Intraoperative Prevention of Adhesions - Is the Key to Reproductive Success
Simrok VV1*, Melnikova DV2, Reznichenko NA3 and Zheltonozka JB4
1Rostov State Medical University, Russia
2Clinic “Lifeline”, Russia
3Medical Academy named after SI Georgievsky, Russia
4Сlinic “Mediland”, Ukraine
Submission: October 29, 2021; Published: November 11, 2021
*Corresponding author: Simrok VV, Rostov State Medical University, Russia
How to cite this article: Simrok V, Melnikova D, Reznichenko N, Zheltonozka J. Intraoperative Prevention of Adhesions - Is the Key to Reproductive Success. J Gynecol Women’s Health 2021: 22(3): 556090. DOI: 10.19080/JGWH.2021.22.556090
Abstract
The effectiveness of the use of anti-adhesive barriers during conservative myomectomy in 54 patients with uterine leiomyoma was studied. The use of intraoperative anti-adhesive barriers improves the course of the postoperative period and prevents the development of adhesions in the pelvis, which increases the reproductive capabilities of the patient.
Keywords: Adhesion; Uterine myoma; Uterine fibroids; Myomectomy; Adhesion barrier; Interceed; Intercoat
Introduction
Peritoneal adhesions following pelvic and abdominal surgery are a frequent cause of intestinal obstruction, reduced fertility, and pelvic pain. In gynecology, adhesion formation at the vaginal cuff and pelvic sidewall frequently involves bowel, omentum, and adnexa. This may result in pelvic pain, dyspareunia, small bowel obstruction, and residual ovary syndrome when salpingo-oophorectomy is not performed [1]. In fact 68% incidence of postoperative adhesion formation is after conservative Myomectomy - is a surgery to remove one or more fibroids.
Although studies have reported adhesions in as many as 88% of women following laparoscopic myomectomy, the majority of studies report similar findings to those of Dubuisson and Takeuchi - approximately 30-40%. This is in contrast to a rate of over 90% adhesion formation quoted by the myomectomy adhesion multicenter group following abdominal myomectomy [2]. The burden of adhesion formation has therefore become a growing concern, and its prevention should be a priority. Our basic concern was to research the effectiveness of usage absorbable adhesion barrier in patients after gynecological operations.
Materials and Methods We investigated 74 patients and in 54 patients we used adhesion barriers, out of which in 37 patients we used INTERCEED because of big surface area of surgical intervention - myomectomy and in the rest of the 17 patients we used INTERCOAT mostly in case of Salpingo-ovariolysis, Salpingo-adhesiolysis and cystectomy. In comparison group of 20 patients with same gynecological pathologies and same surgical interventions but without usage of adhesion barriers. To estimate the efficiency of these methods we investigated our patients with ultrasound investigation, bimanual investigation in postoperative period after 1, 3 and 6 months.
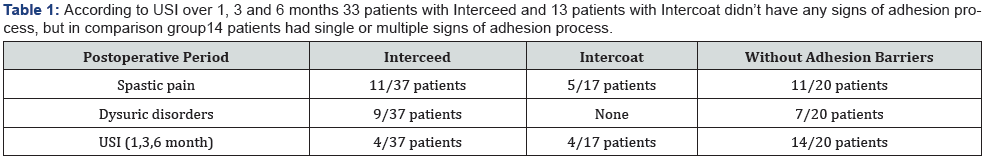
Results our research showed that in our principal group with adhesion barrier the general condition of the patient was much better as in comparison group in postoperative period. In our principal group the spastic pain was decreased by two times, absence of sings of inflammation of urinary bladder and bowel as compared with Comparison group which had long-term dysuric disorders and painful peristalsis. According to USI over 1, 3 and 6 months 33 patients with Interceed and 13 patients with Intercoat didn’t have any signs of adhesion process, but in comparison group14 patients had single or multiple signs of adhesion process (Table 1).
Conclusion
Thus in our study we tried to prove that the usage of adhesion barriers i-e Interceed and Intercoat is important to prevent postoperative adhesion process and its complications and the important role of the uterine fibroid plays in infertility as well as the importance of fibroids removal before the achievement of pregnancy and it also further studies are needed.






























