Assessment of Factors Associated with the Intake of Folic Acid in the Periconceptional Period
López Martín Sofía BM1 and Herrero Rivera Daniel2*
1Department of Gynecology and Obstetrics. Virgen del Rocío University Hospital, Spain
2Depatment of Medical Oncology, Virgen del Rocío University Hospital, Spain
Submission: December 11, 2020;Published: December 17, 2020
*Corresponding author: Daniel Herrero Rivera, Department of Medical Oncology, Virgen del Rocío University Hospital, Spain
How to cite this article: López M S B, Herrero R D. Assessment of Factors Associated with the Intake of Folic Acid in the Periconceptional Period. J Gynecol Women’s Health. 2020: 20(3): 556038. DOI: 10.19080/JGWH.2020.19.556038
Abstract
Background:We have knowledge that the lack of folic acid around 27-28 day after conception, can cause open neural tube defects (NTDs). Our primary objective is to determine the folic acid intake in pregnant women and as a secondary objective, the level of maternal knowledge about the implications of it.
Method:Observational, multicentric study of 305 women from 3 different institutions. The Chi-square statistical test (χ2) was used for the analysis. It has been considered a p < 0.05 and a 95% confidence interval. The data were analysed with the IBM SPSS 21.0 statistical package.
Findings:Only 22.6%(n=69) of our spelling took the folate in the recommended period, from one month before pregnancy to labour. Women with a greater likelihood of taking folate supplementation in this period were those with university degree (OR=7.88, p=0.003), employees or self-employed (OR=3.72, p<0.001), health sector workers (OR=2.33; p=0.44), those who had planned their pregnancy (OR=5.96, p<0.001) and who achieved their pregnancy through assisted reproduction techniques (ART) (OR=9.73, p<0.001).
Conclusion:This study findings add to the evidence that there are variable rates of consumption of periconceptional folic acid in the recomended period. Future research will be conducted to validate risk factors that decrease supplementation.
Keywords: Pregnancy; Folic acid; Maternal nutrition; Neural tube defects; Periconceptional period
Abbreviations: PE: Primary Education; SE: Secondary Education; PTS: Professional Training Studies; BD: Bachelor´s degree; UD: University degree; ART: Assisted Reproduction Techniques; UD: University degree
Introduction
Folate it is a water-soluble vitamin, namely vitamin B9, found in legumes, leafy green vegetables, fruits, as well as in dairy products and veal liver [1]. The bioavailability of folic acid is approximately 70% higher than that of folate naturally contained in foods, although there are wide variations depending on the methodology used in the measurement [2]. The function of folate is in any process of cell division. Sufficient folate is critical for the synthesis of fetal cell DNA and RNA [3].
Folic acid deficiency around day 27-28 after conception, a period in which most women are not aware that they are pregnant, can cause open NTDs [4-6], that include several malformations [7-9] affecting health, growth, and learning and may be evident immediately after birth or grammer later in life [10-12]. The prevalence of open NTDs worldwide is highly variable. In 2016 a systematic review showed that in Eastern Mediterranean, the prevalence of NTD is the highest of the all geographical areas, with 21.9 per 10,000 births. In Europe the prevalence is lower, 9.0 per 10,000 births [1,9,13].
These data have provided the evidence gynaecologists, midwives and primary care physicians to encourage women of childbearing age to take folic acid supplements in the periconceptional period [14]. Because of the high prevalence of NTD since 1992, the Public Health Service of the United States recommends daily supplementation with 400μg of folic acid for all women of reproductive age [14]. In the United Kingdom (UK), an update of the Scientific Advisory Comittee on Nutrition (SACN) in 2017, also recommended 400 μg of folic acid supplementation until the twelfth week of pregnancy and adds that those women with a history of a previous NTD-affected pregnancy are advised to increase consumption to 5mg/d [15].
Beginning in 1998, the World Health Organization (WHO) recommended to take 400μg of folic acid from preconception and up to 12 weeks of pregnancy [16,17]. This is included in the Clinical Practice Guide (CPG) for Pregnancy and Puerperium Care of the National Health System (NHS) [18]. For women with a history of giving birth to a newborn with a NTD, the recommended daily dose is 5mg of folic acid in addition to dietary advice to increase dietary folate intake [18-20]. There are more limited evidences to recommend high dosis with other high-risk groups such as those with family history of an NTD, antiepileptic drug therapy, maternal medical conditions like malabsorption or preexisting diabetes. This is also stated in the CPG of the referred NHS.
Some obstetricians and/or midwives claim to recommend that women continue to take folic acid until the end of pregnancy, due to the multiple benefits that this has for pregnant woman, childbirth, and puerperium [20,21]. According to the U.S. National Toxicology Program and the UK SACN, they reported little evidence of adverse effects related to folic acid fortification above the normal upper limit [22]. Our primary objective is to determine the folic acid intake in a Spanish pregnant women cohort to assesed the consumption in our country and compare data with those describe in other countries in this setting.
Material and Methods
Design
Observational, multicentre study of a representative sample of 305 women from 3 different Spanish health institutions. The data analysed in the study were collected, with the patient consent, through questionnaires prepared for this purpose to obtain information on folic acid intake between January and March 2018. The information collected in this research has been obtained exclusively from human participants with the approval of the health institution where the data has been collected in accordance with the 1964 Declaration of Helsinki and its later amendments. Different sociodemographic variables (age, place of origin, place of residence, level of education, employment status and profession), gynaecobstetrics (parity, type of birth, habitual contraception, gestational planning, spontaneity of gestation) and their relationship with the time of initiation and completion of folic acid intake as the primary objective of the study have been studied. As a secondary objective, the level of maternal knowledge about the folic acid has been studied. The study variables are shown in Table 1. Inclusion criteria included all women who have given birth to at least one living child in one of the three institutions. Exclusion criteria included those women who do not wish to participate in the study and those who have given birth to a deceased fetus.
Statistical analysis
The association between sociodemographic and gynaecobstetric variables with the time of onset and completion of folic acid intake, as well as with the level of maternal knowledge about it, has been assessed independently using the Chi- square statistical test (χ2). It has been considered a statistically significant level values of p < 0.05. A 95% confidence interval has been taken into account for the adequate estimation of the results. The data were analysed with the IBM SPSS 21.0 statistical package.
Result
Characteristics of patients
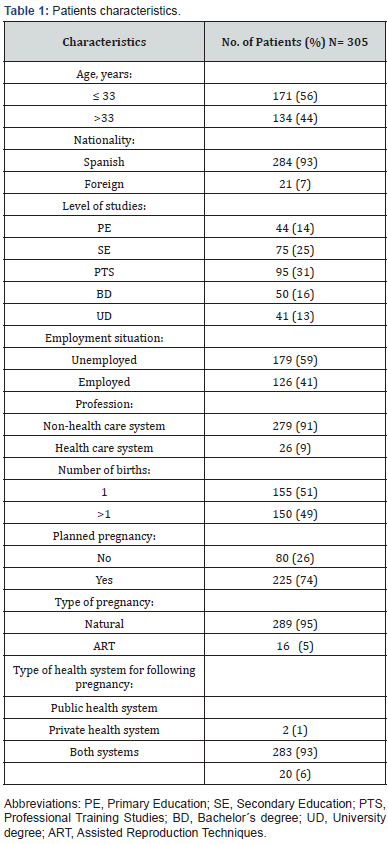
The characteristics of the 305 postpartum women are shown in Table 1. The median age of the study cohort was 33 years (range 17-50 years). 93% of those surveyed were Spanish. The type of health system chosen by the women for the follow-up of their pregnancy had been the public system in 93% of cases. 41% of the women in the study sample were not employed, while 59% of them were employed or self-employed. Of all postpartum women, 14% said they have primary education, 25% have completed obligatory secondary education, 31% have vocational training, 16% have a bachelor’s degree and 13% ratify having university degree. Of all those surveyed, 9% belonged to the health sector. 49% of women in the study had more than one child. Of the sample, 74% said they had planned their pregnancy and only 5% confirmed having had a pregnancy using assisted reproduction techniques (ART).
Start of folic acid intake
Related to the folic acid intake, of the 305 women surveyed, only 26.6% (81) began taking the supplement following international recommendations, that is, before pregnancy, compared to 73.4% (224) who began taking it during the first trimester of pregnancy. All the outcome of start of folic acid intake is shown in Figure 1.
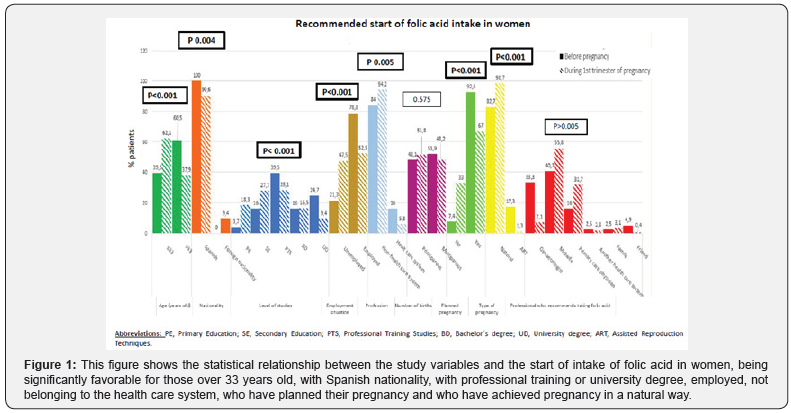
All the women who started taking it at the recommended time (n=81) were of Spanish nationality. Concerning the level of studies, 39.5% expressed having professional training studies and 24.7% university students.78.8% were workers, compared to 21.3% who said they were not doing any paid job. The majority of women who started with folate before becoming pregnant, 84%, did not belong to the health system, although 16% expressed working in it. There was a higher percentage of multiparous than primiparous women that had started taking folic acid at the right time. Most of the women monitored their pregnancy in the Public health system, 88.9%. With regard to pregnancy planning, 92.6% said they had done so. Spontaneous conception accounted for 82.7% of cases. Finally, 40.7% and 33.3% stated that the midwife and gynaecologist, respectively, were the professionals who recommended folic supplementation before pregnancy.
Of all women who started taking folic acid during the first trimester (n=224), a high percentage had Spanish nationality (90.6%). The highest percentage of women who began taking the supplement later corresponded to those who claimed to have vocational training or only completed obligatory secondary education (28.1% and 27.7% respectively). 52.5% were employed women and 94.2% belonged to no health-care system. Primiparous began later folic acid intake (51.8%) than multiparous (48.2%). 94.2% of this group of women stated that they monitored their pregnancy in the Public health system. In terms of pregnancy planning, 67% reported having planned the pregnancy, even though they started taking the supplement later. 98.7% of the pregnancies of this group of women were natural. Finally, 55.8% and 31.7% said that the midwife and the primary care physician, respectively, recommended the start of taking folic acid in the first trimester.
By evaluating the time when folic acid intake began with various study parameters, it was calculated that women who were more likely to have an adequate start of folic acid intake were those who were over 33 years of age (OR=2.5; p<0.001), not unemployed (OR=3.35; p<0.001), with vocational training (OR=6.94; p<0.001), those who had a high school diploma (OR=4.80; p<0.001) and university degree (OR=13.01; p<0.001). Considering the sector in which they worked, the health-care system partipants (OR=3.10; p=0.005) have shown the greatest tendency to start taking folic acid at the recommended time. Pregnancy planning establishes a statistically significant relationship with the adequate initiation of folic acid intake (OR=6.17; p<0.001). To conclude, those who have become pregnant through ART have shown a greater probability of initiating folate intake prior to conception (OR=15.39; p<0.001).
Discontinuation of folic acid intake
Of all women surveyed, 80% (244) finished intake of the supplement following the latest standarized recommendations, compared to 20% (61) who stopped it during the second trimester. All the outcome of discontinuation of folic acid intake is shown in Figure 2 Of all the women who finished the intake at the recommended time (n=244), 32.4% had vocational training studies and 59.9% were active female employers. 90.6% did not belong to the health-care system, while 9.4% were health sector workers in it. 55.3% of those who said they had finished their supplementation did not exceed 33 years of age. A higher percentage of nuliparous women (54.5%) expressed having finished taking folic acid at the ideal time. 91.8% of this group of women had had their pregnancy monitored in the Public health system. With regard to pregnancy planning, 75.8% confirmed that they had planned it. Spontaneous conception accounted for 93.9% of cases. Finally, 55.3% and 23% stated that the midwife and the primary care physician, respectively, were the professionals who recommended the intake of folic acid up to the time of delivery.
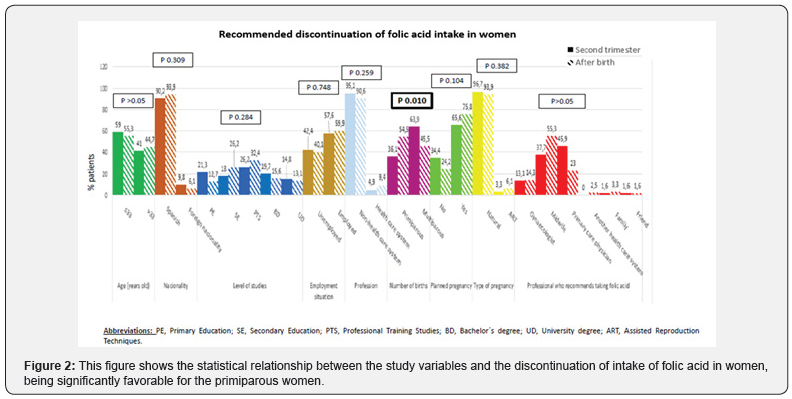
Of the women who finished taking folic acid during the second trimester (n=61), a 26.2% of them corresponded to those who reported having vocational training. 57.6% corresponded to active female workers, of all active female workers, 95.1% worked in non-health system. As for the age of these women, most of them were under 33 years of age (59%). The multiparous women accounted for 63.9%. 96.7% of this group of women stated that they had monitored their pregnancy in the Public health system. Moreover, a 65.6% had planned their pregnancy and 96.7% of all pregnancies were due to spontaneous conception. Finally, 45.9% and 37.7% confirmed that the primary care physician and the midwife, respectively, recommended the taking of folic acid until the second trimester.
The time of completion of folic acid intake was analyzed with the same study parameters previously assessed, and it was concluded that those who had just had their first child (OR=2.12; p<0.010) are more likely to complete the intake at the appropriate time (after childbirth).
Level of knowledge about folic acid
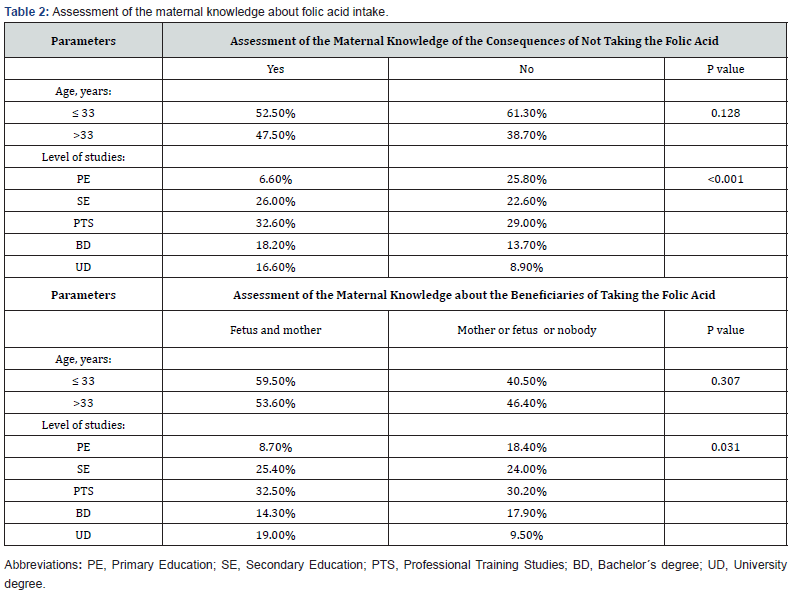
In relation to maternal knowledge about the consumption of folic acid, 59.3% (181) claimed to have an adequate level of knowledge related with the functions of folic acid, some of the consequences of not taking it and the most benefits of the intake. Of all the women who demonstrated an adequate level of knowledge (n=181), 32.6% claimed to have vocational training. Finally, the women with the most knowledge in this area did not exceed 33 years of age (52.5%). Moreover, all the women who expressed no knowledge about folate supplementation (n=124), 29% had vocational training, and 61.3% did not exceed 33 years of age.
Of the postpartum women who considered that they had an adequate level of knowledge about folic acid (n=181), only 18% (33) expressed knowing some consequences of not taking the recommended supplementation.
It should be mentioned that women who ratified knowing the consequences of not taking folic supplementation (n=33), 27.3% had either primary or secondary studies, and 60.6% did not exceed 33 years of age. Regardless of the level of knowledge they had about folic acid or some of consequences of not taking it, and though they knew the benefits of the vitamin supplement, only 41.3% (126) were able to define the true benefits, mother and child, and the highest percentage all of them (32.5%) refer to those with vocational training studies. The statistical analysis of the relationship between some of the parameters previously studied with the level of maternal knowledge, the consequences of not taking folate and the ability to identify the benefits of such taking, showed that the women who are most likely to identify the beneficiaries are those with a university degree (OR=4.23; p=0.031), who have completed vocational training (OR=2.28; p=0.031) and who have completed secondary education (OR=2.23; p=0.031). The outcome is shown in Table 2.
Recommended start and finish of folic acid intake in periconceptional period
Following this and concluding the description and analysis of all the results, the categories of the parameters that refer to the period in which women take folic acid, “start and finish time of taking folic acid”, have been grouped in two, shown in Figure 3. Of all the women in our sample (n=305), only 22.6% (69) of them took the folic acid from preconception to week 12 of pregnancy. Of all the women who took folic acid in the period discussed above (n=69), most of them (58%) exceeded 33 years, all had Spanish nationality and 42% said they had vocational training. 80.9% of these women were employed or self-employed and 85.5% worked in non-health sectors. 92.8% had planned the pregnancy, and 82.6% had not used ART.
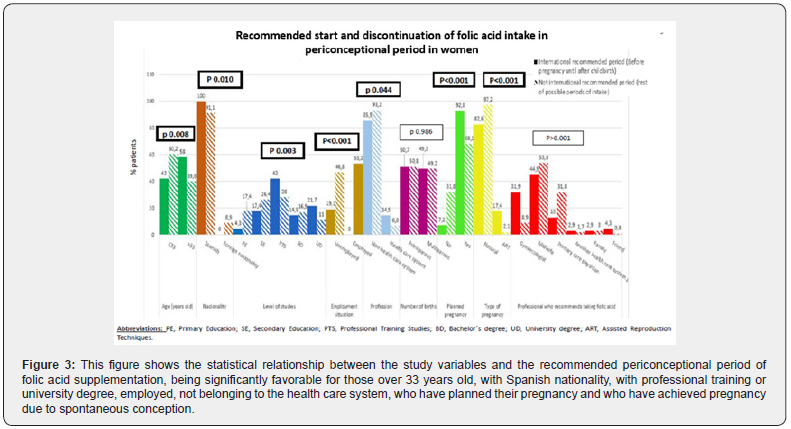
Of the population of women who have not taken the supplement as recommended internationally (n=236), 60.2% did not exceed 33 years of age. 91.1% had Spanish nationality and 28% reported having vocational training. 53.2% of these women expressed that they were employed and 93.2% were not in the health-care system. 68.2% had planned pregnancy and 97.9% did not use ART.
It has been verified if there is a relationship between the adequate period of suplementation, and several variables already studied, it has been obtained that they have greater likelihood of taking folic acid in women older than 33 years (OR=2.08, p=0.008). Taking into account the level of studies, it is university students (OR=7.88, p=0.003) who are more likely to take folic acid in the recommended period. On the other hand, it must be borne in mind that the women with the greatest expectation to take the named vitamin correctly are the employees or self-employed (OR=3.72, p<0.001) and those belonging to the health sector (OR=2.33; p=0.44). Special mention must be made of pregnancy planning, since pregnancy planning is statistically related to a correct intake of folic acid (OR=5.96, p<0.001) probably because they have been advised by a health professional to take folic acid. Finally, it is also the women who achieved their pregnancy through ART who are more likely to have adequate supplementation (OR=9.73, p<0.001).
Discussion
There is scientific evidence of the association between the use of folic acid for the prevention of neural tube defects. Jou and colleagues [23] investigated 275 women in Taiwan in 2010, and although 90% of them knew the importance of folic acid supplementation, only 15.6% took it preconceptionally. Similar studies were carried out in 2011 in Turkey and 2012 in Beirut on populations exceeding 500 women, by Baykan et al. [24] and by Nasr Hage et al. [25] respectively, demonstrating in both that a low percentage of women took the vitamin preconceptionally, (12.2% and 24.7% respectively) such as in our study because of failure to advise women to take folic acid.
Rodríguez et al. [26] in 2013 carried out a study in which they also recorded a low incidence of pre-conceptional folic supplementation (18.8%). In 2017, Jihyun et al. [13] studied 439 women in Korea, with the same conclusion as previous studies; only 26.4% began taking folic acid at the right time. Recently, in 2018, Teixeira et al. [27] have carried out a research in New Zealand to find out what folic acid intake is used in the periconceptional period and with what factors it could be related. Of all the women surveyed (n=6822), 92% had not taken such supplementation in the recommended period, considering the recommended period from the month prior to conception to 12 weeks of pregnancy. In our study, the percentage of women who began folic acid such as in the internationally recommended moment, is similar to the studies referred previosuly, 26.6% of cases.
One of the novel contributions of our research, is that it takes into account the percentage of women who finish taking folic acid at the recommended time until the end of pregnancy, rising that percentage to 80%.
This research identifies that 22.6% women have made an adequate intake of folic acid in the recommended period, but the period recommended in our study for taking this vitamin is different from that considered in the 2018 study referred to above. In order to establish this period, from one month before conception to after childbirth, some studies inform about the multiple benefits of continuing the intake of folic acid up to childbirth, although there is some controversy [28].
In our study, women most likely to take the supplement adequately are those who are over 33 years old, with university degree, employed, who belong to the health- care system, those with planned pregnancy and who manage to become pregnant through ART. Another interesting aspect of this article is the mention of the level of knowledge of women about the functions of folic acid, the consequences of not taking it and the most benefits of the intake. 59,3% (181) claimed to have an adequate level of knowledge about folic acid, 18% could identify some of the consequences of not taking it and taking into account the whole sample again (n=305), 41.3% described the target women of the benefits of such supplementation. In this study, it has been concluded that having university degree is related to the level of knowledge about the consequences of not taking the vitamin.
The study had several limitations, among which are that in certain categories of dependent variables it has not been possible to collect data, for example in relation to the percentage of foreign women who start taking folic acid before pregnancy. Finally, the recruitment has only been carried out in the Public health system, therefore this did not capture data from Private health system, where the number of births is increasing in our country.
Conclusion
Our findings demonstrate that there is a significant association between various characteristics of women with folic acid intake at the most recommended time, as well as with the level of maternal knowledge about its implications. Gynaecologists, midwives and primary care physicians could use this information to guide their clinical practice when recommending folic acid in women who are at risk or planning pregnancy. Our results have confirmed previous research that many women do not take folic acid in the periconceptional period.
Compliance with Ethical Standards
All persons listed as authors have given their approval for the submission of the paper. Authors declare that we do not have any financial support or relationships that may supose conflict of interest. The information collected in this research has been obtained exclusively from human participants with the previous acceptance of these through informed consent. No animals were involved in this study.
References
- Iglesias VL, Abajo LlS, Serrat ON, Arija VV (2015)Estado periconcepcional de ácidofólico: revisiónsobresurelevancia para la salud de la madre y de la descendencia. Relevancia del estadopericoncepcional de ácidofólicosobre el neurodesarrollo. Rev EspNutrComunitaria 21(3): 38-44.
- De‐Regil LM, Fernández‐Gaxiola AC, Dowswell T, Peña‐Rosas JP (2010)Effects and safety of periconceptional folate supplementation for preventing birth defects. Cochrane Database Syst Rev 6(10): CD007950.
- Linhares AO, Cesar JA (2017)Suplementação com ácido fólico entre gestantes no extremo Sul do Brasil: prevalência e fatores associados. Ciência & Saúde Coletiva22(2):535-542.
- Crider KS, Bailey LB, Berry RJ(2011)Folic acid food fortification-its history, effect, concerns, and future directions. Nutrients3(3):370-384.
- Denny KJ, Jeanes A, Fathe K, Finnell RH, Taylor SM, et al (2013)Neural tube defects, folate, and immune modulation.
Birth Defects Res A Clin Mol Teratol 97(9):602-609. - Greenberg JA, Bell SJ, Guan Y, Yu Y-H (2011) Folic acid supplementation and pregnancy: more than just neural tube defect prevention. Rev Obstet Gynecol4(2):52-59.
- Fonseca EBd, Raskin S, Zugaib M (2013) Folic acid for the prevention of neural tube defects. Revista Brasileira de Ginecologia e Obstetricia35(7):287-289.
- Peake JN, Copp AJ, Shawe J (2013)Knowledge and periconceptional use of folic acid for the prevention of neural tube defects in ethnic communities in the United Kingdom: Systematic review and meta-analysis. Birth Defects Res A Clin Mol Teratol 97(7):444-451.
- Wallingford JB, Niswander LA, Shaw GM, Finnell RH (2013)The continuing challenge of understanding, preventing, and treating neural tube defects. Science339(6123):1222002.
- Czeizel AE, Dudás I, Vereczkey A, Bánhidy F (2013) Folate deficiency and folic acid supplementation: the prevention of neural-tube defects and congenital heart defects. Nutrients 5(11):4760-4775.
- De‐Regil LM, Peña‐Rosas JP, Fernández‐Gaxiola AC, Rayco‐Solon P (2015) Effects and safety of periconceptional oral folate supplementation for preventing birth defects. Cochrane Database Syst Rev 12: CD007950.
- Moussa HN, Nasab SH, Haidar ZA, Blackwell SC, Sibai BM, et al. (2016)Folic acid supplementation: what is new? Fetal, obstetric, long-term benefits and risks. Future Sci OA2(2): FSO116.
- Kim J, Yon M, Kim C-I, Lee Y, Moon G-I, et al. (2017)Preconceptional use of folic acid and knowledge about folic acid among low-income pregnant women in Korea. Nutr Res Pract11(3):240-246.
- Blencowe H, Cousens S, Modell B, Lawn J (2010)Folic acid to reduce neonatal mortality from neural tube disorders.
Int J Epidemiol 39(suppl_1): i110-i121. - SACN (2017)Update on folic acid.
- Gomes S, Lopes C, Pinto E (2015)Folate and folic acid in the periconceptional period: recommendations from official health organizations in thirty-six countries worldwide and WHO. Public Health Nutr 19(1):176-189.
- WHO (2014) Daily administration of iron and folic acid supplements in pregnancy.
- Ministerio de Sanidad (2014) Guía de práctica clínica de atención en el embarazo y puerperio.
- Wehby G, Murray J (2010)Folic acid and orofacial clefts: a review of the evidence. Oral Dis 16(1):11-19.
- Wilson RD, Wilson RD, Audibert F, Brock J-A, Carroll J, et al. (2015)Pre-conception folic acid and multivitamin supplementation for the primary and secondary prevention of neural tube defects and other folic acid-sensitive congenital anomalies. J Obstet Gynaecol Can 37(6):534-549.
- Peña‐Rosas JP, De‐Regil LM, Dowswell T, Viteri FE (2012)Daily oral iron supplementation during pregnancy.
Cochrane Database Syst Rev 12: CD004736. - Field MS, Stover PJ (2018) Safety of folic acid. Ann N Y Acad Sci 1414(1):59-71.
- Jou H-J, Hsu IP, Liu C-Y, Chung S-H, Chen S-M, et al. (2010)Awareness and use of folic acid among pregnant women in taipei. Taiwan J Obstet Gynecol 49(3):306-310.
- Baykan Z, Öztürk A, Poyrazoğlu S, Gün İ (2011)Awareness, knowledge, and use of folic acid among women: a study from Turkey. Arch Gynecol Obstet 283(6):1249-1253.
- Nasr Hage C, Jalloul M, Sabbah M, Adib SM (2012)Awareness and intake of folic acid for the prevention of neural tube defects among lebanese women of childbearing age. Matern Child Health J 16(1):258-265.
- Rodríguez Dominguez PL, Collazo Cantero I (2013)Embarazo y uso del ácido fólico como prevención de los defectos del tubo neural. Revista Médica Electrónica35(2):105-113.
- Teixeira JA, Castro TG, Wall CR, Marchioni DM, Berry S, et al. (2018) Determinants of folic acid supplement use outside national recommendations for pregnant women: results from the Growing Up in New Zealand cohort study. Public Health Nutr 21(12):2183-2192.
- Asadi-Pooya AA (2015)High dose folic acid supplementation in women with epilepsy: Are we sure it is safe? Seizure 27:51-53.






























