Maternal Near-Miss and Maternal Death Associated with Abdominal Ectopic Pregnancy: Case Series from a Tertiary Hospital in Southern Ethiopia
Shimelis Fantu Gebresilasie1 and Wondimagegnehu Sisay Woldeyes1,2
1MD, Gynecologic oncologist, Assistant Professor of Obstetrics and Gynecology, Hawassa University, Collage of Medicine and Health sciences, Ethiopia
2Chief Obstetrician and Gynecologist, Tercha General Hospital and Urogynecology and pelvic reconstructive surgery fellow at Jima University, Ethiopia
Submission: December 21, 2021; Published: January 10, 2022
*Corresponding author: Wondimagegnehu Sisay Woldeyes, MD, Gynecologic oncologist, Assistant Professor of Obstetrics and Gynecology; Hawassa University, Collage of Medicine and Health sciences / Chief Obstetrician and Gynecologist, Tercha General Hospital and Urogynecology and pelvic reconstructive surgery fellow at Jima University, Ethiopia.
How to cite this article: Shimelis F G, Wondimagegnehu SW. Maternal Near-Miss and Maternal Death Associated with Abdominal Ectopic Pregnancy: Case Series from a Tertiary Hospital in Southern Ethiopia. J Gynecol Women’s Health 2022: 22(5): 556100. DOI: 10.19080/JGWH.2022.22.556100
Abstract
An abdominal pregnancy is a rare form of pregnancy, and frequently missed during antenatal care. It almost always results in maternal near-miss or maternal death. A high index of suspicion may help to diagnose the condition early, but majority of these cases are diagnosed at advanced gestation when nonsurgical interventions are impossible and surgical interventions are difficult. Therefore, it is associated with high risk of maternal and foetal morbidity and mortality. In this case serious we report three cases of abdominal pregnancies, all were diagnosed before surgery, but the procedures were catastrophic with massive intra-abdominal bleeding in which two of our cases survived after massive transfusion and become maternal near misses whereas a third case died from severe intra-abdominal sepsis.
Keywords: Broad ligament pregnancy; abdominal pregnancy; maternal near-miss; Ethiopia; Hawassa
Abbreviations: MRI: Magnetic resonance imaging
Introduction
A woman who nearly died, but survived a complication that occurred during pregnancy, childbirth, or within 42 days of termination of pregnancy is called a maternal near-miss case. If these women die of those complications, they become maternal death cases. With abdominal pregnancy 1in 5 of them result in maternal death and almost all the remaining become maternal near-miss cases. In United States, for example, maternal death due to abdominal pregnancy estimated to be seven times higher than the estimated rate for ectopic pregnancy and ninety times the death related to normal delivery [1,2]. It is also associated with early fetal loss, malformation, and perinatal death of 40-95 % [3-5].
Abdominal pregnancy is an extremely rare form of ectopic pregnancy where implantation occurs within the peritoneal cavity outside the fallopian tubes and the ovaries [1,2]. It accounts 1-1.4 % of ectopic pregnancies, with an incidence of one in 2200-30,000 pregnancies [3-5]. Possible mechanisms for occurrence of abdominal pregnancy include: a secondary implantation from an aborted tubal pregnancy, the result of intra-abdominal fertilization of sperm and ovum, with primary implantation in the abdomen or rarely an iatrogenic mechanism after in vitro fertilization (IVF) resulting from uterine perforation by the IVF transfer catheter [2,3,5].
An abdominal pregnancy may get implanted anywhere in the abdomen including the omentum, pelvic sidewall, broad ligament, posterior cul-de-sac, abdominal organs (e.g., spleen, bowel, liver), large pelvic vessels, diaphragm, and the uterine serosa [2,4]. Unlike tubal pregnancy, these pregnancies may go to advanced gestational age and their presentation is also variable depending on the site of attachment. Acute abdomen and shock due to severe intra-abdominal hemorrhage from placental separation or rupture of maternal blood vessels or viscera may be first presentation in some cases. In others, on the other hand, it may be diagnosed in third trimester for the first time after failed induction or may even go to term undiagnosed [5-9]. When there is suspicion of abdominal pregnancy, different clinical and imaging criterion can be employed to assist in its diagnosis.
After diagnosis of abdominal pregnancy, the main stay of management is surgical (laparoscopy for early gestation and laparotomy for advanced pregnancy) [17,18]. In general delivery of the fetus may not be difficult, but the key issue is management of the placenta. Removal of the placenta (with risk of bleeding) and ligating the umbilical cord and leaving the placenta in situ with or without arterial embolization and/or methotrexate use are mentioned as options of dealing with the placenta. With either option there is high likely hood of severe maternal morbidity and mortality. Hemorrhage requiring transfusion is reported in 9/10 women and maternal death in as many as 20% of cases [5,6].
Sometimes medical treatment could be considered as an option when diagnosed in early gestational age, and conservatively managed for advanced but previable pregnancy till fetal maturity with great precaution and proper patient counseling [2,15,16].
In this case series we presented summery of clinical presentation, management, and foeto-maternal outcome of three cases of abdominal pregnancy managed in our hospital. Two of the cases presented in second trimester and a third case in third trimester. All the cases were managed surgically and required multiple transfusions. In the first case placenta is removed and bleeding was managed by abdominal packing whereas in the second case placenta removed easily by ligating the vessels. For the third case placenta was left behind but letter complicated by intrabdominal sepsis which required relaparotomy. The first two cases have survived this life-threatening condition, whereas the third case has complicated with maternal death.
Case presentation
Case-1
S.B. is a 26 years old gravid-5, para-4 mother presented to our hospital with complaint of lower abdominal pain at 5 months of amenorrhea. The pain started for 10 days before her visit to our hospital and worsening since two days with associated low grade fever. She has no history of antenatal care visits. The patient had no vaginal bleeding or discharge. She is married, mother of four and has no known medical problem.
On physical examination, her blood pressure was 90/60mmHg, pulse rate was 124, temperature was 38 OC, and respiratory rate was 28 breaths per minute. She had slightly dry mucosa with pink conjunctiva. On abdominal examination 20 weeks sized abdominopelvic mass, with guarding and tenderness. Otherwise, she had no sign of fluid collection. Upon pelvic examination, bulged posterior vaginal fornix which is soft, and tender was noted. The cervical-os pushed far anterior behind pubic bone and couldn’t be felt properly. No blood on examine finger.
On ultrasound examination, the uterus was enlarged with empty endometrial cavity. Well-formed foetus with positive heartbeat seen to the right posterolateral to the uterus. Gestational age from femur length was 19 weeks. There is no visible aminiotic fluid around the foetus but echo complex mass with cystic components seen behind the uterus. There was no free fluid collection. Her hematocrit was 32 percent and blood group was B+.
With impression of second trimester abdominal pregnancy, senior oncologist (for possible difficult dissection) was consulted, and laparotomy was decided (MRI is planned but the patient could not afford.)
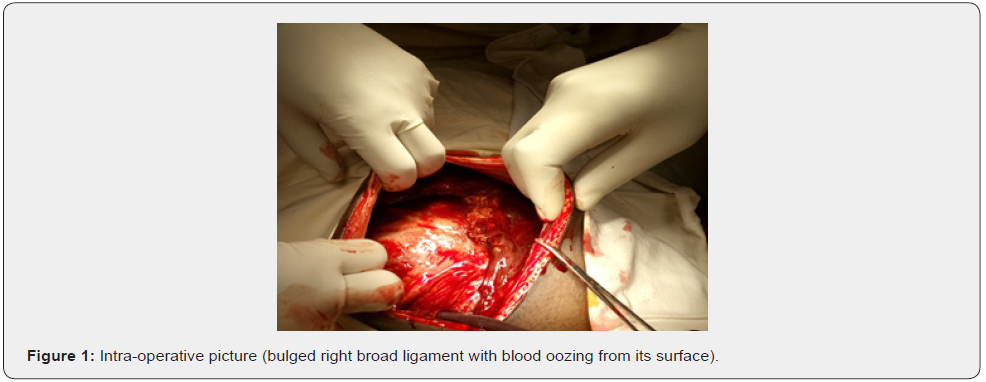
Upon laparotomy with midline vertical sub-umbilical incision, there was dark blood of around 300ml with bulged right broad ligament with oozing of blood from its surface (Figure 1). The uterus was slightly enlarged; otherwise, there is no overt defect on its wall. Right broad ligament entered through small incision on its anterior leaf. After blunt dissection 300gm, well-formed alive abortus extracted, which was buried deep into the recto vaginal septum (Figure 2).

The dissection has traumatized the placenta with massive bleeding. Due to this, placenta has to be dissected off and removed. To achieve this, right utero-ovarian pedicle ligated and separated while right ureter identified, sigmoid colon dissected off the mass attachment and the appendix too.
Continued bleeding couldn’t be controlled with application of multiple figure of eight stitches. An attempt to ligate the internal iliac artery was not successful due to distorted anatomy of the tissues to its vicinity which also bleeds on attempted manipulation. The patient’s blood pressure starts to drop, two unit of whole blood administered during surgery. Finally, the bleeding site is tightly packed with two gauze packs observed for some time. After confirming no ongoing bleeding, it was decided to leave the pack in place for 24 hours. After placing tube drain in the area of bleeding, abdomen was closed.
On immediate postoperative period, the patient was closely monitored for vital sign derangement, drainage output and urine output. She was put on ceftriaxone and metronidazole with regular analgesia. Twenty-four hours later, the patient had stable vitals, except for tachycardia; the abdominal drainage also had 200ml of haemorrhagic peritoneal fluid. On the first postoperative day (24 hours later), patient underwent repeat surgery to remove the pack. Under general anaesthesia, abdomen entered via previous incision, there was no fluid collection in the peritoneal cavity and both packs removed without difficulty. There was no bleeding after removal of the packs and abdomen closed with the drain kept in-situ.
The antibiotics continued, there was continued output via the drainage tube, until third day a total of 800ml of blood-tinged fluid collected. The patient was transfused with a total of five unit of whole blood in postoperative period. On fourth and fifth postoperative days the drain output starts to decrease and was removed subsequently. The patient was discharged improved on ninth postoperative day with therapeutic iron tablets in good condition with follow up appointment and contraception.
Case-2
RB is a 25 years old Gravid-1 mother presented with abdominal pain of 3 days duration at four months of missed period. She had associated nausea and intermittent vomiting of ingested matter since the early days of the pregnancy and worsened for the last three days. She also complains easy fatigability and dizziness but no syncope attack. The patient was married for the last twelve years and had difficulty of conceiving but did not have proper evaluation or treatment for this. Otherwise, she had no vaginal bleeding or discharge. The patient has no known medical problem diagnosed before this presentation.
On physical examination: She was acutely sick looking during her presentation to the hospital. The blood pressure was 100/70mmHg, and her pulse rate was 120 beats/min with respiratory rate of 24 breaths/min and was afebrile. She had pale conjunctiva and nonicteric sclera. On abdomen, diffusely distended abdomen with flank fullness, and shifting dullness. She also has 18 weeks sized ill-defined tender abdominopelvic mass. On digital pelvic examination, closed cervix with cervical motion tenderness and bulged posterior vaginal fornix, tender on attempted bimanual examination.
Her trans abdominal ultrasound scanning show enlarged uterus with empty endometrial cavity, placenta and fetus seen outside endometrial cavity anterior to the uterus, with BPD= 16 weeks and positive cardiac activity. There was also free peritoneal fluid in the posterior cul-de-sac and both paracolic gutters.
Her hematocrit was 22 percent with blood group of A+. With the diagnosis of ruptured 2nd trimester abdominal pregnancy emergency laparotomy decided.
Abdomen entered through mid-line vertical incision. There was 1500 ml of hemoperitoneum. The placenta was implanted to the great omentum, and serosa of the small bowel & sigmoid colon. The placental attachments were clumped, ligated; and the fetus (250 gm) and placenta extracted together (Figure 3). Removal was not difficult. The left ovary and tube were visualized and look normal. The right side of the uterus feel intact, right tube and ovary were normal. It was difficult to visualize the whole uterus due to extensive adhesions. After surgery the patient was transfused with two unit of whole blood and discharged on her sixth postoperative day in stable condition.

Case-3
RB is a 35 years old Gravid-1 mother with seven months amenorrhea and presented with abdominal pain of 6 months which has worsened since a week. She had antenatal care visits at a nearby health center with vaccination and blood tests but had no ultrasound examination. The patient was married for the last 10 years and had difficulty of conceiving. She did not have proper evaluation or treatment for that. Otherwise, she had no vaginal bleeding, nausea or vomiting. The patient has no known medical problem diagnosed before this presentation nor does history of pelvic surgery or diagnosed tuberculosis.
On physical examination the patient had stable vital signs with no remarkable findings except on the abdomen. On abdominal examination; slightly tender abdomen with irregular ‘’foetal parts’’ palpable over the lower abdomen with no sign of fluid collection. On ultrasound of the abdomen, uterus was slightly enlarged and empty. An alive feotus with gestational age of 30 weeks and positive heartbeat was seen outside the uterus and no measurable amniotic fluid around it. The placenta is seen behind the fetus and the uterus with difficulty to delineate it totally. Pelvic MRI revealed the placenta is attached to posterior pelvic wall with extension to posterior cul-de-sac and posterior uterine wall. Her hematocrit was 36 perecent.
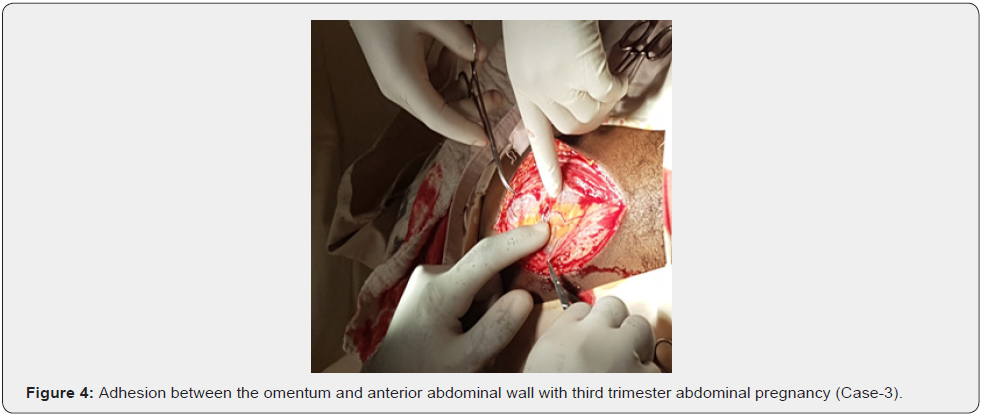
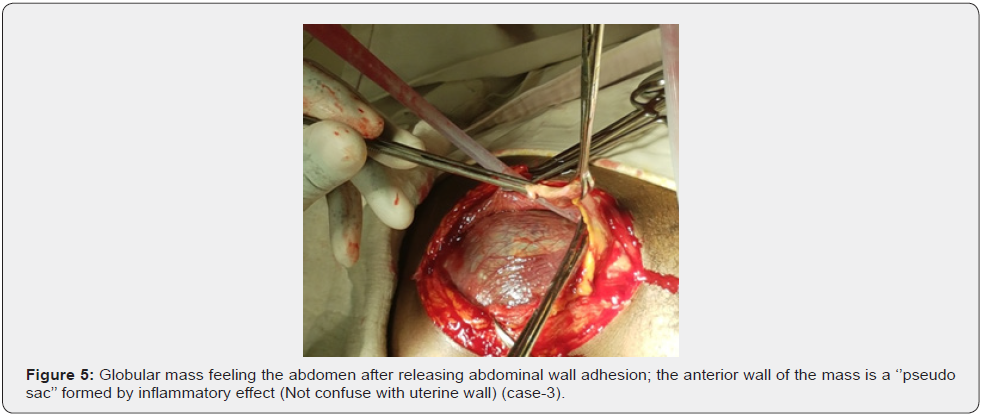
After preparing 4 units of cross matched blood and appropriate counseling laparotomy was decided with involvement of gynecologic oncologist. Under general anesthesia, abdomen was entered via midline incision which extended above the umbilicus. Upon entry, there was dense adhesion between the indurated omentum and anterior abdominal wall with inflammatory nodules all over it (Figure 4). After careful dissection of this adhesion, we found globular mass filling the whole lower abdomen (Figure 5).
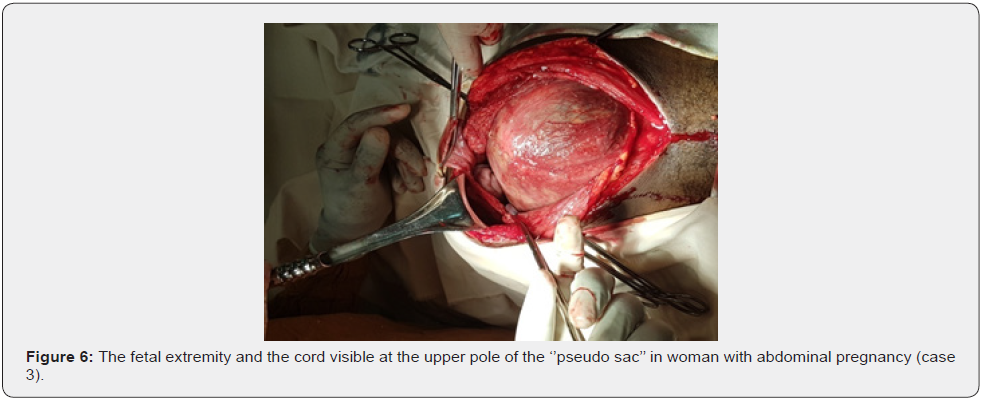
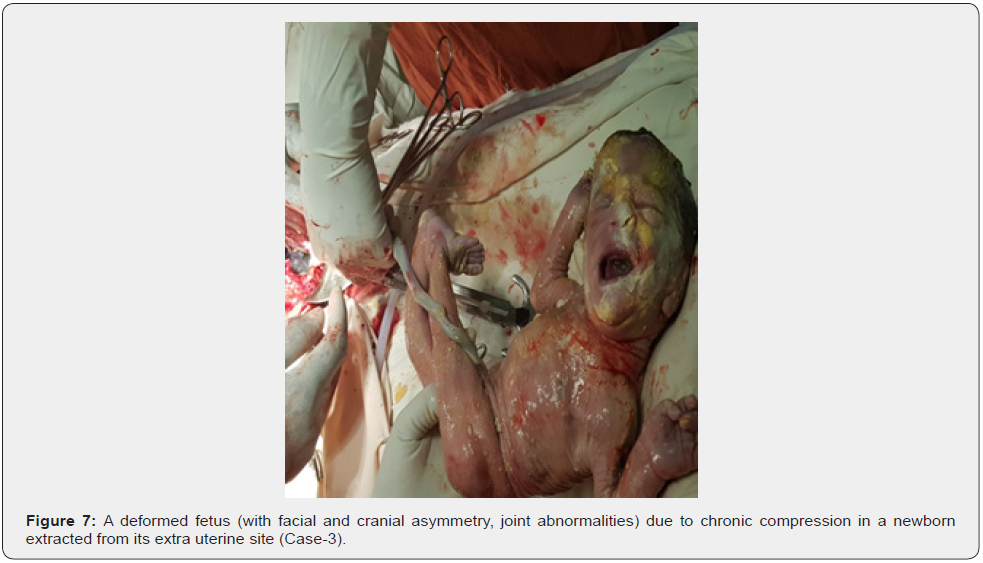
Foetal extremity and umbilical cord were protruding through the upper pole of the mass (Figure 6). Since it was already known that the placenta is posterior, a small incision is made over the anterior surface of the mass (i.e., its sac) and an alive male neonate weighing 1300gm was extracted (Figure 7). The newborn had deformities resulting from compression on the extremities and head was admitted to neonatal ICU and died after six days of admission. The umbilical cord with true note is cut as close as possible to its insertion to placenta and placenta left in situ as it is morbidly attached to the posterior pelvic wall the cul-de-sac, the ceacum and sigmoid colon and posterior wall of the uterus and an attempt to remove the placenta was considered catastrophic (Figure 8).
Post-operatively the patient was closely monitored with vital signs, serial hematocrit measurement, and given broad spectrum antibiotics. After relatively smooth course on her immediate post operative days, the patient starts to have fever and continuous abdominal pain on her third post operative day, which has persisted in spite of changing more antibiotics. With diagnosis of intra-abdominal sepsis, ultrasound revealed significant pelvic collection and anechoic areas within the substance of the placenta. After preparation of blood and informed consent re-laparotomy was decided. Upon re-laparotomy via previous incision, we found about 1000ml of hemorrhagic pus with grossly infected placenta.

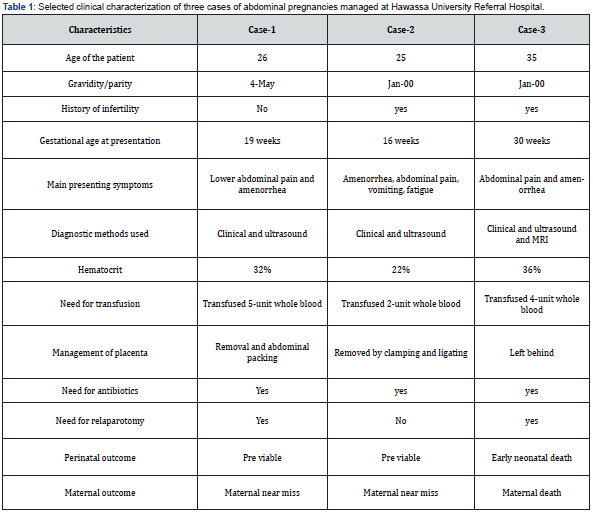
After draining out the pus, the placenta was removed by blunt and sharp dissection from its site of attachments. Bleeding from the site was controlled with ligatures, application of figure of eight stitch at multiple sites and has also required total abdominal hysterectomy to arrest it totally. The patient was transfused with 4 units of whole blood intra-operatively as well as at recovery and broad-spectrum IV antibiotics were continued. Despite these measures, the patient was persistently febrile and on her second post relapartomy day diagnosed with septic shock and died from multiorgan dysfunction due to the underlying condition (Table 1).
Discussion
Abdominal pregnancy is an ectopic pregnancy where the placenta is implanted anywhere in the peritoneal cavity. It could implant on pelvic side walls, parietal peritoneum, over the uterus, the pouch of Douglas, omentum, bowel and mesentry, mesosalpinx. It rarely implants over the liver, spleen, and under the surface of the diaphragm [5]. Primary abdominal pregnancy is a rare form of the pregnancy in which fertilization and implantation occurs primarily in the peritoneal cavity. It is diagnosed by Studdiford’s criteria either at laparotomy or imagings-characterised by normal looking tubes and ovaries, no connection or fistula between the uterus and abdominal cavity, pregnancy should be related only to the peritoneal cavity without signs that it was a tubal pregnancy by any time [5,20].
Secondary abdominal pregnancy is a common form of abdominal pregnancy, the zygote was initially implanted in the uterus, tubes, and ovaries, later re-implanted on the peritoneal structures and survived following tubal abortion or rupture of tubal, uterine or ovarian pregnancy. Sometimes it could occur following uterine perforation during embryo transfer at IVF [5,6]. In both of our cases, being secondary pregnancy is highly likely, because the adnexal tissues were not identified separate from the mass. It can be categorized in to early (up to 20 weeks of gestation) abdominal pregnancy or advanced when the pregnancy is over 20 weeks of gestation with a fetus living or showing signs of having once lived and developed in the mother’s abdominal cavity [5,8].
Broad ligament ectopic pregnancy is a rare form of abdominal pregnancy when the gestational tissue implanted between the two layers of the broad ligament [3]. The mechanism of the development of a broad ligament ectopic pregnancy remains unclear. Primary broad ligament pregnancy postulated to occur due to unsuspected uterine perforation at the time of embryo transfer, or the oocte could migrate abdominally through fistulous tract and fertilized in the broad ligament. It is diagnosed at time of laparotomy using studdiford’s criteria- the uterus located medially to the ectopic pregnancy, the pelvic side walls located laterally, the pelvic floor located inferiorly,and the fallopian tube located superiorly [3,10,20].
Secondary broad ligament pregnancy could occur following rupture of the mesosalpingeal border of tubal pregnancy, or migration of gestation through dehisced uterine scar with implantation in the broad ligament [3, 9]. In our case both possibilities are there because implantation might have occurred primarly, or could follow tubal rupture, but intraoperative findings didn’t fulfill the studdiford’s criteria and she didn’t have any uterine manipulation before.
Abdominal pregnancy more commonly associated with tubal abnormalities (tubal surgery, pelvic infection, adhesion, endometriosis); and also, multi parity, infertility, history of abortion, low socioeconomic status, use of intra uterine devices, use of progestin only pills, prevous history of ectopic pregnancy, smoking, assisted reproduction; but more than half of the cases has no obvious risk factors [1-3,5,6,18]. In our cases low socioeconomic status, multiparity, and history of infertility had been noticed.
There is difference on clinical presentation of abdominal pregnancy. Most clinical features are none specific, and the patient could be asymptomatic. In this case the diagnosis would be delayed, and intervention be made late at term, or could be left unnoticed for years and later diagnosed with Lithopedion [6-14]. High index of suspicion, thorough clinical and ultrasound examination are crucial for early diagnosis and intervention [8]. The cases could present with dull lower abdominal pain during early gestation, like our second case which was overlooked [1].
Women present with abdominal pain, gastrointestinal symptoms, vaginal bleeding, painful fetal movements, hypovolemia & shock. On clinical examination: deranged vital signs, features of anemia, abnormal fetal lie & presentation, easily palpable fetal parts, unexplained fetal demise, free peritoneal fluid, uneffaced cervix at term, and failed induction of labor [5,6,8,11-13]. In our cases most of the clinical features has been noticed, but their diagnoses were delayed due to the patients’ awareness and misdiagnosed on initial encounters.
Ultrasound remains the primary means of diagnoses, but it can be missed frequently due to quality of the machine and operators experience [5,18]. The features are empty uterus, reduced amniotic fluid, absent uterine wall around the fetus, abnormal lie, and abnormal looking placenta with free fluid in the peritoneal cavity. It is also used to diagnose fetal anomalies, common in abdominal pregnancies [5,8]. It was helpful for diagnosis of abdominal pregnancy in our cases, but placental localization and extent of attachment, fetal anatomy, and the pregnancy in the broad ligaments were not well characterized.
Magnetic resonance imaging (MRI) with Doppler has a limited role. It can better be used for fetal imaging, placental location and attachment to visceral organs to plan surgery for the woman [5,19,20]. We also used for 3rd case, helped us to know the extent of placental attachment before surgery.
The treatment of abdominal pregnancy depends on the general condition of the patient, the gestational age of the pregnancy, the resource available. Medical treatment using methotrexate could be considered in few cases, who has stable maternal condition with intact early pregnancy, but the patient needs close monitoring because there is still great risk of rupture with grave consequence [2]. Laparoscopic excision could be another option when the patient condition is stable, with small pregnancy; associated with less blood loss, lower surgical morbidity, and a faster recovery [17,18].
Laparotomy is preferred in most cases of abdominal pregnancy, especially when the patient is hemodynamically unstable and large pregnancy. After fetal delivery the placenta could be removed completely when vascular attachments are easily accessed for ligation, as we did for our second case [6,8,11]. Resection of intraabdominal structures could be considered with the placenta, but partial placental excision or removal in piecemeal are not recommended, which increase the risk of hemorrhage, as we have seen in the first case [5,6].
When placental removal considered difficult, it is preferable to leave the placenta in situ with the umbilical cord tied & cut short, with or without administration of methotrexate, as was done in our 3rd case but placental removal was needed few days later for intraabdominal sepsis [6,8]. In the absence of complications with close medical supervision, conservative management could be considered for previable advanced pregnancy till fetal maturity, but the risks to the mother & the fetus should be clearly discussed with the patient [6,15,16].
Abdominal pregnancy is associated with poor maternal & fetal outcomes. The maternal mortality rate reaches up to 20 %, due to hemorrhage either before surgery following placental abruption, or at time of surgery when securing hemostasis is difficult. The patient could die of sepsis and septic shock, as happened in our third case [8,10].
The maternal morbidity is also high with anemia, infection, pulmonary embolism. It will be worse if the placenta left in situ, with or without methotrexate administration. Accumulated large necrotic tissue predispose to intra-abdominal infection, with peritonitis and abscess collection. Inflammatory mass of the necrotic tissue could lead obstruction of the bowel & ureters, & also fistula formation [3,5,6].
The perinatal outcome is also poor, with perinatal mortality ranging 40-95 % [5,6,8-10]. The perinatal morbidity is also high with perinatal asphyxia, meconium aspiration, fetal anomy and deformity of the head, face, and the extremities [6,10,11]. In our third case, even if it was premature, the neonate had deformities over the face and extremities. The baby died on the 6th postpartum day. Postmortem examination was not made because the family couldn’t give consent for the exam.
Conclusion and Recommendations
Abdominal pregnancy is associated with high maternal morbidity and mortality, and also perinatal mortality. Early diagnosis and intervention could decrease the impact to the mother. In most cases the placenta can safely be removed to decrease the impacts of leaving behind, which has resulted in the death of one of our patients due to uncontrolled sepsis. In the presence of uncontrolled bleeding after placenta removal. leaving pack for tamponade with relaparotomy after 24 hours and removal can successfully be employed as demonstrated in our case.
Acknowledgment
We thank the clients and their family for allowing us to report their pregnancy condition. We would also like to extend our appreciation to residents, interns, midwives, and anesthesia team for their active participation during the management of these cases.
References
- Wondimagegnehu SW, Dejene A, Geremew M (2018) Incidence and determinants of severe maternal outcome in Jimma Universityteaching hospital, south West Ethiopia: a prospective cross-sectional study. BMC Pregnancy and Childbirth 18(1): 255.
- Okechukwu BA, Chidi UOE, Justus NE, Emeka OO, Mathew IN, et al. (2016) Advanced abdominal ectopic pregnancy: A case report. Open Journal of Obstetrics & gynecology 6(6): 360-364.
- Amal AD, Rahma A, Wasima S, Reem B, Ola E, et al. (2011) Full term extra uterine abdominal pregnancy: A case report. Journal of medical case reports 5: 531.
- Susmita S, Nayana P, SPS Goraya, Praveen M (2011) Broad ligament ectopic pregnancy: A case report. Sri Lanka Journal of Obstetrics and Gynecology 33: 60-62.
- Ashraf DM, Azadeh DM (2015) Broad ligament ectopic pregnancy: A case report. Der Pharmacia Lettre 7(10): 1-4.
- Charleen SC, Vincent YTC (2014) Broad ligament ectopic pregnancy: A case report. Case reports from the society of laparoscopic & robotic surgeons.
- Recep Y, Ali K, Fulya A, Ertan A, Mertihan K, et al. (2009) Primary abdominal ectopic pregnancy: A case report. Cases Journal 2: 8485.
- Atif BEF, Vidya R, Hala B, Faikha MA, Sawsan KH, et al. (2018) Abdominal pregnancy: A case report. Open Journal of Obstetrics & Gynecology 8(12): 1198-1204.
- Wondimu G, Delayehu B (2015) Preoperatively diagnosed advanced abdominal pregnancy with surviving neonate: A case report. Journal of medical case reports 9: 228.
- Samar R, Suhasini G, Bal Krishan T, Ranjana G (2013) Full term broad ligament pregnancy through a Cesarean scar: A case report. Obstetrics & Gynecology Science 56(6): 404-407.
- Sheethal CH, Akshata P (2017) Full term secondary broad ligament pregnancy: A rare case. Case reports in women’s health 13: 4-5.
- Mercy NN, Tadele MB, Moreri BN, Elly M (2016) A case report of an asymptomatic late term abdominal pregnancy with live birth at 41 weeks of gestation. BioMed Central research notes 9: 31.
- Dismas M, Nhandi N (2014) Hemoperitoneum in advanced abdominal pregnancy with a live baby: A case reprt. BioMed Central research note 7: 106.
- Nkencho O, Olakunle IM, Peter OE, Zakaa Z, Bright NO (2019) Abdominal pregnancy misdiagnosed as an intrauterine pregnancy: A cause of failed induction of labor for fetal death. International Journal of reproduction, contraception, Obstetrics & Gynecology 8(8): 3382-3386.
- Nafisa AM, Ikram AH, Salah AO, Khalid SK, Abdirizak HA (2016) Calcified abdominal pregnancy with five years of evolution (Lithopedion): A case report. Open Journal of obstetrics & Gynecology 6(8): 515-519.
- Louis M, Sophie M, Marie-Charlotte L, Alexandre M, Marie SA, et al. (2014) Conservative management of an advanced abdominal pregnancy at 22 weeks: A case report. American Journal of perinatology reports 4(1): 55-60.
- Hassan MH, Michael SJ, Luke CD, Gary DVH (2016) Conservative management & planned surgery for previable advanced extra uterine abdominal pregnancy with favorable outcome: A report of two cases. American Journal of perinatology reports 6(3): 301-308.
- Jayashree N, Sobha SN (2016) Broad ligament pregnancy- Success story of a laparoscopically managed case: a case report. Journal of clinical & diagnostic research 10(7): 4-5.
- Xuetang M, Shiyan T, Lee-Jaden-GYKZ, Cuilan L (2018) Management of ectopic pregnancy in a broad ligament & recurrent tubal pregnancy: A case report. Open Journal of Obstetrics & Gynecology 8: 431-436.
- Vartan M, Edmund JHL (2001) MR imaging & MR angiography of an abdominal pregnancy with placental infarction. American Roentgen Ray society 177(6): 1305-1306.






























