Effects of Antenatal Care (ANC) on Institutional Delivery Among Women Living in Low-Income Housing in Delhi, National Capital Region (NCR)
Aditi Puri* and Peter Nwakeze
Monroe College, King Graduate School, School of Allied Health - Masters in Public Health, USA
Submission: August 20, 2020; Published: August 27, 2020
*Corresponding author: Aditi Puri, Monroe College, King Graduate School, School of Allied Health - Masters in Public Health, USA
How to cite this article: Aditi P, Peter N. Effects of Antenatal Care (ANC) on Institutional Delivery Among Women Living in Low-Income Housing in Delhi, National Capital Region (NCR). J Gynecol Women’s Health. 2020: 19(4): 556019. DOI: 10.19080/JGWH.2020.19.556019
Abstract
Background: Access to health care services during pregnancy, childbirth and also postpartum are important for the overall well-being and survival of mother and child.
Methods and ObjectiveA cross-sectional study design was utilized to study the impact of ANC utilization on institutional delivery among urban poor women living in low-income housing in Delhi.
Results:The study findings emphasized that women who accessed ANC in the 1st trimester were more likely to deliver at an institution (91%) compared to those who used services in the 2nd/3rd trimester (79%). Moreover, 21% of those who accessed ANC in the 2nd/3rd trimester delivered at home compared to 9% who accessed ANC in the 1st trimester (chi-square= 8.120, p=.017). Regarding place of delivery, this study found those who accessed ANC at a government (90%) or a private hospital (90%) delivered at an institution. Whereas 76% of those who accessed ANC at a NGO clinic delivered at an institution. Most importantly, 24% of those who accessed ANC at a NGO clinic delivered at home compared to women who accessed ANC at a government (10%) or a private hospital (10%) (chi-square=19.983, p=.001).
Conclusion: ANC utilization and institutional delivery have increased significantly among women in low-income housing in Delhi. Home delivery remains high among women who utilize ANC services in the 2nd/3rd trimester (21%) and at NGO clinics (24%). Strengthening the health system is essential for improving access to ANC services and institutional delivery among underprivileged urban women in Delhi.
Keywords:Antenatal care; Home delivery; Institutional deliver
Introduction
Although the Maternal Mortality Ratio (MMR) is declining in India, it is still high by global standards. MMR was estimated at 482.1 in 1990, 416.7 in 2000 and 247.6 in 2015 compared to the global estimates of 281.5 in 1990 and 195.7 in 2015 [1]. Of the Sustainable Development Goals (SDG), the SDG 3.1 aims to reduce maternal mortality to less than 70 per 100,000 (SDG, 2019) [2]. To achieve this goal, the Global Burden of Disease (GBD) report suggests that 91% of pregnant women should access at least one antenatal care visit (ANC) and efforts should be made to increase 4 ANC visits to 78%, in-facility delivery to 81%, and skilled birth attendance (SBA) to 87% [1]. In India, according to National Family Health Survey-4 (NFHS-4), the proportion of women age 15-49 years old who received ANC has increased from 77% in 2005-06 to 84% in 2015-16. The first ANC visit, during the first trimester increased from 44% in 2005-06 to 59% in 2015-16. During these visits, a greater proportion of women had their weight and blood pressure measured (91% and 89% respectively), blood and urine sample taken (87% and 88% respectively), and abdomen examined (89%). Thirty percent consumed Iron and Folic Acid (IFA) tablets for at least 100 days, and 18% used intestinal parasitic drugs. A marked increase in institutional deliveries, up from 39% in 2005-2006 to 79% in 2015-2016, was noted [3]. Access to health care services during pregnancy, childbirth and also postpartum are important for the overall well-being and survival of mother and child. Screening for complications during ANC can reduce risks for mothers and infants. Delivery at an institution, by a skilled medical provider can reduce risks of complications and infections during delivery [3].
ANC and Institutional Delivery
The findings of a meta-analysis by Fekadu et al. [4] suggested that women who used antenatal services at least once or more were 4 times more likely to deliver at an institution. Additionally, women who used 4 or more antenatal visits were 4.38 times more likely to deliver at an institution in comparison to women who had fewer visits. These women may have a better understanding of benefits associated with institutional delivery, hence would be more inclined to use health services subsequently [4]. Another community-based, cross-sectional study found mothers who accessed ANC services were 2 times more likely to deliver at an institution [5]. Demographic Health Survey (DHS) data from Bangladesh indicated that an increase in number of ANC visits led to a subsequent increase in use of skilled birth attendants (SBA) and institutional delivery [6]. Studies show that several factors positively influence utilization of ANC such as, mother’s age, mother’s and husband’s level of education, household wealth quintile, working status of a woman, health insurance enrollment, religion, and woman’s decision-making autonomy [7,8]. Tarkegan et al. [8] found that women with higher education were more likely to utilize ANC and SBA. Those who used ANC services were more likely to use birth attendants. Another study conducted in six South East Asian countries found that various components of ANC (tetanus injection, height, weight, blood pressure measurement, blood and urine tests, breastfeeding counselling and information about pregnancy complications) were strongly associated with institutional delivery. They emphasized the significance of improving quality of ANC to promote institutional delivery [9]. Dixit et al. [10] analyzed National Family Health Survey-IV to explore the relationship between ANC and institutional delivery. Their findings showed that women who used ANC once or twice had a 6.6% higher chance of delivering at an institution [10].
ANC Utilization in India
The health infrastructure in India is relatively strong, but healthcare resources are inequitably distributed between rich and poor [11]. Prusty et al. [12] found a positive association between utilization of maternal healthcare services and economic conditions. Women in the richest wealth quintile were 1.8 times more likely to have full ANC; 4 times more likely to delivery safely in an institution or at home with a trained provider such as doctor, nurse, Auxiliary Nurse Midwife (ANM), or Lady Health Visitor; and 1.7 times more likely to have PNC compared to women from the poorest wealth quintile. A study conducted in Punjab urban slums found that 59% of poor women had completed 3 ANC visits, 49% delivered at home, 81% of these deliveries were conducted by a trained dai (midwife) while 19% delivered without SBA. Janani Suraksha Yojna (JSY) is an ambitious cash transfer scheme launched by the Indian government to provide cash incentives to promote institutional delivery [13]. Approximately 89% of those who were eligible for JSY cash benefits did not receive them; 49% revealed that it was due to non-filing of the JSY card by the ANM [11]. In addition, the trained Social Health Activists (ASHA) have been envisioned by the government to receive performancebased incentives for motivating women to receive MCH services under the Reproductive and Child Health Program [13]. In a study conducted to evaluate the maternal healthcare utilization among women in Delhi slums, the authors found that awareness of and accessibility to a well-equipped modern healthcare facility can increase health service utilization. In their study, 76% received ANC from a hospital or a peripheral health post. Sixty-eight percent of the deliveries were conducted by a doctor/nurse at a hospital, and 66.6% of the home deliveries were conducted by a dai. It may not be possible to establish a well-equipped health facility near every slum in the Delhi area, but effort should be made to increase awareness about the benefits of utilizing a modern healthcare facility within the vicinity of the slum [14]. Gupta et al. [15] found that government hospitals were an important source of ANC services for women living in Bhopal urban slums; in fact 90% of women accessed services at a government hospital and 6% at a private hospital. However, 86.49% of the deliveries were performed at home by an untrained dai (63.33%) [15]. In contrast, 93.9% of women in Aurangabad urban slums delivered at a facility, and 67.6% had their first antenatal visit in the 1st trimester [16].
A plethora of research shows that ANC services tend to increase institutional delivery [17-22]. A majority of these studies were conducted on the African continent. No studies to our knowledge have explored the relationship between ANC services and institutional delivery in India. The current study will fill gaps in the literature by evaluating the effect of antenatal service utilization on institutional delivery among women living in lowincome housing in Delhi, NCR.
Material and Methods
The setting of this cross-sectional quantitative study was low-income housing communities in Delhi, NCR (Gurugram and Delhi). One hundred and five (105) mothers with children below 3 years of age were recruited from slums and low-income housing located in Delhi, NCR and neighboring villages such as Saraswti Kunj, Neemtala, Wazirabad, Rangpuri padai/Indercamp, Ullawas, Nalapar, Bhanwadi, and Ghata. The participants were recruited from Mother and Child Health (MCH) camps offered by a Sukraya (NGO) or immunization camps at aangan wadi’s (head start programs in Gurugram). The lead investigator trained three (3) interviewers for 3 hours on 2 consecutive days to help administer the survey. The survey questions were taken from 4 peer-reviewed studies and reports [11-15]. The team conducted one-on-one interviews after participants signed an informed consent form. Those who consented were interviewed outside under a tree or in a courtyard. The interviews lasted 30 minutes. The data were collected from April 2 to April 30, 2018. The data were entered in an Excel spreadsheet and transferred to SPSS 26. The data were analyzed using descriptive statistics and chi-square test.
Results
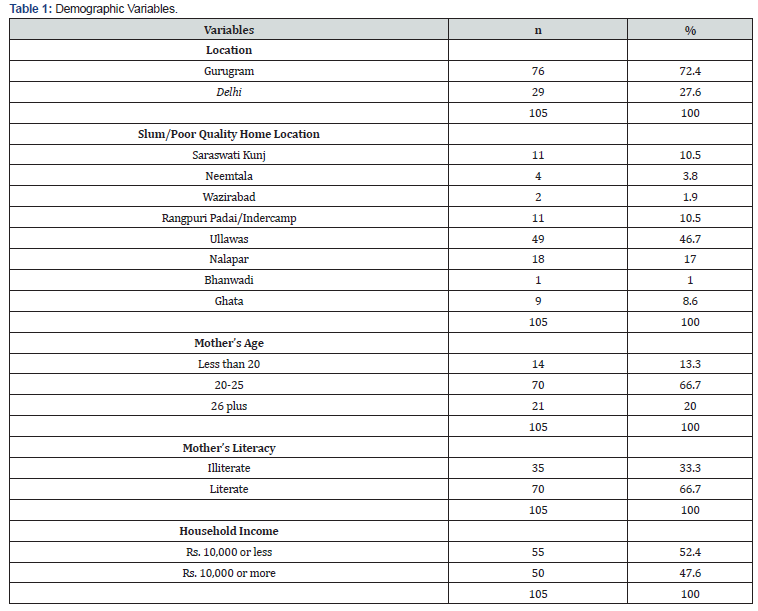
In this study, a majority of the mothers (67%) were between the ages of 20-25 years old and lived in Gurugram (72%) and Delhi (28%). Thirty percent of women had infants between the ages of 8 and 12 months old, and 45% of the infants were firstborn. Seventy-four percent of the mothers lived in a rental home; 52% had less than an INR10,000 household income ($142US per month or $4.70US per day); 67% were literate, and 69% were not working (see Table 1).
In terms of service utilization, 100% of women utilized ANC services, although 57% lived more than 5 km away from a Mother and Child Health (MCH) center. Fifty percent had less than 4 ANC visits; 54% utilized ANC services in the first trimester; 94% received 2 doses of Tetanus Oxide (TT) injection; 48% had >100 Iron and Folic Acid (IFA) tablets during pregnancy; and 76% did not experience any health problems during pregnancy, although 14% experienced some, and 10% experienced serious health problems. Some examples of health problems included: bleeding, hypertension, diabetes, measles, pain, and swelling. Eighty percent were satisfied with ANC; 69% delivered at a government hospital, 14% at home and 17% at a private hospital. Some reasons cited for non-institutional delivery were: convenience of home (3.8%), normal pregnancy (1%), no one to accompany (1%), distance (2.9%) and untimely delivery (9.5%). Among those who delivered at home, 40% were assisted by an untrained person and 60% by a dai. Eighty-three percent delivered vaginally, and 16% had C-sections; 40% stayed less than a day at the hospital post-delivery. Thirty-five percent traveled to the place of delivery by auto rickshaw, 20% by car, and 24% by ambulance or taxi. Only 40% received postnatal care, and 83% were satisfied with PNC. Some examples of postnatal services received were: BCG (95%), Zero polio (94%), breastfeeding advice (80%), and complete immunization (89%). Fifty-one percent of the women indicated receiving less than optimal help from ASHA, whereas 45% received optimal help. Some of the ways in which ASHA assisted included: referral to ANC (45%), helped register for ANC (43%), counselled on ANC (57%), ASHA visits during delivery (33%), counselled regarding child immunization (58%) and breastfeeding advice (60%). It is important to note that only 9% of the women received Janani Suraksha Yojna (JSY) cash benefits (see Table 2&3).


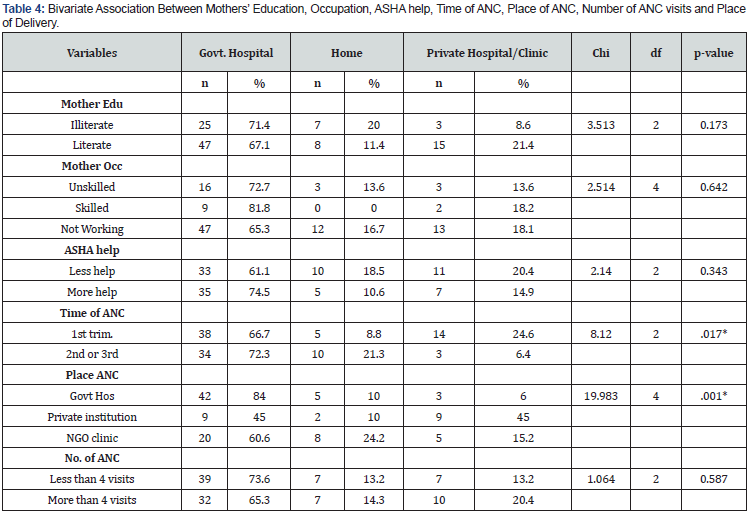
The bivariate analysis indicated that only 2 variables (time of ANC and place of ANC) were significantly associated with place of delivery. The study findings emphasized that women who accessed ANC in the 1st trimester were more likely to deliver at an institution (91%) compared to those who used services in the 2nd/3rd trimester (79%). Moreover, 21% who accessed ANC in the 2nd/3rd trimester delivered at home compared to 9% who accessed ANC in 1st trimester (chi-square= 8.120, p=.017). The place of receiving ANC was also significantly associated with place of delivery. Antenatal services were accessed from multiple locations, such as a government hospital, private hospital and NGO clinic. Those who accessed ANC at a government (90%) or a private hospital (90%) delivered at an institution. Whereas 76% of those who accessed ANC at a NGO clinic delivered at an institution. Most importantly, 24% who accessed ANC at a NGO clinic delivered at home compared to women who accessed ANC at a government (10%) or a private hospital (10%) (chisquare= 19.983, p=.001). In this study, number of ANC visits were not significantly associated with place of delivery (chisquare= 1.064, p-value=.587). Additionally, mother’s education, mother’s occupation and ASHA help were not associated with place of delivery. The significant variables (time of ANC and place of ANC) were no longer significantly associated with place of delivery after they were entered in a logistic regression model (see Table 4).
Discussion
In this study, trimester of first antenatal visit (chi=8.120, p=.017) and place of ANC (chi=19.983, p=.001) were significantly associated with place of delivery. The study findings emphasized that women who accessed ANC in the 1st trimester were more likely to deliver at an institution (91%) compared to those who used services in the 2nd/3rd trimester (79%). Moreover, 21% who accessed ANC in the 2nd/3rd trimester delivered at home compared to 9% who accessed ANC in the 1st trimester (chisquare= 8.120, p=.017). Early access to ANC increased the chance of institutional delivery. In another study conducted in the urban slums of Punjab, only 46% of women used ANC services in the first trimester [11] compared to 54% in this study. Improvement in access to MCH services among poor women could be responsible for these gains. Additionally, satisfaction with the ANC services could have further motivated women to deliver at an institution. It is important to note that 80% of women in this study were satisfied with ANC services. According to Dixit et al, if the content of ANC services fulfills the needs and expectation of the woman, it can further motivate her to deliver at an institution [9]. Perhaps important factors such as level of care, ANC content, and knowledge of delivery complications motivated women to access ANC in 1st trimester and deliver at an institution. An interesting observation in this study was that only 14% of women delivered at home and 86% or 8 out of 10 delivered at an institution; 40% of the home deliveries were performed by an untrained person and 60% by a dai. Some reasons for home delivery included: convenience of home (4%), normal pregnancy (1%), distance from delivery institution (3%), nobody to accompany (1%) and untimely delivery (10%). It seems that efforts focused on increasing intuitional delivery are bearing fruit. Some examples of interventions that appeared to increase institutional delivery included: improved access to ANC services at government/ private hospitals and NGO clinics; assistance from ASHA workers; satisfaction with ANC services; and access to ANC in 1st trimester. However, only 9% of women in this study received the JSY benefits and 45% received optimal services from ASHA workers as compared to less than optimal services (51%). Some ways in which ASHA assisted women included: counselling on ANC (57%), referral (45%) and registration for ANC (43%), ASHA visit during delivery (33%), counselling regarding child immunization (58%) and breastfeeding advice (60%). Twenty-four percent noted that they did not receive any help from ASHA.
Previous studies have not explored the relationship between place of ANC and institutional delivery. This study found a significant association between place of ANC (government hospital, private hospital or NGO clinic) and institutional delivery. In terms of place of delivery, this study found those who accessed ANC at a government (90%) or a private hospital (90%) delivered at an institution. Whereas 76% of those who accessed ANC at an NGO clinic delivered at an institution. Most importantly, 24% who accessed ANC at an NGO clinic delivered at home compared to women who accessed ANC at a government (10%) or a private hospital (10%) (chi-square=19.983, p=.001). Clearly an increase in access to ANC services has increased utilization of institutional delivery among women living in slums/low-income housing. However, home births remain high among those who used ANC services from NGO clinics. Thus, public health endeavors need to focus on marginalized women who depend on NGO clinics for ANC care; these women need to be educated and incentivized to deliver at an institution. In addition, 100% of women in this study had utilized ANC services; 50% had less than 4 visits, whereas 47% had 4 visits or more. Ninety-four percent received 2 TT doses during these visits, and 48% had consumed more than 100 IFA tablets. Dabade et al. [16] in their study in urban slums of Aurangabad, found that 88.9% of women had received 2 doses of TT, but IFA tables were consumed by only 41.7% women. The majority (93%) of the women delivered at an institution, and 1.9% of those who delivered at home were assisted by an untrained person [16]. Findings of this study were mostly similar to Dabade et al. [16] although 9 out of 10 women in their study delivered at an institution compared to 8 out 10 in this study. According to NHS-4 (2015-2016) [3], nationally, 51% of women had 4 ANC visits compared to 47% in this study, WHO recommends at least 4 visits. Fifty-nine percent had their first visit in the 1st trimester [3], compared to 54% in this study. Eighty-nine percent of births were protected by TT injection [3], whereas it was 94% in this study. Eighty-nine percent received services from a skilled provider [3] whereas 100% in this study received ANC services from a skilled provider at a government hospital, private hospital or NGO clinic. Seventy-nine percent of the deliveries were institutional [3], whereas in this study 86% delivered at an institution. The Ministry of Health and Family Welfare (MoHFW) recommends that all postpartum women receive a postnatal check within 24 hours, if they deliver in a facility. Those who deliver outside a facility should receive a check within 12-hours of birth [3]. In this study, an alarming number (40%) stayed less than a day (24 hours) in the hospital after delivery. Only 40% utilized PNC services, but 95% of the infants received the BCG vaccine; 94% received zero polio, and 89% had complete immunization. The authors recommend further strengthening of the mother and child health services in poor urban settings to encourage access to ANC in the first trimester.
Conclusion
Institutional delivery was highest among those who accessed ANC from a government (90%) or a private (90%) hospital. A majority (91%) of those who utilized ANC in the 1st trimester delivered at an institution. However, home delivery remains high among women who utilize ANC services in the 2nd/3rd trimester (21%) and at NGO clinics (24%). Thus, it’s imperative for government, NGOs, private and public health institutions to improve access to quality antenatal services and institutional delivery among poor women in urban settings. Programs such as ASHA and JSY can be further strengthened to improve ANC utilization and institutional delivery among marginalized urban women.
Acknowledgement
The authors thank the Sukaraya (NGO) team for their invaluable support in data collection; a special thanks to Shahnawaz Shahid for providing us an opportunity to work with the Sukaraya team. The authors thank the research librarian Marilyn Reside for editing the manuscript.
A special thanks to my parents Savita Puri and Ravinder Nath Puri for encouraging me to achieve my dreams.
References
- GBD 2015Maternal Mortality Collaborators (2016) Global, regional and national levels of maternal mortality, 1990-2015: a systemic analysis for the Global Burden of Disease Study 2015. The Lancet 388(10053):1175-1812.
- United Nations Development Programme (2020)Goal 3: good health and well-being.
- International Institute for Population Sciences (2020) National Family Health Survey, India.
- Fekadu GA, Kassa GM, Berhe AK, Muche AA, Katiso NA, et al. (2018) The effect of antenatal care on use of institutional delivery service and postnatal care in Ethiopia: a systematic review and meta-analysis. BMC Health Serv 18(1): 577.
- Tekelab T, Yadecha B, Melka AS (2015) Antenatal care and women's decision making power as determinants of institutional delivery in rural area of Western Ethiopia. BMC Res Notes, pp. 2-8.
- Ryan BL, Krishnan RJ, Terry A (2019) Do four or more antenatal care visits increase skilled birth attendant use and institutional delivery in Bangladesh? A propensity-score matched analysis. BMC Public Health 19: 583.
- Dahiru T, Oche OM (2015) Determinants of antenatal care, institutional delivery and postnatal care services utilization in Nigeria. Pan Afr Med J 21: 321.
- Tarekegn SM, Lieberman LS, Giedraitis V (2014) Determinants of maternal health service utilization in Ethiopia: analysis of the 2011 Ethiopian Demographic and Health Survey. BMC Pregnancy Childbirth 14: 161.
- Dixit P, Khan J, Dwivedi LK, Gupta A (2017) Dimensions of antenatal care service and the alacrity of mothers towards institutional delivery in South and South East Asia. Plos One 12(7): e0181793.
- Dixit P, Dwivedi LK, Ram F (2013)Estimating the impact of antenatal care visits on institutional delivery in India: A propensity score matching analysis. Health 5(5): 862-878.
- Phawa P, Sood A (2013)Existing practices and barriers to access of MCH services - a case study of residential urban slums of district Mohali, Punjab, India. Global Journal of Medicine and Public Health 2(4): 1-8.
- Prusty KR, Gouda J, Pradhan MR (2015) Inequalities in utilization of maternal healthcare services in Odisha, India. International Journal of Population Research.
- UNFPA (2009)Concurrent assessment of Janani Suraksha Yogana (JSY) scheme in selected states of India.
- Agarwal P, Singh MM, Garg S (2007) Maternal health-care utilization among women in an urban slum in Delhi. Indian Journal of Community Medicine 32(3).
- Gupta SK, Nandeshwar S (2012) Status of maternal and child health and services utilization patterns in urban slums of Bhopal, India. National Journal of Community Medicine 3(2): 330-332.
- Dabade JK, Dabade SK, Madhekar NS, Khadilkar HA (2013) A study of utilization of maternal health care services in urban slums of Aurangabad City, Maharashtra. Journal of Evolution of Medical and Dental Science 2(51): 9907-9915.
- Adedokun ST, Uthman OA (2019) Women who have not utilized health service for delivery in Nigeria: who are they and where do they live?BMC Pregnancy Childbirth 19.
- Negero MG, Mitike YB, Worku AG, Abota TL (2018) Skilled delivery service utilization and its association with the establishment of women’s health development army in yeky district, south west ethiopia: a multilevel analysis. BMC Res Notes 11(1): 83.
- Assefa M, Fite RO, Taye A, Belachew T (2020) Institutional delivery service use and associated factors among women who delivered during the last 2 years in Dallocha town, SNNPR, Ethiopia. Nursing Open 7(1): 186-194.
- Kasaye HK, Endale ZM, Gudayu TW, Desta MS (2017) Home delivery among antenatal care booked women in their last pregnancy and associated factors: community-based cross sectional study in Debremarkos town, North West Ethiopia, January 2016. BMC Pregnancy Childbirth 17: 225.
- Siyoum M, Astatkie A, Mekonnen S, Bekele G, Taye K, et al. (2018) Home births and its determinants among antenatal care-booked women in public hospitals in Wolata Zone, Southern Ethiopia. Plos One 13(9): e0203609.
- Kasaaw A, Debie A, Geberu M D (2020)Quality of prenatal care and associated factors among pregnant women at a public health faciltiy in Wogera district. Journal of Pregnancy.






























