Prevalence of and Factors Associated with Hormonal Contraceptive use among Undergraduate Students Studying Health-Related Fields
Fernanda Rassi Alvarenga1, Douglas Nunes Stahnke2, Marcos Pascoal Patussi2 and Juvenal Soares Dias da Costa2*
1Faculdade de Medicina, Universidade de Rio Verde, Brazil
2Universidade do Vale do Rio dos Sinos, Brazil
Submission: November 01, 2021; Published: November 10, 2021
*Corresponding author: Juvenal Soares Dias da Costa, Universidade do Vale do Rio dos Sinos, Brazil
How to cite this article: Fernanda R A, Douglas N S, Marcos P P, Juvenal S D d C. Prevalence of and Factors Associated with Hormonal Contraceptive use among Undergraduate Students Studying Health-Related Fields. J Gynecol Women’s Health 2021: 22(3): 556089. DOI: 10.19080/JGWH.2021.22.556089
Abstract
Introduction: Contraceptive use by females of reproductive age has significantly increased. Studies of contraceptive use have shown that choice of the method is dependent on several factors. Objective: This study investigated con-traceptive use by university students and attempted to verify the factors associated with hormonal contraceptive use.
Methods: A cross-sectional, school-based study was conducted among female university students studying health-related fields who were 18 years or older, sexually active, and enrolled full-time at the institution. A standard-ized, pre-coded, self-administered questionnaire comprising specific questions related to contraceptive use was completed by participants and 1288 females were included in the study. Demographic, socioeconomic, academic, religious, sexual, and reproductive factors were evaluated from October to December 2018. Descriptive statistics were used for data. Poisson regression with robust variance was used according to the conceptual analysis model. Variables associated with the outcome were retained in the model (p≤0.20 was used to adjust for confounding fac-tors; p<0.05 was considered significant). Results: The most frequently used contraceptive methods were contracep-tive pills (66.5%) and male condoms (43.9%). The prevalence of all hormonal contraceptives was 81.50%. The multivariate regression analysis showed that hormonal contraceptive use was most prevalent among female stu-dents 23 to 24 years of age who were living with friends, from economic class A, and did not practice any religion.
Conclusion: Contraceptive use by students has limited diversity; therefore, more studies involving representative samples of this population are necessary to monitor trends in and guide intervention efforts for sexual and reproduc-tive health.
Keywords: Contraception; Contraceptive methods; Hormonal contraceptives; Undergraduate students
Abbreviations: HIV: Human Immunodeficiency Virus; STI: Sexually Transmitted Infection
Introduction
Recently, there has been an increase in the number of adolescents and young adults engaging in sexual activ-ity, and the average age at which sexual activity is initiated has become younger [1]. Concomitantly, there has been a significant increase in the use of contraception, with approximately 60% of females of reproductive age using some form of contraception [2]. In Brazil, contraceptive use was investigated using the Brazilian National Survey of De-mography and Health (PNDS), which was conducted in 1996 and 2006. The 2006 results showed that 66% of sexual-ly active individuals 15 to 19 years of age have used at least one contraceptive method [3].
Studies of contraceptive use have shown a high prevalence among youth (age 15-24 years), and that the choice of method depends on the relationship, partner, reproductive intentions, sociocultural and religious issues, method affordability, and access to different methods [4-7]. However, other factors, such as the absence of a stable relationship, influence the use, non-use, and inappropriate use of contraception [8,9]. Studies involving female uni-versity students confirmed a high prevalence of contraceptive use among them [10], as well as inconsistent usage practices and misuse, thereby exposing them to the risks of unplanned pregnancies, induced abortions, and sexually transmitted infections (STIs). Therefore, the use of contraception, especially by young individuals, is associated with the prevention of STIs, unwanted pregnancies, and other consequences [11,12].
According to the World Health Organization and the eligibility criteria for the use of different contraceptive methods, there is no ideal contraceptive for all individuals, and age is not a limitation to any contraceptive method [4]. It is important to know the available contraceptive options so individuals can make the most appropriate choice by considering characteristics such as frequency of sexual activity, number of partners, desire to avoid pregnancy, and lifestyle, as well as the characteristics inherent to each method, such as its function, effectiveness, possible side effects, and whether it requires follow-up (such as a prescription or medical examination).
Currently, several contraceptive methods are available. Oral hormonal contraceptive pills are the most commonly used method of contraception. This method is quite effective if used correctly. Additionally, hormonal contraceptives may have additional benefits, such as the treatment of dysmenorrhea, acne, premenstrual tension, ovarian cysts, and endometriosis. However, they may have adverse effects as well; for example, they can cause slight increases in blood pressure, thromboembolism, diabetes mellitus, and cardiovascular events [13].
This study aimed to describe the contraceptive methods used by female undergraduate students studying health-related fields at a university in midwestern Brazil. It also intended to verify the use of and factors associated with hormonal contraceptive methods to help guide intervention efforts for reproductive planning.
Materials and Methods
This research study was performed to verify the living and health conditions of students studying health-related fields at the University of Rio Verde. In 2018, the University of Rio Verde had approximately 7000 students enrolled in 21 undergraduate programs and 15 postgraduate programs. The University of Rio Verde has three cam-puses, Rio Verde (southwest region), Aparecida de Goiania (metropolitan region of Goiania), and Goianesia (north-ern region). This cross-sectional study included female undergraduate students who were studying nursing, dentis-try, medicine, physiotherapy, pharmacy, or physical education courses, 18 years or older, sexually active, and not pregnant at the time of data collection (N=2620 students).
The sample size was calculated based on a 60% prevalence of contraceptive use. A power of 80% was con-sidered to identify a prevalence ratio of 1.13 with a confidence level of 95% and an error rate of 3%. The sample size was increased by 10% to account for possible losses and refusals, and by 15% to control for confounding factors. Therefore, the sample size was estimated to be 743 participants. Ultimately, 1288 females were included in the study.
Data were collected using a standardized, pre-tested, self-administered questionnaire that was completed anonymously by university students from October to December 2018. The questionnaire consisted of 209 questions and was completed in the classroom. If students did not attend the first questionnaire session, then two more at-tempts were made so that they could complete it. The researchers involved in this project were responsible for dis-tributing the questionnaire. Training was performed and an instruction manual was created to standardize the appli-cation of the data collection and coding instrument. Additionally, a pilot study was conducted with university students studying law to improve the instrument and its logistics.
The types of contraceptive methods used by sexually active females were described. For the association analysis, the outcome was the use of hormonal contraceptive methods such as contraceptive pills, injectable contra-ceptives, transdermal patches, vaginal rings, subcutaneous progesterone implants, and intrauterine hormonal sys-tems. Demographic, socioeconomic, education, religion, and reproductive variables were analyzed. Demographic variables included age (age groups: 18–20 years; 21-22 years; 23-24 years; 25 years or older), self-reported race (white or non-white), relationship status (with or without a partner), and living situation (living alone; living with a partner, parents, or guardians; living with friends or colleagues).
Economic classes according to the Brazilian Association of Companies and Research were included in the analysis. Classes were categorized as A (high) , B (medium), or C/D/E (low) based on the possession of certain ma-terial goods, education of the head of the family, presence of domestic servants, and availability of public services at the location of the residence.
The student variables were course of study (medicine, dentistry, and other health-related fields) and course periods (six or fewer semesters completed or seven or more semesters completed). The religion variable was cate-gorized as Catholic, Protestant/Evangelical, other religions, and no religion. Regarding reproductive variables, the following were included in the analysis: sexarche (categorized by age group: 15 years or younger; 16-17 years; 18 years or older); number of sexual partners during the past year (one, two, three, or more than three); and parity (children or no children).
The database was created using the Epi data 3.1 program; double entry was performed to reduce typing errors. A descriptive analysis was performed to calculate the frequency of contraceptive use and the prevalence rates of the contraceptive methods. Crude and adjusted analyses, confidence intervals, and significance levels were per-formed using the chi-square test and Stata software version 12.0 for hormonal contraceptive methods.
For the adjusted analysis, Poisson regression was performed using a hierarchical model. Therefore, the demographic and socioeconomic variables were placed at the distal level, the variables related to student character-istics and religion were placed at the second level, and the variables related to sexual and reproductive characteris-tics were placed at the proximal level; all of these determined the outcomes of using hormonal contraceptives. Vari-ables were entered into the model if they had statistical significance of 20% (p≤0.2) in the crude analysis; further-more, they were retained in the model if they had a significance level of 5% (p<0.05).
This research project was approved by the research ethics committees of the University of Vale do Rio dos Sinos (no. 2,892,764; September 13, 2018) and the University of Rio Verde (no. 2,905,704; on September 19, 2018). The participants were informed about the objectives and procedures of the research and were allowed to participate after signing the informed consent form.
Result
Of the total sample of university students participating in the project, 1593 were female; of these, 1288 (80.8%) reported being sexually active. The prevalence of contraceptive use was 85.9% (95% confidence interval, 83.3%-87.2%), and the most frequently used contraceptive methods were contraceptive pills (66.5%) and male condoms (43.9%). Additionally, the analysis showed that 257 (20%) participants reported withdrawal as their method of contraception, 234 (18.2%) reported the morning-after pill as their method of contraception, and 124 (9.6%) reported using other methods of contraception (Table 1).
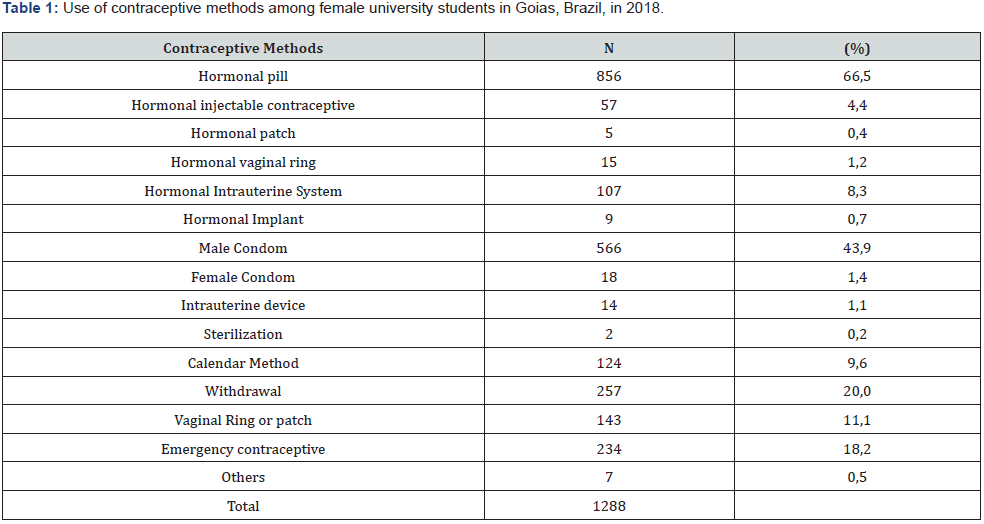
The prevalence of hormonal contraceptive use was 81.5%. In addition to contraceptive pill users, 8.3% of the participants reported using a hormonal intrauterine system, 4.4% reported using injectable hormonal contracep-tives, 1.2% reported using a vaginal contraceptive ring, 0.7% reported using subdermic hormonal implants, and 0.4% reported using an intradermic contraceptive adhesive (Table 1).
According to the demographic variables of the sample, most participants were between 21 and 22 years old (36%) and were white (58.3%). Regarding the relationship status, there was a predominance of females without a partner (86.8%). The economic class distribution showed that 87.6% of females were classified as classes A and B. Furthermore, 52.4% lived with parents, guardians, or partners, 68.1% were studying medicine, and 61.7% complet-ed up to six semesters of courses. The predominant religion was Catholic (56.2%). Regarding sexual and reproduc-tive characteristics, the majority (41.3%) reported that their age when they first had sexual intercourse was older than 18 years, 61.7% reported having only one sexual partner, and 92.9% reported having no children (Table 2).
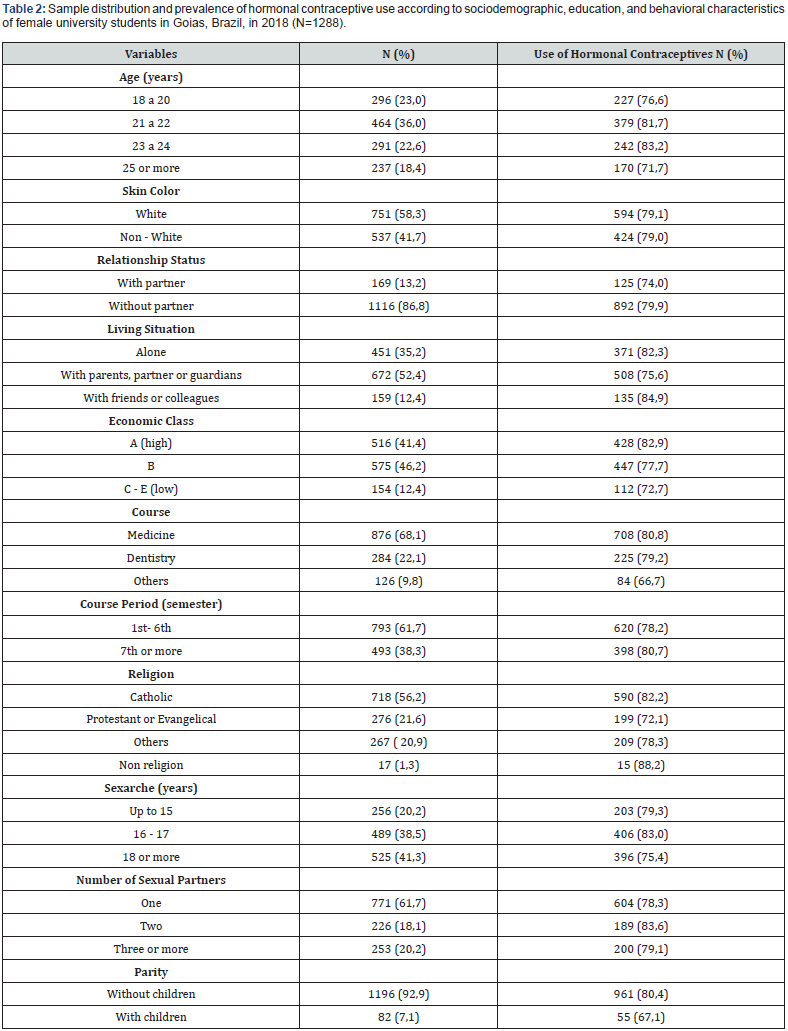
The distribution of the use of hormonal contraceptive methods was observed according to the characteris-tics of the study sample. The highest prevalence of use was observed among females who were 23 to 24 years of age, without a partner, from economic classes A and B, living with friends, studying medicine, practicing no religion, and completing the second half of their coursework. Regarding behavioral characteristics related to sexual and/or repro-ductive life choices, a higher prevalence of hormonal contraceptive use was observed among those who were be-tween 16 and 17 years old when they first had sexual intercourse, had two sexual partners, and had no children.
The crude analysis showed an association between age and the use of hormonal contraceptive methods; however, the confidence intervals encompassed unit values. Regarding the relationship status, statistically signifi-cant differences indicating that females without a partner chose hormonal contraceptives more often than females with a partner were observed. Students living with friends and living alone also had a higher prevalence of hormonal contraceptive use. Race was not a statistically significant variable for the use of hormonal contraceptive methods. The analysis of socioeconomic characteristics showed significant differences and revealed a higher prevalence of hormonal contraceptive use among females from economic class A (Table 3).
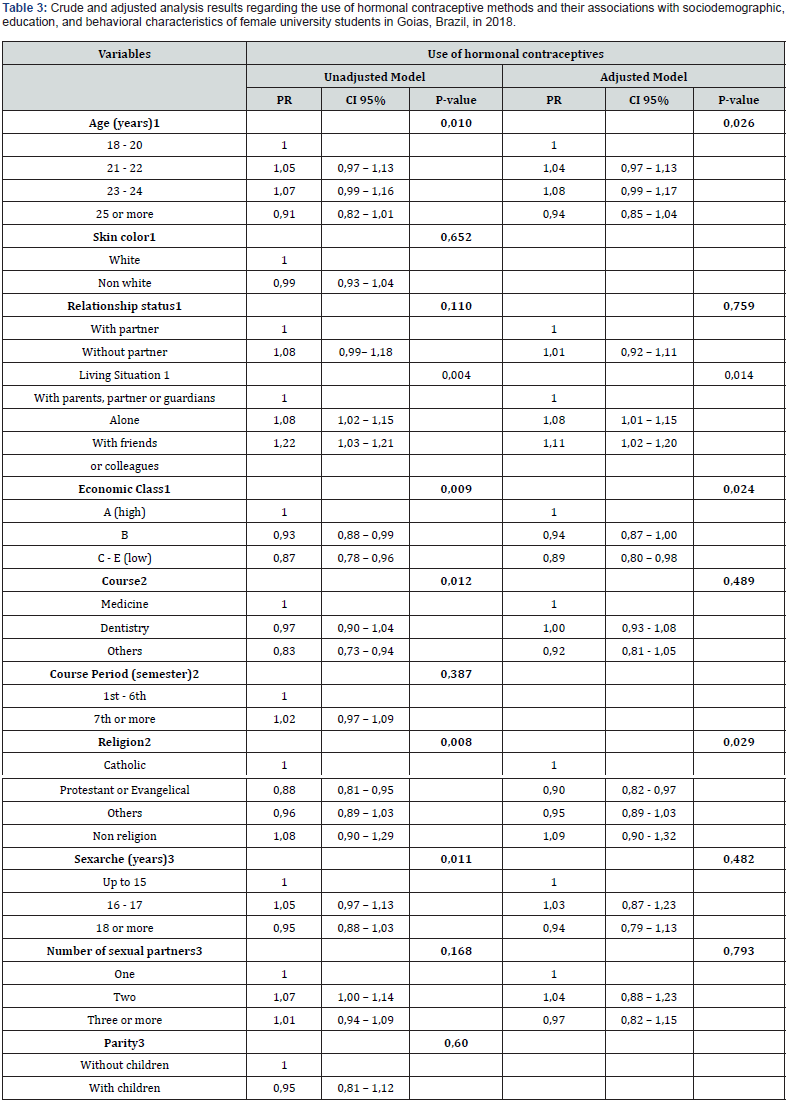
Regarding student characteristics, females studying medicine had a higher prevalence of hormonal contra-ceptive use. The course period was not associated with the outcome (Table 3). The university students who declared that they practice no religion, those who first had sexual intercourse between the ages of 16 and 17 years, and those who reported two sexual partners more often chose hormonal con-traceptive methods. Parity was not associated with the use of hormonal contraceptives (Table 3).
According to the adjusted analysis, age, living situation, economic class, and religion were retained in the adjusted analysis, which showed that that those 23 to 24 years of age, living with friends, from economic class A, and without religion were more likely to use hormonal contraceptives (Table 3).
95% CI: 95% confidence interval; PR, prevalence ratio. Each variable was adjusted to the others at the same or pre-vious level in a hierarchical model of causality. Only variables associated with the outcome at P ≤ 0.20 in the unad-justed model were subsequently entered and retained in the final multivariateadjusted model. 1st Level - Variables adjusted to each other. 2nd Level - Variables adjusted to each other and for age, economic class and residence. 3rd Level - Adjustable variables among themselves and for age, economic class, residence, course and religion
Discussion
During this study, the majority of females who reported being sexually active had a high prevalence of con-traceptive use. A similar result was found during a European cross-sectional study of university students using a self-administered questionnaire that showed a 93% prevalence of being sexually active and an 86.9% prevalence of contraceptive use during the first sexual intercourse experience [14]. An analysis conducted in São Paulo, Brazil, involving 258 public university students found a high prevalence of contraceptive use during their last relationship with sexual involvement, and 100% of the sample reported the general use of contraceptive methods [15]. A study performed in Curitiba in 2020 that involved 1036 university students with an average age of 21.2 years reported that 41.6% were enrolled in healthrelated courses, 87.2% were sexually active, and 89.3% used contraception [16]. Other studies of female university students showed a lower prevalence. One study including 23 universities from 22 countries in Asia and Africa showed a 57.4% prevalence of contraceptive use by a sample of female university stu-dents [10]. Another large study performed in the United States that analyzed trends in the use of contraceptive meth-ods by 97,376 university students from 2008 to 2013 found contraceptive use prevalence rates of 45% in 2008 and 44% in 2013 [17]. In the midwestern city of Goiânia in Brazil, a study involving 178 nursing students in 2014 showed a 52% prevalence of general contraceptive use [18].
In the present study, contraceptive pills and male condoms were the most commonly used contraceptive methods. Other school-based studies performed in Brazil found a higher prevalence, however. In the southeastern region of Brazil, a study performed at a public university in São Paulo in 2010 found rates of 69.5% and 79.2% for contraceptive pill and male condom use, respectively [15]. Another study performed in southern Brazil that aimed to verify the use of contraceptive methods during the first sexual intercourse experience among 293 university students in 2015 found prevalence rates of 82.7% and 87.7% for the contraceptive pill and male condom, respectively [19]. During the study in Curitiba, in 2020, the most commonly used methods were the contraceptive pill and the male condom, with prevalence rates of 79.1% and 37%, respectively [16]. In contrast, during a study conducted in the midwestern region of Brazil that included 270 females enrolled in health-related courses at a private university, the prevalence rates were only 24.8% for contraceptive pills and 30.7% for male condoms [20].
As expected, contraceptive pills were the predominant form of hormonal contraception, followed by hor-monal intrauterine systems, long-term reversible contraceptives, and injectable contraceptives. Studies conducted in different countries have shown different regional patterns in the use of hormonal contraceptive methods. Short-term reversible methods have been most commonly used in Africa and Europe, and long-term or permanent methods have been most commonly used in Asia and North America. In Latin America, the Caribbean, and Oceania, combina-tions of different methods are used [21]. In the United States, a study to verify contraceptive use trends over time showed a progressive increase in the use of long-term reversible contraceptives from 1% in 2008 to 4% in 2013, with race, age, relationship status, and sexual orientation being associated factors [16]. In Brazil, a cross-sectional, population-based study including 20,404 urban Brazilian households and data reported by females 15 to 49 years of age showed differences in the prevalence of oral contraceptive use, with higher rates in the southern region (37.5%) and lower rates in the northern region (15.7%). Regarding injectable contraceptives, no differences were detected between regions, with a total prevalence of 4.5% [22].
Interestingly, two contraceptive methods, the male condom and the contraceptive pill, were used most commonly, and the prevalence rates for more modern methods of contraception, such as the intrauterine contracep-tive device, vaginal ring, and injectable hormonal implants, were low. There was also a high frequency of the use of other methods such as withdrawal and emergency contraception, even though they may not have been used routine-ly.
The male condom is a barrier method of contraception that has the advantage of providing protection against unwanted pregnancy and STIs such as HIV [23]. It is one of the oldest and most popular forms of contracep-tion and is 95% effective if used correctly. Furthermore, it can be safely used by all age groups and is easily accessi-ble from public and private health services [24]. Therefore, it would be expected to have a higher prevalence of use among adolescents (15-19 years) and young adults (20-24 years), especially university students, because they are highly educated and have access to information. Traditional or natural methods, such as withdrawal, are considered unreliable and have high failure rates [23]; therefore, they should be discouraged for contraception.
Emergency contraception consists of ingesting an isolated progesterone pill within 72 hours after sexual intercourse that was unprotected because of situations involving forgetting to use or inappropriate use of the regular contraceptive method, condom failure (broken condom), or sexual violence. However, routine use compromises the effectiveness of emergency contraception. A study of public university students in São Paulo, Brazil, found a 50% prevalence of emergency contraceptive use, and that 15% of females did not demonstrate adequate knowledge about emergency contraception, such as its inability to prevent STIs [25]. Furthermore, 56.1% of female private university students in southern Brazil reported using emergency contraception, 11.4% of them reported having used it more than twice within 1 year, and 10.7% reported that they did not use contraception continuously [16]. Another study of university students studying nursing in the midwestern region of Brazil found a 29% prevalence rate of emergen-cy contraception use, and that correct answers to questions about emergency contraception were provided by less than 50% of these students [18]. These results are worrying because the frequent use of emergency contraception is a marker of risky sexual behavior and may indicate exposure to unprotected sex or poor adherence to regular contra-ceptive use, resulting in vulnerability to unplanned pregnancy.
Several studies have shown that contraceptive practices by youth are related to several factors, such as their current relationship, partner, and sociocultural and religious issues, as well as other aspects such as socioeconomic level, method affordability, and access to different methods [5-7,26]. During this study, age, economic class, living situation, and religion significantly influenced the use of hormonal contraceptives. The results observed for univer-sity students aged 23 to 24 years with a higher economic class who were living with friends and did not practice any religion were related to a higher prevalence of contraceptive use and indicated trends among university students. Other studies have reported similar results. A multicenter study performed in Asia and Africa showed that factors such as younger age, having a religious affiliation, and sexually protective behavior (not being pregnant at the time of the interview and not having multiple sexual partners) were associated with the non-use of contraceptives among sexually active university students [10]. In the United States, a study that analyzed the prevalence of and factors associated with the consistent use of contraceptives by 842 university students found that self-esteem, confidence, independence, and satisfaction with life were positively associated with the consistent use of contraceptives [27].
It was elucidated that educated young individuals still have inconsistencies in their use of contraception and in their prevention of STIs and have little knowledge of and a low prevalence of using long-term reversible con-traceptives, which are safe and highly effective for their age group. Because this was a cross-sectional study of a population restricted to a particular university, it is not representative of all female university students in Brazil. There were also limitations to determining all factors involved in decisions regarding contraceptive use by female university students, and limitations to evaluating situations involving contraindications to contraceptive methods, adverse effects of contraceptive, and adequate adherence to contraception throughout the reproductive life. However, because of the sample size and methodological rigor, these results reflect trends that indicate that it is necessary to expand interventions aimed at reproductive guidance and reproductive planning for students in Brazil.
Conclusion
There is little diversity in the contraceptive methods used by university students studying health-related fields, and their contraceptive choices are related to sociocultural and religious reasons. These results do not differ from those of other females in different age groups or even females of the same age but with less education and greater difficulty accessing information and different contraceptive methods.
Acknowledgement
Stahnke received a scholarship from Brazilian Federal Agency for Support and Evaluation of Graduated Education (CAPESPROSUC).
Contributors
Dias-da-Costa JS, Patussi MP, contributed to the conception and design of the study, review of the analysis, critical review and final approval of the manuscript. Stahnke DN contributed to the data analysis and interpretation. All the authors have approved the final version and are responsible for all aspects of this work, including guaranteeing its accuracy and integrity.
References
- Boislard MA, Boungardt VDD, Blais M (2016) Sexuality (and lack) in adolescence and early adulthood: A review of the literature. Behavioral Sci 6(1): 8.
- Alkema L, Kantorova V, Menozzi C, Biddlecom A (2013) National, regional, and global rates and trends in contraceptive prevalence and unmet need for family planning between 1990 and 2015: a systematic and comprehensive analysis. Lancet 381(9878): 1642-1652.
- Brazil Ministry of Health (2009) Brazilian Center for Analysis and Planning. National survey on demography and health of children and women - PNDS 2006: dimensions of the reproductive pro-cess and child health. Ministry of Health, Brasília (DF), Brazil.
- World Health Organization (2015) Medical eligibility criteria for contraceptive use: A WHO Family Planning Cornerstone. In: (5th edn), World Health Organization, Switzerland.
- Stenhamar C, Tiblom EY, Åkerud H, Larsson M, Tydén T, et al. (2015) Sexual and contraceptive behavior among female university students in Sweden–repeated surveys over a 25‐year period. Acta Obstet Gynecol Scand 94(3): 253-259.
- Kransdorf LN, Raghu TS, Kling JM, David PS, Vegunta S, et al. (2016) Reproductive life planning: a cross-sectional study of what college students know and believe. Matern Child Health J 20(6): 1161-1169.
- Ahmed ZD, Baffa SI, Lukman AM, Mohammed Y, Nguku P, et al. (2017) Knowledge and utiliza-tion of contraceptive devices among unmarried undergraduate students of a tertiary institution in Kano State, Nigeria 2016. Pan African Med J 26: 103.
- Bastos BM, Scoppetta SAF, Quadro SM, Rezende RS (2018) Low level of knowledge of contraceptive methods among pregnant teens in Brazil. J Pediatr Adolesc Gynecol 31(3): 281-284.
- Hoopes AJ, Teal SB, Akers AY, Sheeder J (2017) Low acceptability of certain contraceptive methods among young women. J Pediatr Adolesc Gynecol 31(3): 274-280.
- Peltzer K, Pengpid S (2015) Contraceptive non-use and associated factors among university students in 22 countries. African Health Sci 15(4): 1056-1064.
- Sorensen NO, Marcussen S, Grønbæk BM, Juhl M, Schmidt L, et al. (2016) Fertility awareness and attitudes towards parenthood among Danish university college students. Reprod Health 13(1): 146.
- Silveira RE, Santos AS, Borges MR (2014) Possible influences on the sexuality of university stu-dents in the REFACS health area (online). 2(Suppl 2): 143-148.
- Brazilian Federation of Gynecology and Obstetrics Associations (2015) Contraceptive Manual. Bra-zilian Federation of Gynecology and Obstetrics Associations (FEBRASGO), Brazil.
- Leon-Larios F, Macias-Seda J (2017) Factors related to healthy sexual and contraceptive behaviors in undergraduate students at university of Seville: a cross-sectional study. Reprod Health 14(1): 179.
- Pirotta KCM, Schor N (2004) Reproductive intentions and fertility regulation practices among uni-versity students. J Public Health 38(4): 495-502.
- Moraes LP, Jones KLG, Pellegrini LE, Silva LF, Barbosa LM, et al. (2020) Analysis of the profile of students at a university in Curitiba regarding the use of contraceptive methods. Arq Med Hosp Fac Cienc Med Santa Casa São Paulo 65: e25.
- Logan RG, Thompson EL, Ramos CA, Griner SB, Vázquez-Otero C, et al. (2018) Is long-acting reversible contraceptive use increasing? Assessing trends among U.S. college women, 2008–2013. Matern Child Health J 22(11): 1639-1646.
- Veloso DLC, Costa PV, da Silveira ODCLJ, Marques SAK, Valadares GJ, et al. (2014) Emergency contraception: knowledge and attitude of nursing students. Revista Gaúcha de Enfermagem 35(2): 33-39.
- Delatorre MZ, Dias ACG (2015) Knowledge and practices on contraceptive methods in university students. SPAGESP Magazine 16(1): 60-73.
- Ferreira JB, Costa APV, Chagas ACF (2018) The practice of using emergency contraception in uni-versity students at a private institution in Campo Grande-MS. Revista Recien. Sci J Nurs 8(22): 3.
- Darroch JE, Singh S (2013) Trends in contraceptive need and use in developing countries in 2003, 2008, and 2012: an analysis of national surveys. Lancet 381(9879): 1756-1762.
- Farias MR, Nair LS, Leão TNU, Oliveira MA, Dourado APS, et al. (2016) Use and ac-cess to oral and injectable contraceptives in Brazil. Rev Saúde Pública 50(Suppl 2): 14s.
- Rakhi J, Sumathi M (2011) Contraceptive methods: Needs, options and utilization. J Obstet Gynecol India 61(6): 626-634.
- Colquitt CW, Martin TS (2017) Contraceptive methods: a review of non-barrier and barrier products. J Pharmacy Pract 30(1): 130-135.
- Orges ALV, Fujimori E, Komura HLA, Vieira CM (2010) Contraceptive practices among university students: the use of emergency contraception. Cad Saude Publica 26(4): 816-826.
- Donadiki EM, Jimenez-Garcıa R, Velonakis EG, Hernandez-Barrera V, Sourtzi P, et al. (2013) Factors related to contraceptive methods among female higher education students in Greece. J Pediatr Adolesc Gynecol 26(6): 334-339.
- Morrison LF, Sieving RE, Pettingell SL, Hellerstedt WL, McMorris BJ, et al. (2016) Protective factors, risk indicators, and contraceptive consistency among college women. J Obstet Gynecol Neonatal Nurs 45(2): 155-165.






























