Treatment With L-Methionine, Chondroitin Sulfate, Hyaluronic Acid and Lactobacillus Plantarum for Recurrent Cystitis
Luca Zurzolo1*, Giampaolo Mainini2, Mario Passaro3 and Giulio Toro1
1Studio Zurzolo, Napoli, Italy
2Menopausal Center, San Leonardo Hospital, Italy
3ASL NA3 SUD, Naples, Italy
Submission: July 19, 2022; Published: July 27, 2022
*Corresponding author: Luca Zurzolo, MD, Studio Zurzolo, Via tasso 480, 80127 Napoli, Italy
How to cite this article: L Zurzolo, G Mainini, M Passaro, G Toro. Treatment With L-Methionine, Chondroitin Sulfate, Hyaluronic Acid and Lactobacillus Plantarum for Recurrent Cystitis. J Gynecol Women’s Health 2022: 23(5): 556123. DOI: 10.19080/JGWH.2022.23.556123
Abstract
Background: The gold prophylactic therapy for recurrent cystitis is based on antibiotic therapy. Phenomena of antibiotic-resistance are reported with increasing frequency, hence the need to develop alternative treatments. The aim of the present study is to evaluate the efficacy and safety of Acidif® Pro, i.e., a food supplement containing L-methionine, chondroitin sulfate, hyaluronic acid and Lactobacillus plantarum, in reducing the symptoms and number of recurrences of urinary tract infections (UTIs) in women with recurrent cystitis.
Patients and Methods: 200 patients with reported episodes of recurrent cystitis were recruited and treated with Acidif® Pro, taken in the evening with an empty bladder, starting with 1 sachet per day for 1 month, followed by 1 sachet per day 7 days a month for 5 months. The trend of their symptoms was assessed by administering a five-question questionnaire during the first visit (T0) and upon completing the treatment protocol (T1).
Results: All patients tolerated the product well, with no reported phenomena of intolerance or allergic reactions associated with the Acidif® Pro. Overall, 85.5% of patients reported a noticeable improvement in symptoms after the treatment, 8.5% reported a slight improvement and 6% no improvement.
Conclusion: The results of this preliminary study seem to demonstrate the efficacy and safety of Acidif® Pro in treating symptomatic pain associated with recurrent cystitis and in reducing the number of episodes.
Keywords: L-methionine; Chondroitin sulfate; Hyaluronic acid; Lactobacillus plantarum; UTI
Abbreviations: UTIs: Urinary Tract Infections
Introduction
Cystitis is a widespread and disabling inflammation of the bladder generally associated with a bacterial infection, the incidence of which is higher among women, as epidemiological data show that 40-50% of female patients are affected by cystitis at least once in their lifetime [1]. Typical symptoms are urinary and suprapubic pain, burning, dysuria, pollakiuria and, in the most severe cases, haematuria. After the first event, 16-25% of patients experience a relapse within 6 months and 40-50% within the year. A minimum of three episodes per year or two in six months classify cystitis as recurrent [1-3]. Among the predominant etiopathological factors there are: genetic factors, use of diaphragm and spermicides, first occurrence of cystitis at an early age, sexual intercourse, reduced hygiene habits, reduced fluid intake and, in postmenopausal women, incontinence, bladder prolapse and post void residual [1,4].
Cystitis is caused by bacteria of enteric origin, mainly aerobic Gram negative [4], and therefore antibiotic therapy represents the gold standard of treatment. The choice of the most suitable antibiotic depends on the identification of the specific pathogen and on the patient’s medical history [5]. In the case of acute cystitis, therapy is limited to a single treatment cycle; while in case of relapses, prophylaxis calls for prolonged low-dose cycles [6]. However, phenomena of antibiotic-resistance are reported with increasing frequency, threatening public health to the point that the World Health Organization itself now recommends a controlled use of antibiotics, to be limited to cases of proven necessity only [7]. Hence the need to implement new treatment strategies to adopt for recurrent cystitis. There are various studies in the literature which document the use of alternative treatments such as oestrogenic substitutes, immunoactive prophylaxis, probiotics (of the genus Lactobacillus), American cranberry (Vaccinium macrocarpon) and intravesical instillations of hyaluronic acid and chondroitin sulfate [1,8,9]. Another available possibility is administering L-methionine, which is an essential amino acid that must be assimilated through the diet. The rationale for using L-methionine is due to its ability to lower the urinary pH, thus hindering bacterial adhesion [10,11]. Furthermore, in an acidic environment, the nitrites found in the urinary tract as products of bacterial metabolism can be converted into nitric oxide [12], whose in vitro activity has been shown to inhibit the growth of different bacteria, including Escherichia Coli, Pseudomonas aeruginosa and Staphylococcus saprophyticus [13]. The efficacy of a food supplement containing L-methionine, in association with extracts of Hibiscus sabdariffa L. and Boswellia serrata Rox., was tested in a group of 216 pregnant women suffering from symptomatic cystitis, and the results were compared with those of 48 women who underwent no treatment and only increased their daily fluid intake.
After the first week, the urine culture was negative in 70% of patients taking the supplement and only in 43.2% of patients in the control group [14]. Similarly positive results confirming the efficacy of L-methionine were obtained in patients suffering from uncomplicated urinary tract infections (UTIs), whose results after 7 days of treatment with a food supplement based on L-methionine, Hibiscus sabdariffa L. and Boswellia serrata Rox. were compared with those obtained in patients treated with fosfomycin for 2 days [15,16]. Hyaluronic acid is a ubiquitous extracellular matrix polysaccharide known for its multiple functions, including maintaining tissue homeostasis and protecting the cell surface, and its involvement in multiple physiological processes, including cell adhesion, migration, proliferation, embryogenesis, wound healing and regulation of immune response and inflammation [17].
Hyaluronic acid is often used in combination with glycosaminoglycans such as chondroitin sulfate-another key component of the extracellular matrix, capable of restoring the mucopolysaccharide film that covers the healthy urothelium and, thus, potentially preventing the recurrence of symptoms associated with cystitis. The use of intravesical instillations of hyaluronic acid in association with chondroitin sulfate as a prophylactic treatment for recurrent UTIs has led to encouraging results [1,18,19]. Two independent studies have evaluated the possibility of using a new formulation for oral use containing hyaluronic acid and chondroitin sulfate, in association with curcumin and quercetin [20,21]. The aim was to evaluate the effectiveness of a hyaluronic acid and chondroitin sulfate based product through a route of administration with greater compliance than the intravesical one. Both studies showed a significant improvement in symptoms, both in postmenopausal women [20] and in women of childbearing age [21].
One of the main natural defence mechanisms against UTIs is represented by the presence of commensal bacteria in the vaginal area and in the periurethral area, especially those belonging to the Lactobacillus genus. These are capable of binding to the cells of the vaginal epithelium, reducing the potential for adhesion, growth and colonization by uropathogenic bacteria [9,22]. A recent meta-analysis [6], including 6 randomised clinical trials and a total of 620 patients, examined the possibility of using these bacteria to treat UTIs, with its results supporting the effectiveness of the prophylactic action of Lactobacilli in recurrent UTIs [6]. The specific action of Lactobacilli is extensively analysed in the literature [23]. A study carried out in 2014, for example, investigated the effectiveness of slow-release vaginal tablets containing tara gum and two microorganisms, i.e., L. plantarum and L. fermentum.
The study involved 34 women with bacterial vaginosis, who used vaginal tablets for 4 weeks and were monitored for an additional month. The authors found that in most women treated with the tablets there was a significant reduction of the 3 bacterial strains responsible for the pathogenesis of vaginosis, bringing their levels below the threshold that would define the imbalance of the vaginal microbiota as pathological. The control group, on the other hand, showed no sign of improvement [24]. Based on this evidence, it was therefore hypothesised that L-methionine, chondroitin sulfate, hyaluronic acid and L. plantarum act in synergy when combined together in a single formulation, thus optimising the therapeutic efficacy of the product. The aim of the present study is therefore to evaluate whether a 6 month treatment based on L-methionine, chondroitin sulfate, hyaluronic acid and L. plantarum can alleviate the symptoms and reduce or eliminate the number of UTIs episodes in women with recurrent cystitis.
Materials and Methods
Patients
The present study examines 200 women, who were treated at Studio Zurzolo for episodes of recurrent cystitis in the period between June 2018 and June 2019. The local ethical committee approved the study. Inclusion criteria: women aged 18-50 who refer to our facility for treatment of recurrent cystitis, defined as two episodes in 6 months or three episodes in a year, with negative urine culture at the first enrolment visit. Exclusion criteria: current pregnancy, diagnosed interstitial cystitis/painful bladder syndrome, antibiotic treatment in the preceding two weeks. The study was conducted in compliance with the ethical principles of the Declaration of Helsinki and the women enrolled in the study signed a written informed consent.
Treatment protocol and parameters analysed
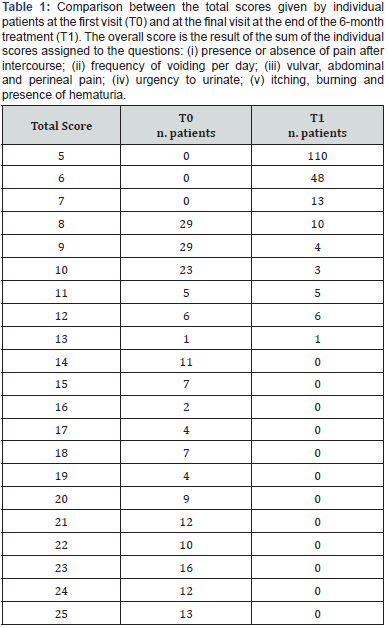
The patients were given a food supplement containing L-methionine, chondroitin sulfate, hyaluronic acid and L. plantarum (i.e., Acidif® Pro, Biohealth srl, Rivoli, Turin, Italy) with the following treatment protocol: 1 sachet per day for 30 days, followed by 1 sachet per day 7 days a month for 5 months, to be taken in the evening with an empty bladder. At the first visit (T0) after the anamnesis, the patients filled out a questionnaire consisting of five questions which were assigned a score from 1 to 5 (where 1 represents the minimum and 5 the maximum). The five questions formulated comply with the parameters evaluated in common clinical practice in the case of diagnosed cystitis, and respectively consider: (i) the presence or absence of pain after intercourse; (ii) the frequency of voiding per day; (iii) vulvar, abdominal and perineal pain; (iv) urgency to urinate; (v) itching, burning and the presence of hematuria. After the 6-month treatment (T1), patients were given the same evaluation questionnaire a second time and were also asked to report any adverse events that may have occurred during the treatment period. In the eventuality of an exacerbation during the six months of the study, the protocol required that patients be treated with conventional antibiotic therapy, but without discontinuing treatment with Acidif® Pro.
Statistical analysis
Mean and standard deviation were calculated for the questionnaire scores at T0 and T1. The scores at T0 and T1 were compared using a paired Student’s t-test. The significance level was set at 0.05. Statistical analysis was performed with Origin 9.0 (OriginLab Co, Northampton, Massachusetts, USA).
Result
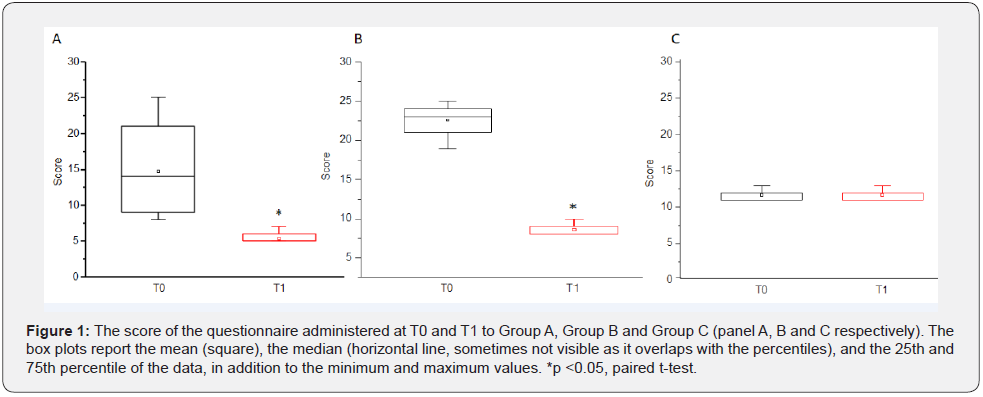
The study involved 200 women between 18 and 50 (mean age 45), who were treated with Acidif® Pro as prophylactic treatment for recurrent cystitis. Among these, 171 women (85.5%-Group A) reported no instances of exacerbation and, instead, a significant improvement in symptomatic pain compared to baseline; 17 women (8.5%-Group B) reported a moderate improvement in symptoms; and 12 women (6.0%-Group C) found no improvement. At T0, the mean total score obtained by questionnaire was 15.3±6.2. At T1, this value dropped to 6.1±1.8: a result that suggests a good overall efficacy of the therapy (p<0.05, coupled t-test). The mean total score of the patients in Group A, who reported a positive improvement in symptoms, decreased from 14.7±6.2 (T0) to 5.4±0.6 (T1), respectively (p<0.05, paired t-test) as shown in (Figure 1). The mean total score of the patients in Group B, who reported moderate symptoms improvement, decreased from 22.8±1.7 (T0) to 8.6±0.8 (T1), respectively (p<0.05, paired t-test) as shown in (Figure 1).
Finally, the mean total score of the patients in Group C remained unchanged over time (T0 = T1 = 11.6±0.7), indicating that in this subgroup of patients, treatment with Acidif® Pro lead neither to an improvement nor to a worsening of symptoms as shown in Figure 1. The parameter assessed by questionnaire which saw the greatest improvement between T1 and T0 was pain after intercourse; respectively followed by presence of itching and burning, urination frequency, vulvar pain, abdominal perineal and, finally, urgency to urinate. Table 1 reports the total score related to the symptoms suffered, as assigned by individual patients in the questionnaire at times T0 and T1. All patients tolerated the product well, none reported intolerances or allergic reactions related to its use.
Discussion
The symptoms that accompany recurrent cystitis have a significant impact on the patients’ quality of life [25]; thus, prophylactic treatments that reduce or eliminate the number of recurrences need to be available. In this study, treatment with a food supplement containing L-methionine, chondroitin sulfate, hyaluronic acid, and L. plantarum, maintained over a period of six months resulted in a reduction in symptoms related to recurrent cystitis from baseline in most patients (85.5%). It is interesting to note that the 12 women who saw no improvement were the same who on average had the lowest score at baseline, and thus had less severe symptoms from the start, compared to the other patients. Therefore, these results support the initial hypothesis that the combined use of these components may represent an effective form of treatment and a valid alternative to standard low-dose antibiotic prophylaxis. Prolonged use of antibiotic therapy leads to the development of resistant strains, which is a serious and widespread healthcare issue [7].
Many of the strains of E. Coli, Klebsiella and Enterobacteria, for example, are already resistant to third generation cephalosporins [26-28] and carbapenems [29,30]. The questionnaire administered to all participants at the start of the study and after 6 months of therapy allowed to evaluate post-treatment symptoms trend compared to baseline, highlighting an overall improvement in symptoms most associated with recurrent cystitis. Moreover, Acidif® Pro proved to be safe, as there were no reports of intolerance or allergic reactions related to the use of the product during the follow up period. A further advantage associated with the use of the product is that, in the event of an exacerbation of the symptoms, it can be used in conjunction with conventional antibiotic therapy without altering the properties of L. plantarum [31]. In fact, probiotic bacteria of the genus Lactobacillus are known to be intrinsically resistant to vancomycin and other antibiotics: meaning this resistance is not horizontally transmissible to pathogenic bacteria [32].
The results of this study are in line with those of other studies reported in the literature, which support the efficacy of L-methionine [14] and of the combined use of hyaluronic acid and chondroitin sulfate [20,21] in the treatment of symptomatic cystitis and in the prevention of recurrent UTIs. Further future investigations will be able to assess whether the use of Acidif® Pro is an adjuvant to the action of antibiotics in cases of documented bacterial cystitis, thus reducing the period of illness and symptoms severity. These results, although preliminary, are of fundamental importance, as they highlight relief in symptoms of recurrent cystitis without the need to resort to antibiotic prophylaxis. The main limitation of the present study consists in the lack of a control group; therefore, in order to confirm the preliminary results obtained during this study, further investigation will have to be carried out involving a greater number of subjects and possibly a control group to treat with an alternative therapy of known efficacy. In addition to this, the effectiveness of the product may be evaluated not only in the case of recurrent cystitis, but also in other UTIs.
Conclusion
Treating patients suffering from recurrent cystitis with a prophylactic treatment based on L-methionine, chondroitin sulfate, hyaluronic acid and L. plantarum over a period of six months is safe and effective to reduce symptoms of UTIs.
References
- Droupy S (2017) The therapeutic approach to different forms of cystitis: impact on public health. Urologia 84(Suppl-1): 8-15.
- Foxman B (2002) Epidemiology of urinary tract infections: incidence, morbidity, and economic costs. Am J Med 113(Suppl 1A): 5S-13S.
- (2013) Prevention of recurrent urinary tract infections in women. Drug Ther Bull 51(6): 69‐72.
- Sen A (2008) Recurrent cystitis in non-pregnant women. BMJ Clin Evid 2008: 0801.
- Kolman KB (2019) Cystitis and Pyelonephritis: Diagnosis, Treatment, and Prevention. Prim Care 46(2): 191-202.
- Ng QX, Peters C, Venkatanarayanan N, Goh YY, Ho CYX, et al. (2018) Use of Lactobacillus spp. to prevent recurrent urinary tract infections in females. Med Hypotheses 114: 49-54.
- WHO: Antimicrobial resistance [Internet]. Geneva: World Health Organization.
- Caretto M, Giannini A, Russo E, Simoncini T (2017) Preventing urinary tract infections after menopause without antibiotics. Maturitas 99: 43-46.
- Sihra N, Goodman A, Zakri R, Sahai A, Malde S (2018) Nonantibiotic prevention and management of recurrent urinary tract infection. Nat Rev Urol 15(12): 750-776.
- Fünfstuck R, Straube E, Schildbach O, Tietz U (1997) Prevention of reinfection by L-methionine in patients with recurrent urinary tract infection. Med Klin (Munich) 92(10): 574-581.
- Pagonas N, Horstrup J, Schmidt D, Benz P, Schindler R, et al. (2012) Prophylaxis of recurrent urinary tract infection after renal transplantation by cranberry juice and L-methionine. Transplant Proc 44(10): 3017-3021.
- Lundberg JO, Weitzberg E, Gladwin MT (2008) The nitrate-nitrite-nitric oxide pathway in physiology and therapeutics. Nat Rev Drug Discov 7(2): 156‐167.
- Carlsson S, Wiklund NP, Engstrand L, Weitzberg E, Lundberg JO (2001) Effects of pH, nitrite, and ascorbic acid on nonenzymatic nitric oxide generation and bacterial growth in urine. Nitric Oxide 5(6): 580-586.
- Passaro M, Mainini G, Ambrosio F, Sgambato R, Balbi G (2017) Effect of a Food Supplement Containing L-Methionine on Urinary Tract Infections in Pregnancy: A Prospective, Multicenter Observational Study. J Altern Complement Med 23(6): 471-478.
- Barletta C, Paccone M, Uccello N, Scaldarella LO, Romano C, et al. (2020) Efficacy of food supplement Acidif plus® in the treatment of uncomplicated UTIs in women: a pilot observational study. Minerva Ginecol 72(2) : 70-74.
- Cai T, Cocci A, Tiscione D, Puglisi M, Di Maida F, et al. (2018) L-Methionine associated with Hibiscus sabdariffa and Boswellia serrata extracts are not inferior to antibiotic treatment for symptoms relief in patients affected by recurrent uncomplicated urinary tract infections: Focus on antibiotic-sparing approach. Arch Ital Urol Androl 90(2): 97-100.
- Becker LC, Bergfeld WF, Belsito DV, Klaassen CD, Marks JG Jr, et al. (2009) Final report of the safety assessment of hyaluronic acid, potassium hyaluronate, and sodium hyaluronate. Int J Toxicol 28(Suppl 4):5-67.
- Goddard JC, Janssen DAW (2018) Intravesical hyaluronic acid and chondroitin sulfate for recurrent urinary tract infections: systematic review and meta-analysis. Int Urogynecol J 29(7): 933-942.
- Cicione A, Cantiello F, Ucciero G, Salonia A, Madeo I, et al. (2014) Restoring the glycosaminoglycans layer in recurrent cystitis: experimental and clinical foundations. Int J Urol 21(8): 763-768.
- Torella M, Del Deo F, Grimaldi A, Iervolino SA, Pezzella M, et al. (2016) Efficacy of an orally administered combination of hyaluronic acid, chondroitin sulfate, curcumin and quercetin for the prevention of recurrent urinary tract infections in postmenopausal women. Eur J Obstet Gynecol Reprod Biol 207: 125-128.
- Schiavi MC, Porpora MG, Vena F, Prata G, Sciuga V, et al. (2019) Orally Administered Combination of Hyaluronic Acid, Chondroitin Sulfate,Curcumin, and Quercetin in the Prevention of Postcoital Recurrent Urinary Tract Infections: Analysis of 98 Women in Reproductive Age After 6 Months of Treatment. Female Pelvic Med Reconstr Surg 25(4): 309-312.
- Costantini E, Giannitsas K, Illiano E (2017) The role of nonantibiotic treatment of community-acquired urinary tract infections. Curr Opin Urol 27(2): 120-126.
- Abad CL, Safdar N (2009) The role of lactobacillus probiotics in the treatment or prevention of urogenital infections--a systematic review. J Chemother 21(3): 243-252.
- Vicariotto F (2014) Effectiveness of an association of a cranberry dry extract, D-mannose, and the two microorganisms Lactobacillus plantarum LP01 and Lactobacillus paracasei LPC09 in women affected by cystitis: a pilot study. J Clin Gastroenterol 48(Suppl 1): S96-S101.
- Renard J, Ballarini S, Mascarenhas T, Zahran M, Quimper E, et al. (2014) Recurrent Lower Urinary Tract Infections Have a Detrimental Effect on Patient Quality of Life: a Prospective, Observational Study. Infect Dis Ther 4(1): 125-135.
- Sabharwal ER (2012) Antibiotic susceptibility patterns of uropathogens in obstetric patients. N Am J Med Sci 4(7): 316-319.
- McIsaac W, Carroll JC, Biringer A, Bernstein P, Lyons E, et al. (2005) Screening for asymptomatic bacteriuria in pregnancy. J Obstet Gynaecol Can 27(1): 20-24.
- Rizvi M, Khan F, Shukla I, Malik A, Shaheen (2011) Rising prevalence of antimicrobial resistance in urinary tract infections during pregnancy: necessity for exploring newer treatment options. J Lab Physicians 3(2): 98-103.
- Carlet J, Jarlier V, Harbarth S, Voss A, Goossens H, et al. (2012) Ready for a world without antibiotics? The Pensières Antibiotic Resistance Call to Action. Antimicrob Resist Infect Control 1(1): 11.
- Zowawi HM, Harris PN, Roberts MJ, Tambyah PA, Schembri MA, et al. (2015) The emerging threat of multidrug-resistant Gram-negative bacteria in urology. Nat Rev Urol 12(10): 570-584.
- Probion: Technical Memorandum Lactobacillus plantarum Lp-115. Halmstad: Probion.
- Gueimonde M, Sanchez B, G de L Reyes-Gavilan C, Margolles A (2013) Antibiotic resistance in probiotic bacteria. Front Microbiol 4: 202.






























