Monochorionic Pseudomonoamniotic Twin Pregnancy Revealing Fetal Demise. A Unique Case
Sotiriou Sotirios1*, Koukoura Ourania1, Sofoudis Chrisostomos2, Zacharos Nikolaos Marios3, Kailas Pangiotis3, Daponte Alexandros1 and Garas Antonios1
1Department of Obstetrics and Gynecology, University Hospital of Larissa, Greece
2Department of Obstetrics and Gynecology, Konstantopoulio General Hospital, Greece
3Larisa Medical School, Univesrity of Thessaly, Greece
Submission: September 10, 2020; Published: September 14, 2020
*Corresponding author: Sotiriou Sotirios, Department of Obstetrics and Gynecology, University Hospital of Larissa, Greece
How to cite this article: Sotiriou S, Koukoura O, Sofoudis C, Zacharos N M, et al. Monochorionic Pseudomonoamniotic Twin Pregnancy Revealing Fetal Demise. A Unique Case. J Gynecol Women’s Health. 2020: 19(5): 556023. DOI 10.19080/JGWH.2020.19.556023
Abstarct
Pseudoamniotic twin pregnancy represents a rare entity throughout current bibliography. It occurs with an incidence less than 1% of monozygotic pregnancies revealing a significant mortality rate. The disruption of the partitioning membrane in a monoamniotic twin pregnancy consists the performance and function of pseudoamniotic twin gestation. Cord entanglement depicts the most common cause of perinatal mortality in monoamniotic twin pregnancy. Many conducted studies reported incidence up to 70% concerning cord entanglement with mortality rate up to 50% in monoamniotic twins respectively.
Keywords:
Monochorionic twin pregnancy; Pseudomonoamniotic twin pregnancy; Cord entanglement
Introduction
Twin pregnancy consists presence of fetal co-existence inside the uterine cavity. Usually, represents fertilization of two eggs from two sperms (dizygotic twins), or fertilization of one egg, separation of the gamete and formation of two embryos (Monozygotic Twins) [1]. All conducted studies from current bibliography estimate incidence of twin pregnancy about 2% of all other pregnancies [2]. This discrepancy not only is strongly associated to an increased risk of prematurity, but also is depending on the additional risks of chorionity. Monochorionic twin pregnancies are susceptible to additional morbidity due to potential for anastomotic placental vessels and resultant Twin-Twin Transfusion Syndrome (TTTS) [3]. Monochorionic-Monoamniotic pregnancies, during ultra-sonographic formation depict lack of dividing membrane, resulting in cord entanglement.
Percentage of cord entanglement estimates about 70% of all twin pregnancies, leading to an increased rate of intrauterine fetal demise. In extremely rare cases in current bibliography, the dividing membrane in a monochorionic twin gestation can rupture ad create a functional Monochorionic-Monoamniotic, or Pseudomonoamniotic pregnancy [4].
Pseudomonoamniotic Twins, as rare ultra-sonographic entity usually express following characteristics:
a)no dividing membrane during two ultrasound examinations
b)same sex twins
c)normal amniotic fluid volume and
d)unrestricted fetal movement.
Case
We present a case of a 40-year-old patient (G3, P2) admitted at our Department, presented with a spontaneous twin pregnancy. Prenatal monitoring with ultrasound examination confirmed a monochorionic twin pregnancy (Figure 1). Ultra sonographic follow up was settled every 2 weeks, in order to diagnose potential MCDA complications (Monochorionic Diamniotic Twins). Ultra sonographic evaluation during 14th week of gestation confirmed the existence of the diving membrane, sign of Monochorionic-Diamniotic pregnancies (Figure 2).


Ultra sonographic scan during 16th week of gestation revealed normal growth for both embryos, without visualization of the diving membrane. Entanglement of the umbilical cords (Figure 3). Diagnosis of fetal demise during routine ultrasound during 29th week of gestation without any previous complications concerning fetal growth or Doppler assessment. Weekly ultrasonography performance of the other embryo followed by measurement of MCA (Middle Cerebral Artery) maximum velocity index as predictor rate of fetal anemia. MCA v max during 30th week of gestation above 95th centile

At 31th week of gestation and after administration of steroid agents concerning fetal lung maturity, patient underwent caesarian section and gave birth of health boy maximum weight of 1900gr. During caesarian section revealed umbilical cords entanglement, presenting evidence of knotting, indicating prenatal disruption of the diving membrane (Figure 4). Neonatal monitoring with serial ultrasound cranial scans and an MRI 4 weeks after delivery did not reveal signs of cerebral hemorrhage.
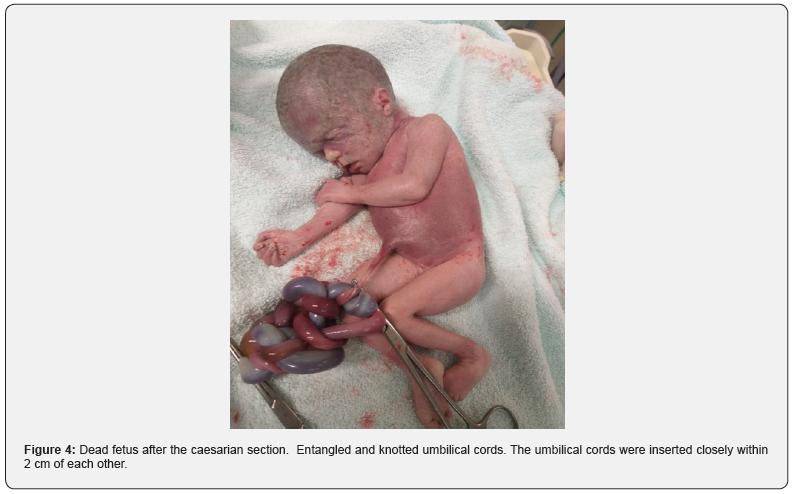
Histopathologic evaluation confirmed presence of monochorionic diamniotic placenta, followed by a diving membrane between the umbilical cords insertions. Assiduous pathologic and autopsy reports, attributed cause of death of the second twin to entanglement of the umbilical cords, leading to thrombosis of the second twin’s umbilical vessels.
Discussion
Monochorionic pseudomonoamniotic twins represent a very rare entity throughout current bibliography.
Many conducted studies revealed reports of spontaneous and iatrogenic cases of a pseudomonoamniotic twin gestational sac [5]. Monochorionic twin pregnancies are often characterized as high risk pregnancies. Apart elevated prenatal and perinatal mortality rate, monochorionic twin gestations can lead to severe fetal complications.
TTTS (Twin-to-Twin Transfusion Syndrome), TAPS (Twin Anemia Polycythemia Sequence) and TRAP (Twin reversed arterial perfusion) consist the most representative fetal abnormalities [6]. In rare cases of pseudomonoamniotic twins, like our case, cord entanglement is considered the most important causative factor [7]. Incidence of monochorionic twins and correlation with severe congenital abnormalities estimated two or three times more likely, comparing with other gestations [8]. IUGR (Intrauterine Growth Restriction) and SGA (Small for Gestation), often presented in monochorionic twin gestations, are strongly accompanied with fetal hypoxia [9].
Focusing on pathophysiologic evaluation, an impediment in the growth of one twin greatly impacts the well-being of the other. Shared fetal circulation, consists in many cases the pathologic etiology of many complications [10]. Monitoring monochorionic twin fetuses, the deceased fetus may draw blood from living fetus (acute transfusion), associating with severe cerebral injury, due to decreased cerebral blood circulation.
Depending on the pathophysiologic pathways of the monochorionic twin gestations, in our case the surviving fetus was born prematurely in order to avoid severe fetal complications. Ultimate goal of our case consists proper diagnosis and treatment of such cases. Assiduous assessment of the partitioning membrane at each ultrasound monitoring in every monochorionic diamniotic twin gestation, along with cord entanglement depiction, reflect proper recommendations of thorough diagnosis.
Disclosure of Interest
All authors declare any financial interest with respect to this manuscript.
Conclusion
Monochorionic pseudomonoamniotic twins reflect rare entities with severe fetal abnormalities. Our case, first described in Greek scientific literature, was properly diagnosed and treated. Ultimate goal remains proper prenatal monitoring, maternal and fetal quality of life respectively.
References
- Liu LY, Zafman KB, Fox NS (2020) The Association between Gestational Weight Gain in Each Trimester and Pregnancy Outcomes in Twin Pregnancies. Am J Perinatol.
- Syngelaki A, Cimpoca B, Litwinska E, Akolekar R, Nicolaides KH, et al. (2019) Diagnosis of fetal defects in twin pregnancies at routine 11-13-week ultrasound examination. Obstet Gynecol Sci62(6):404-410.
- Murgano D, Khalil A, Prefumo F,MieghemTV, Rizzo G, et al. (2020) Outcome of twin-to-twin transfusion syndrome in monochorionic monoamniotic twin pregnancy: systematic review and meta-analysis. Ultrasound Obstet Gynecol55(3):310-317.
- Patil AS, Martin J, Tsukahara K, Skljarevski A, Miller K, et al. (2015) Pseudomonoamniotic Pregnancy: Case Report and Review of Etiologic Considerations. Fetal Pediatr Pathol34(6):413-421.
- Eddib A, Rodgers B, Lawler J, J Yeh (2006) Monochorionic pseudomonoamniotic twin pregnancy with fetal demise of one twin and development of maternal consumptive coagulopathy. Ultrasound Obstet Gynecol28(5):736-737.
- Bamberg C, Hecher K (2019) Update on twin-to-twin transfusion syndrome. Best Pract Res Clin Obstet Gynaecol58:55-65.
- Aisenbrey GA, Catanzarite VA, Hurley TJ, Spiegel JH, Schrimmer DB, et al. (1995) Monoamniotic and pseudomonoamniotic twins: sonographic diagnosis, detection of cord entanglement, and obstetric management. Obstet Gynecol86(2):218-222.
- Townsend R, D'Antonio F, Sileo FG,H KumbayH, Thilaganathan B, et al. (2019) Perinatal outcome of monochorionic twin pregnancy complicated by selective fetal growth restriction according to management: systematic review and meta-analysis. Ultrasound Obstet Gynecol53(1):36-46.
- Bartha JL, Duyos I, de la Calle M, HerreroB, Rodriguez R, et al. (2019) Severe fetal anemia after umbilical cord occlusion leading to severe neurological injury in monochorionic twins. J Matern Fetal Neonatal Med11:1-3.
- Liao TB, Nomura RM, Liao AW, Francisco RPV, Zugaib M, et al. (2014) Fetal venous circulation in monochorionic twin preganncies with placental insufficiency: prediction of academia at birth or intrauterine fetal death. Ultrasound Obstet Gynecol43(4):426-431.






























