married woman with two children, was referred to the surgery department due to the presence of an abdominal mass that has been persisting for a year. The mass causes pain during physical activity. Upon physical examination, the mass was found to be solid and immobile. NH brought an abdominal ultrasound image from a previous healthcare provider (Figure 1a). The ultrasound revealed a significantly enlarged liver extending to the right pelvic cavity, and there was an irregular solid mass present in both the right and left lobes, raising suspicions of malignant lesions. The uterus was measured at an anteroposterior size of 22mm, with no visible signs of gestation, and the presence of a mass, suspect malignant tumor [6-8].
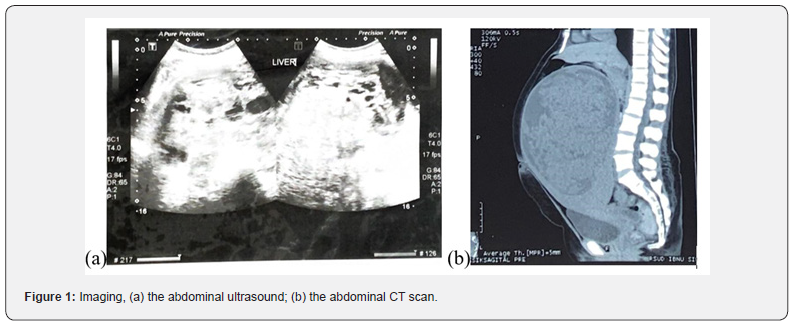
Based on the surgeon’s decision, an abdominal CT scan was performed on this patient (Figure 1b). Unexpectedly, the liver appeared normal. However, a cystic lesion with a solid component was identified, measuring 226.3 x 137.5 x 140mm for the solid part, and 257.5 x 159.6 x 140mm for the cystic part. Upon contrast enhancement, there was a vivid uptake in the solid lesion, while the cystic lesion did not exhibit noticeable contrast absorption, except for a rim of contrast enhancement. This lesion extends from the abdominal cavity down to the upper pelvic cavity, pushing the intestines peripherally and superiorly. the uterus, which could not be evaluated further, with conclusion malignant tumor from peritoneal.
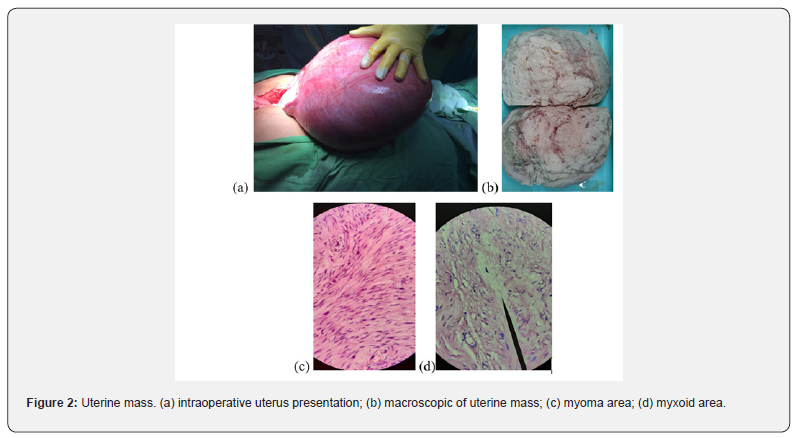
The surgeon, upon operating on the patient, unexpectedly encountered a substantial uterine mass (Figure 2a & 2b), with the myoma measuring 28 x 25 x 25cm. A consultation with a gynecologist was made intraoperatively. The gynecologist decided on a supracervical hysterectomy and bilateral salpingectomy, diagnosing the condition as a hydatidiform mole, with a differential diagnosis of uterine leiomyoma. Post-operatively, the patient’s β-HCG levels were checked, yielding normal results.
The uterine mass was analyzed by the pathologist. The findings included an atrophic endometrium and benign growth in the myometrium, which consisted of smooth muscle with spindle-shaped, monotonous cells with fine chromatin arranged in fascicles (Figure 2c). Additionally, some areas displayed characteristics consistent with myxoma (Figure 2d). No malignant cells were found in the examined tissue. The final diagnosis is intramural leiomyoma with myxoid degeneration.
Discussion
In this report, we present the case of a 40-year-old married woman with two children. Initial diagnostic modalities, including ultrasound and CT scan, led to a suspected diagnosis of a malignant tumor. Post-operative findings altered the diagnosis to a hydatidiform mole, with uterine leiomyoma as a differential diagnosis. Subsequent histopathological examination confirmed the presence of a giant intramural leiomyoma with myxoid degeneration, measuring 28 x 25 x 25cm.
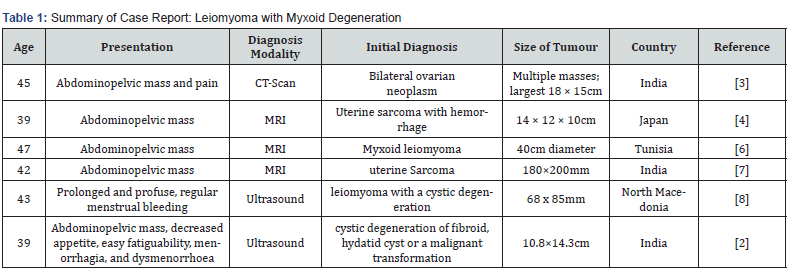
This misdiagnosis could likely be attributed to the massive size of the tumor, which is frequently associated with malignancy, and the rarity and complexity of the case, making evaluation challenging. As found in our literature review, an initial misdiagnosis was reported in four cases (Table 1). Surprisingly, misdiagnosis also occurred with the utilization of magnetic resonance imaging (MRI), while accurate diagnosis was achieved using ultrasound. This may be because smaller masses are easier to evaluate with ultrasound, and are often associated with benign conditions, leading to a correct and straightforward diagnosis.
The prensentation comes to seek medicine of leiomyoma with myxoid degeneration is same as usual leiomyoma such as including abnormal uterine bleeding and pelvic/abdominal pain and A pelvic mass [5]. The epidemiology of leiomyoma indicates that 30-40% of women older than 40 years are affected [9], which is consistent with our case report and literature review. Additionally, there is a higher prevalence among Black and Asian women compared to White women [10], further aligning with the observations made in our report and the accompanying literature review.
The clinical presentation of leiomyoma with myxoid degeneration typically aligns with the common manifestations of usual leiomyomas, which include symptoms such as abnormal uterine bleeding, pelvic/abdominal pain, and the discernment of a pelvic mass [5]. Epidemiological data underscores that leiomyomas affect about 30-40% of women aged over 40 years [9], a statistic that resonates with the observations articulated in our case report and substantiated through our literature review. Moreover, a discernible pattern of heightened prevalence has been noted among Black and Asian women in comparison to their White counterparts [10], further aligning with the observations made in our report and the accompanying literature review.
Conclusion
A rare giant intramural leiomyoma with myxoid degeneration, often misdiagnosis. The initial diagnostic imaging erroneously suspected a malignant tumor, and post-operatively, a hydatidiform mole was considered. The misdiagnosis likely stemmed from the massive size of the tumor and the inherent difficulties in diagnosing such extensive masses, which are often associated with malignancy. Due to often misdiagnosis leimyoma with myxoid degeneration must be considered when occurring in Asian, mass occur exceeding in 40 year.
References
- Dayal S, Kumar A, Verma A (2014) Clinicopathologic correlation of leiomyoma with clinical findings and secondary changes in a rural population of North India. Am J Clin Pathol 141(2): 275-279.
- Sugandha S, Mahajan G, Jindal M, Minhas S (2023) Uterine Fibroid and Extensive Myxoid Degeneration- Is it Benign or Malignant? J Clin Diagnostic Res 17(1): QD01 - QD03.
- Sharma R, Guleria K, Suneja A, Bhaskaran S, Tanveer N, et al. (2017) Giant leiomyoma with extensive myxoid degeneration in Mayer–Rokitansky–Küster–Hauser syndrome. Int J Gynecol Obstet 138(1): 125-127.
- Yamashiro T, Gibo M, Utsunomiya T, Murayama S (2007) Huge uterine leiomyoma with adenomyotic cysts mimicking uterine sarcoma on MR imaging. Radiat Med 25(3): 127-129.
- Moroni RM, Vieira CS, Ferriani RA, dos Reis RM, Nogueira AA, et al. (2015) Presentation and treatment of uterine leiomyoma in adolescence: a systematic review. BMC Womens Health 15(1): 4.
- Chaouki M, Marouen N, Najet BM, Zied K, Anis BA, et al. (2012) An unusual presentation of uterine leiomyoma: Myxoid leiomyoma. Int J Case Reports Images 3(3): 1-3.
- Panda A, Mahoorkar DN, Reddy N, Reddy BM (2022) Myxoid degeneration of leiomyoma-a masquerader. Int J Reprod Contraception, Obstet Gynecol 11(12): 3415.
- Samardjiski I, Petrushevska G, Simeonova-Krstevska S, Paneva I, Livrinova V, et al. (2021) Rare concomitant myxoid and cystic degeneration of uterine leiomyoma: Case report. Scr Med (Brno) 52(3): 235-238.
- Sparic R, Mirkovic L, Malvasi A, Tinelli A (2016) Epidemiology of Uterine Myomas: A Review. Int J Fertil Steril 9(4): 424-435.
- Murji A, Bedaiwy M, Singh SS, Bougie O (2020) Influence of Ethnicity on Clinical Presentation and Quality of Life in Women With Uterine Fibroids: Results From a Prospective Observational Registry. J Obstet Gynaecol Canada 42(6): 726-733.e1.






























