Sepsis and Pregnancy
Warren Carll1,2*, Richard W Carlson1,3,4, Anthony Vaccarello1,2 and Ashlye Carll5
1Department of medicine, Valleywise Medical Center, United States
2Creighton University School of Medicine, United States
3College of Medicine, University of Arizona, United States
4Mayo Clinic Alix School of Medicine, United States
5Phoenix Children’s Hospital, United States
Submission: August 18, 2022; Published: August 25, 2022
*Corresponding author: Warren Carll, Creighton University School of Medicine, Phoenix, AZ, United States
How to cite this article: Warren C, Richard W C, Anthony V, Ashlye C. Sepsis and Pregnancy. J Gynecol Women’s Health 2022: 23(5): 556125. DOI: 10.19080/JGWH.2022.23.556125
Abstract
Sepsis continues to be a leading cause of morbidity and mortality in pregnant patients. Despite advances in sepsis screening, diagnosis, and management, mortality has been increasing around the world. In this review, we discuss the advances in the screening, diagnosis, and management of sepsis in pregnant patients. We also discuss areas for potential improvement.
Keywords: Sepsis; Septic shock; Pregnancy; Sepsis management; Sepsis screening
Abbreviations: MAP: Mean Arterial Pressure; SIRS: Systemic Inflammatory Response Syndrome; SOFA: Sequential Organ Failure Assessment; ICU: Intensive Care Unit; ECMO: Extracorporeal Membranous Oxygenation; MEW: Maternal Early Warning
Introduction
In the most recent SEPSIS-3 criteria, sepsis was defined as a life-threatening organ dysfunction caused by a dysregulated host response to infection; and septic shock was defined as persistent hypotension and an elevated lactic acid >2mmol/L in the absence of hypovolemia and requiring vasopressors to maintain a mean arterial pressure (MAP) of >/= 65mmHg. Rather than utilizing the traditional systemic inflammatory response syndrome (SIRS) criteria, SEPSIS-3 focuses on the use of the quick Sequential Organ Failure Assessment (qSOFA) score outside of the intensive care unit (ICU), and the SOFA score for the ICU. The primary rationales for this paradigm shift are that these definitions are less ambiguous, easier to incorporate at the bedside, more rapid than waiting for laboratory studies, and can be assessed anywhere rapidly at the bedside, even without laboratory or imaging capabilities [1]. This is important, as sepsis remains a major cause of pregnancy-related morbidity and mortality. In fact, the incidence of sepsis in pregnancy has increased by 236% in the United States and remains the 3rd most common maternal cause of death in the peripartum period globally. This is thought to be due to barriers to care of the pregnant patient, along with failure to recognize sepsis in these patients [2].
Pathophysiology
Sepsis is a multifaceted host response to infection, with activation of both pro-, and anti-inflammatory pathways. Additionally, there is modification of many non-immune physiological pathways, including cardiovascular, endocrine, coagulation, hormonal, and autonomic; all of which have prognostic significance. In fact, mortality increases significantly with each system affected. This may result in increased risk of premature rupture of membranes, neurodevelopmental abnormalities, such as cerebral palsy, premature labor, stillbirth, and maternal mortality [3-6]. During pregnancy, there are multiple adaptations to the maternal immune system to prevent immune rejection of the developing fetus, which are beyond the scope of this article. These must be balanced to allow for adequate host response to infection [8]. Well-described risk factors for sepsis during pregnancy include invasive procedures, such as cervical cerclage and amniocentesis, cesarean delivery, mastitis, lack of prenatal care, immunosuppression, poverty, and obesity [8,9]. The most common sources of sepsis in this population include pyelonephritis and pneumonia, followed by chorioamnionitis/endometritis, gastrointestinal tract trauma or rupture, and retained products of conception [10].
Pathogens
The most commonly implicated pathogens in sepsis are bacterial. These include gram negative organisms, such as Escherichia coli, along with Streptococcus and Staphylococcus [11]. Although rare, group A Streptococcus may be an important cause of shock and death in the pregnant patient, with a reported mortality of 30-60% [12]. This is largely due to the organism’s ability to spread through tissue planes, resulting in necrotizing soft tissue infections. Additionally, exotoxin production may lead to toxic shock syndrome. Occasionally, Candida species can lead to sepsis, especially in the immunocompromised patient. Important viral causes of sepsis include Influenza A and B, and CoVID-19 [10,13]. Of particular interest is CoVID-19, as pregnant patients with CoVID-19 may be at a higher risk of more severe disease. Pregnancy-related complications of CoVID-19 include increased risk of preterm delivery and venous thromboembolism [13].
Screening and Diagnosis
Several warning signs of sepsis in pregnancy have been developed. According to Bauer et al., the Systemic Inflammatory Response Syndrome (SIRS) was the most sensitive and least specific, whereas the quick Sequential Organ Failure Assessment (qSOFA) was the most specific and least sensitive screening tool. Maternal early warning (MEW) was less sensitive that SIRS and less specific than qSOFA [14]. In Australia and New Zealand, omqSOFA has recently been adopted to help aid in the identification of sepsis in pregnant patients, as there are important physiologic changes during pregnancy. The most relevant physiological changes during pregnancy include increased minute ventilation and hypotension, particularly during the 3rd trimester due to the gravid uterus compromising venous return. It is unknown whether these criteria improve sensitivity and specificity of qSOFA in the pregnant patient [15]. (Table 1) compares and contrasts SIRS, qSOFA, MEW, and omqSOFA.
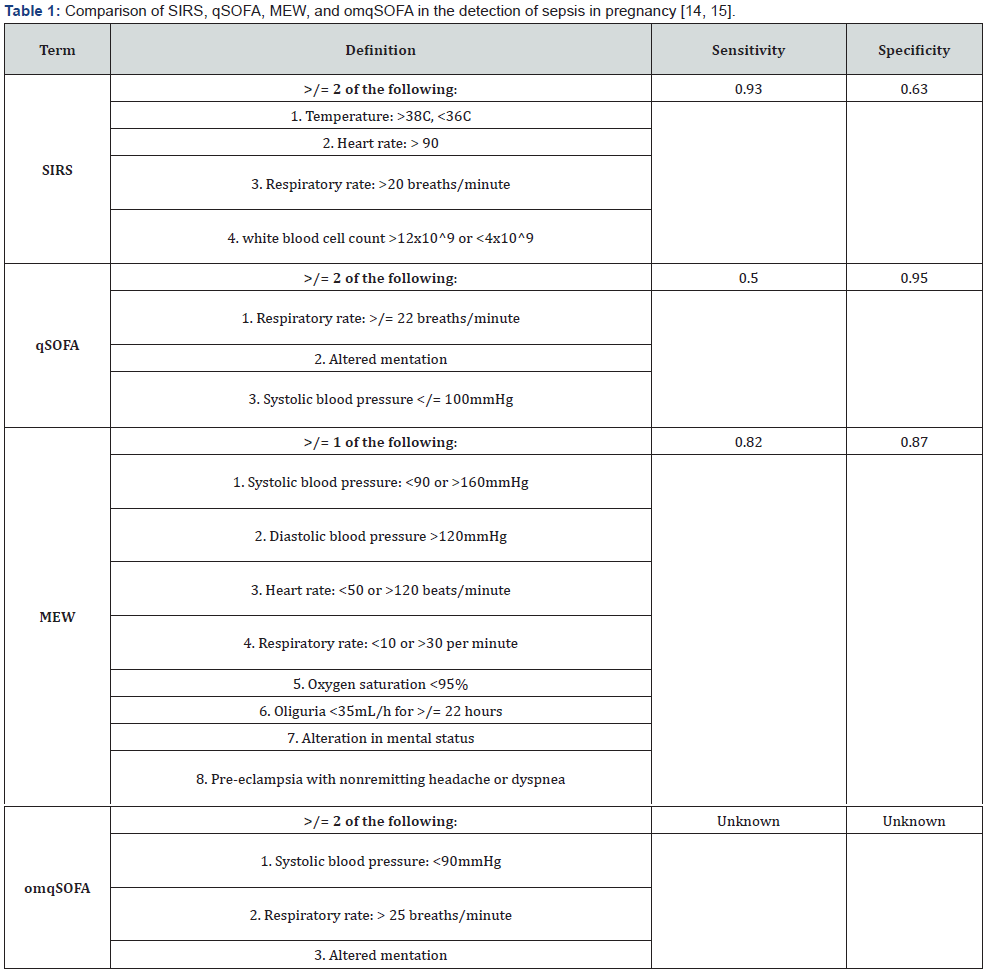
Table definitions: SIRS-Systemic Inflammatory Response Syndrome. qSOFA-quick Sequential Organ Failure Assessment. SOFA-Sequential Organ Failure Assessment. omqSOFA-Obstetrically-modified quick Sequential Organ Failure Assessment.
Management
There are no differences in the management of sepsis in pregnant patients in the Surviving Sepsis Campaign. These guidelines were updated in 2018 to reflect the “Hour-1 Surviving Sepsis Campaign Bundle of Care”. The first priority within the first hour of presentation to the emergency department, or earliest recognition of sepsis, is to administer empiric antimicrobials after obtaining blood cultures. The most common pathogens include Escherichia coli, Staphylococcus, Streptococcus, and other gramnegative infections [1]. Blood cultures should not delay empiric antimicrobial administration, as mortality increases 7.6% each hour [16].
Other priorities include obtaining an initial blood lactate, with repeat assessments if the initial value >/= 2mmol/L, along with rapidly administering 30ml/kg of intravenous fluids for patients who are hypotensive and/or have a lactic acid >/= 4mmol/L. If the mean arterial pressure (MAP) remains <65mmHg, vasopressor therapy should be initiated. Additionally, a site of infection requiring source control should be sought and definitively managed [17]. In the pregnant patient, this should include delivery of the fetus if the uterus is thought to be the source of infection [2]. If the patient fails to respond to the above measures, Extracorporeal Membranous Oxygenation (ECMO) may be considered, as maternal and fetal survival rates with implementation of ECMO are 80% and 70%, respectively [18]. Finally, corticosteroids should be administered for patients <34 weeks of gestation, together with electronic fetal monitoring [19].
Discussion
As discussed herein, sepsis continues to be a significant cause of morbidity and mortality in pregnancy. Risk factors for sepsis in pregnancy include invasive procedures, cesarean delivery, immunosuppression, lack of preterm care, obesity, and lower socioeconomic status. The most common sources of infection in pregnancy include pneumonia and pyelonephritis, followed by chorioamnionitis/endometritis, retained products of infection, and gastrointestinal pathology. The most common organisms include Escherichia coli and other gram-negative organisms, as well as Streptococcus and Staphylococcus. Empiric antimicrobials targeting these organisms should be administered within the first hour of recognition of sepsis, ideally after blood cultures have been obtained. A source of infection should be sought and aggressively managed.
In 2016, Chebbo et al. published a seminal review paper, which highlighted important topics regarding sepsis in pregnancy, including incidence and mortality, pathophysiology, current definitions, identification, prevention, sources of infection, and management of specific infections [20]. Since this paper was published, there have been additional changes in the understanding of sepsis in pregnancy, including definitions, scoring systems, and principles of management. There have also been advancements in the understanding of pathophysiology and risk factors of sepsis in the pregnant patient. The current emphasis is the use of empiric antimicrobials and aggressive management as soon as possible after the recognition of sepsis; ideally within the first hour. Despite these advances, rates of sepsis-related mortality have been increasing throughout the world. Future areas of improvement should therefore focus on barriers to care of the pregnant patient, along with early recognition.
Acknowledgements
Medical Intensive Care Unit staff of Valley wise Health Medical Center, April Aguinaga, MLS, AHIP. Valley wise Health Medical Center library.
References
- Singer M, Deutschman CS, Seymour CW, M Shankar-Hari, Djillali A, et al. (2016) The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA 315(8): 801-810.
- Fan S, Liu P, Yan S, Huang L, Liu X (2020) New concept and management for sepsis in pregnancy and the puerperium. Maternal-Fetal Medicine 2(4): 231-239.
- Ping L, F Shang-Rong, L Xiao-Ping, Z Di-Rong, Li Yun, et al. (2020) Puerperal sepsis caused by clostridium innocuum in a patient with placenta accreta and literature review. Maternal-Fetal Medicine 2(3): 181-188.
- Kim CJ, Romero R, Chaemsaithong P, Chaiyasit N, Yoon BH, et al. (2015) Acute chorioamnionitis and funisitis: Definition, pathologic features, and clinical significance. Am J Obstet Gynecol 213(4 Suppl): S29-52.
- Tann CJ, Nakakeeto M, Willey BA, Margaret S, Emily LW, et al. (2018) Perinatal risk factors for neonatal encephalopathy: An unmatched case-control study. Arch Dis Child Fetal Neonatal Ed 103(3): F250-F256.
- Helmo FR, Alves EAR, Moreira RAA, Viviane OS, Laura PR, et al. (2018) Intrauterine infection, immune system and premature birth. J Matern Fetal Neonatal Med 31(9): 1227-1233.
- Abu-Raya B, Michalski C, Sadarangani M, Lavoie PM (2020) Maternal immunological adaptation during normal pregnancy. Front Immunol 11: 575197.
- Burlinson CEG, Sirounis D, Walley KR, Chau A (2018) Sepsis in pregnancy and the puerperium. Int J Obstet Anesth 36: 96-107.
- Foeller ME, Gibbs RS (2019) Maternal sepsis: new concepts, new practices. Curr Opin Obstet Gynecol 31(2): 90-96.
- Martin S, McMurtry Baird S (2018) Sepsis and septic shock in pregnancy. Contemporary OB/GYN.
- Bauer ME, Bateman BT, Bauer ST, Shanks AM, Mhyre JM (2013) Maternal sepsis mortality and morbidity during hospitalization for delivery: Temporal trends and independent associations for severe sepsis. Anesth Analg 117(4): 944-950.
- Rottenstreich A, Benenson S, Levin G, Kleinstern G, Moses AE, et al. (2019) Risk factors, clinical course and outcomes of pregnancy-related group A streptococcal infections: Retrospective 13-year cohort study. Clin Microbiol Infect 25(2): 251.e1-251.e4.
- Wastnedge EAN, Reynolds RM, van Boeckel SR, Sarah JS, Fiona CD, et al. (2021) Pregnancy and COVID-19. Physiol Rev 101(1): 303-318.
- Bauer ME, Housey M, Bauer ST, Sydney B, Anthony C, et al. (2019) Risk factors, etiologies, and screening tools for sepsis in pregnant women: A multicenter case-control study. Anesth Analg 129(6): 1613-1620.
- Bowyer L, Robinson HL, Barrett H, Timothy MC, Michelle G, et al. (2017) SOMANZ guidelines for the investigation and management sepsis in pregnancy. Aust N Z J Obstet Gynaecol 57(5): 540-551.
- Kumar A, Roberts D, Wood KE, Bruce L, Joseph EP, et al. (2006) Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med 34(6): 1589-1596.
- Levy MM, Evans LE, Rhodes A (2018) The surviving sepsis campaign bundle: 2018 update. Crit Care Med 46(6): 925-928.
- Sharma NS, Wille KM, Bellot SC, Diaz-Guzman E (2015) Modern use of extracorporeal life support in pregnancy and postpartum. ASAIO J 61(1): 110-114.
- Plante LA, Pacheco LD, Louis JM (2019) SMFM consult series #47: Sepsis during pregnancy and the puerperium. Am J Obstet Gynecol 220(4): B2-B10.
- Chebbo A, Tan S, Kassis C, Tamura L, Carlson RW (2016) Maternal sepsis and septic shock. Crit Care Clin 32(1): 119-135.






























