A Retrospective Analysis of Laparoscopic Outcome in Women with Primary and Secondary Infertility in A Developing Country
Zohra Amin1*, Arzoo Amin2, Wajiha Pervaiz3, Farah Nighat Saani4 and Meher Obaid5
1 TraineeObs/Gyn at Derriford Hospital, Plymouth, Uk (Former Trainee Hayatabad Medial Complex, Peshawar, Pakistan)
2 Post CCT fellow Obs/Gyn, Royal Hospital Surrey, Uk
3 Former Trainee Obs/Gyn at Hayatabad Medical Complex, Peshawar, Pakistan
4 Former Trainee Obs/Gyn at Hayatabad Medical Complex Peshawar, Pakistan
5Associate Professor Obs/Gyn at Hayatabad Medical Complex Peshawar, Pakistan
Submission: March 11, 2020; Published: March 17, 2020
*Corresponding author: Amin Zohra,TraineeObs/Gyn at Derriford Hospital, Plymouth, Uk (Former Trainee Hayatabad Medial Complex, Peshawar, Pakistan)
How to cite this article: Amin Zohra. Retrospective Observational Study for Laparoscopy. J Gynecol Women’s Health. 2020: 18(4): 555993. DOI: 10.19080/JGWH.2020.18.5559893
Abstract
Objectives: To analyse the role of diagnostic laparoscopy and compare the laproscopic findings of primary and secondary infertile cases in a developing country.
Methods: A retrospective analyses of cases done from January 2008 to December 2012 in the Department of Obstetrics and Gynaecology, Hayatabad Medical Complex, Peshawar, Pakistan was done. 874 cases were studied. The data was collected retrospectively and analysed using Microsoft excel, prism 2014 and SPSS version 17. The main outcome criteria were to determine the frequency of primary and secondary infertile cases, along with their different pathological findings”.
Result: Out of 874 cases ,69% (600) had primary and 31% (274) had secondary infertility. Ovarian pathology was the most frequent finding in both, affecting 46.4% (127) secondary and 44.9% (269) primary cases. Polycystic ovaries were more common in primary (18.1%) while adhesions were more common in secondary cases (7.1%). Interestingly normal uterus was found more in primary 81.6% than secondary 78.5%. Fibroid (6.7%) was the major finding in primary infertile women while among secondary cases bulky uterus (6.5%) was the commonest finding followed by adhesions (4.7%). Fallopian tubes were normal in 76.5% primary and 69.7% secondary cases, tortuous tubes being the most frequent finding. Dye test demonstrated tubal blockage to be more common in secondary infertility.
Conclusion: Laparoscopy is an effective diagnostic tool. Anomalies and Polycystic ovaries are more common in primary while adhesions and tubal blockage are more common in secondary cases. Safe delivery measures implementation could reduce infections and its consequences like adhesions and tubal blockage.
Keywords:Infertility; Secondary infertility laproscopic finding; Adhesions; Tubal blockage; Polycystic ovaries
Introduction
Infertility is defined as inability of a couple to conceive after 1 year of unprotected regular intercourse [1]. Infertility can affect a woman’s social and psychological life, leaving her miserable and insecure especially in developing countries like Pakistan [2]. Providing these underprivileged people with the latest medical advancements at an affordable cost should be the mainstay of treatment in this part of the world. Infertility can be caused by multiple factors including ovulatory disorders, tubal diseases, uterine or cervical factors, endometriosis and male factor infertility [3]. The main reasons however, in the developed world are different from those in the developing world. According to World Health Organisation, the major causes on a global basis are pelvic tuberculosis, malnutrition, post abortion and postpartum infections leading to tubal blockade [3].
Evaluation of infertile women includes detailed history and physical examination followed by hormonal assessment and pelvic sonography. Hysterosalpingography (HSG) has been used as a traditional way to assess the uterine cavity and tubes. However, in about half of the patients with normal HSG, pelvic pathologies have been identified [4]. This lead to use of laparoscopy and hysteroscopy especially in patients remaining undiagnosed with the above mentioned investigations. Diagnostic laparoscopy allows direct visualization of reproductive organs which no other imaging techniques provide the same degree of specificity and sensitivity. Laparoscopy also helps in therapeutic manipulations of infertility but its main role however, is diagnostic [5]. Although it has an excellent safety record in hands of well-trained operator yet it is not cost effective and involves hospital stay for at least 24 hours. Moreover, besides anesthesia exposure. The objective of this study was to analyse the role of diagnostic laparoscopy in establishing the cause of infertility and to compare the laparoscopic findings of primary and secondary infertility so as to find any area for improvement of care
Methods
The patients with primary or secondary infertility subjected to laparoscopy from January 2008 to December 2012 in the department of Obstetrics and Gynecology A, Hayatabad Medical Complex, Peshawar, Pakistan were included in this retrospective study. Total 874 cases were done. Institutional Ethics Committee approval was obtained. Data was analyzed using Microsoft excel, prism 2014 and SPSS version 17. The patients having heart diseases, chromosomal disorders, known cases of uterine abnormalities, those with known male factor infertility and unco- operative ones were excluded from the study. Patients with all contraindications as related to procedures of laparoscopy like hernia, tubercular peritonitis with adhesions, large pelvic masses were also excluded from the study.
Result
Total number of patients were 874 with 69% (600) primary cases and 31% (274) having secondary infertility. The patients ranged in 19-40 years of age with maximum number between 21- 30 years (Mean 29.5 years). The duration of infertility was 2-10 years with majority seeking treatment after 2-5 years. Out of the uterine pathologies, fibroids had the highest prevalence and were present in 4.7% (13) secondary and 6.7% (40) primary cases (Table I). Pelvic inflammatory diseases and Endometriosis were more frequent a finding in secondary cases with adhesions in 4.7% secondary (and 3.6% primary) cases. The frequency of congenital anomalies was evidently greater in primary (1.5%) than secondary cases (0.7%). Most frequent anomalies were infantile uterus and uterus di-delphys in primary and rudimentary horn in secondary cases. The most common finding on laparoscopy was ovarian factor affecting 46.4% (127) secondary and 44.9% (269) primary cases. Most common pathology being polycystic ovaries, found in 13.8% secondary and 18.1% primary cases. Ovaries were affected by adhesions more in secondary cases in concordance with higher incidence of PID in secondary cases (Figure 1) (Table I &2).


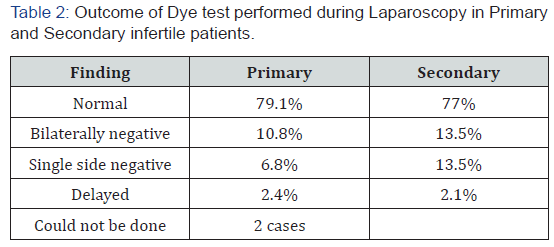
Tubal pathology was found in 30.3% (88) secondary cases and 23.6% (141) in primary cases. Most common being hydro salpinx, affecting almost twice as many secondary cases as primary 17% (46) secondary while 9.3% (56) primary cases. Tubes were affected by adhesions in 6% primary and 10.5% secondary cases. Dye test was bilaterally negative in 10.8% (65) primary and 13.5% (37) secondary cases [6,7].
Discussion
Out of the total 874 cases, the number of patients with primary infertility 674(69%) was almost twice of those who presented with secondary infertility 274(31%). This is in contrary to the findings of Khurshid N 1995 (Pakistan) 5 which showed higher incidence of secondary infertility than primary [8]. Apparently more cases with primary infertility are seeking early medical advice. Female age is an important determinant of fertility. According to American Society of Reproductive Medicine (2012)6 35 years is considered as advanced maternal age. NICE recommendation states that women over 35 years of age should be referred early from primary care for investigation and treatment. In this study the mean presenting age was 29.5 years which has increased in comparison to previous studies conducted in Pakistan [9,10]. which could be because of delayed marriages or delaying conception. Major presenting symptoms in this study were pelvic pain, dyspareunia, irregular cycles or asymptomatic infertility which are in consistence with other studies [3,8- 12]. in both developing and developed countries. The fact that symptomatic patients were frequently diagnosed associated with organic pelvic pathology on diagnostic laparoscopy, emphasizes its importance therein.
Uterus was normal in 78.5% secondary and 81.6% primary infertile patients showing the incidence of uterine pathologies to be higher in secondary cases [13]. These findings are consistent with the study of Boricha YG et al. [5] (India) where 82% primary cases had a normal uterus. Out of the pathologies detected 4.7% were fibroids in secondary compared to a higher incidence of 6.7% in primary. However the incidence of bulky uterus on the other hand was higher in secondary 6.5% then primary cases 4.7%, similar to the findings in study of Gulfreen13 in Rawalpindi, Pakistan. The incidence of myoma in women with unexplained infertility is estimated to be 1-2.4% [14].
There was a very low overall incidence of Endometriosis only 1.1% among secondary and 0.3% of primary cases supporting the presumption that endometriosis is uncommon in Asian women [15-17]. Previous study in this department has shown similar results8but conflicting data has also been reported [9]. A higher incidence of Endometriosis (4.4%) was reported in Africa [18]. The incidence of pathologies was highest in Ovaries being 46.4% in secondary and 44.9% in primary cases. Boricha YG5 Mumbai had the same finding in their study, while Shetty et al. [3] (2013) India and ikechebelu (2011)15 in Nigeria found tubal cause to be the most common. The prevalence of polycystic ovarian disease (PCO) in asymptomatic women is thought to be between 16 and 33% [12]. In this study, polycystic ovaries were found in 18.6% primary and 13.6% secondary cases, showing its more frequent incidence in primary cases in consistence with many other studies [8,9,12].
The fallopian tubes were affected in 23.5% primary and 30.3% secondary cases, similar to the studies of Boricha YG5 and Gulfreen13 where tubal pathology was the finding in only 20% and 10% cases respectively. However, in studies by Khurshid [6]. the tubal factor was the most common cause. In a study done in Nigeria15 60.4% of the cases had a uni/bilateral tubal occlusion. A decline in tubal pathology through the years in our part of the world might possibly be due to decreased incidence of infection and/or timely treatment with antibiotics. Tubal occlusion, peri tubal and peri ovarian adhesions are factors responsible for obstruction in ovum transport. In developed countries as well, the major cause is PID and tubal factors accounts for up to 40% of infertility with diverse etiologies [16]. In Osuga Y’s17study, 31% patients were found to have PID and 5% had Endometriosis. Pelvic-peritoneal adhesions (mostly sequels of prior infections from organisms like Chlamydia Trachomatis and Neisseria Gonorrhoea) constitute the single most common class of tubal pathology responsible for tubal infertility. The cause is anatomical and physiological compromise of tubal functions of ovum pick-up, fertilisation and zygote transport between the ovary and the uterus.3Beaded appearance of the tubes in 3.15% of our primary cases suggest high incidence of Tuberculosis in this part of the world.
Bilateral tubal blockade was however, the finding in only 10.8% primary and 13.5% secondary cases. However dye test could not be done in 2 cases as they were uncooperative. sTubal blockage represents the aftermaths of pelvic infection or surgery. In a previous study [8], conducted in the same department (covering same population) blocked, dilated and tortuous tubes were more frequent in secondary than in primary infertility. A single episode of disease carries up to 10% risk of future tubal factor infertility [18]. Sinawat et al. [19] reported tubal abnormalities in over one fourth of all infertile females while Moore J [16] reported 36.6% bilateral tubal blockade followed by extensive adhesions contributing to infertility and chronic pelvic pain secondary to PID. In Shetty’study tubal blockage was observed in as many as, 18.7% secondary cases [3].
Most sub fertile couples with normal laparoscopic findings (or minimal Endometriosis) conceived within next couple of months. Similar results have been reported in other studies [3]. Unexplained infertility however, may be managed with ovulation induction and/or intrauterine insemination while ART should be considered in couples with advanced maternal age (to buy time) and in those where other options have failed.
Conclusion
Laparoscopy evidently remains the main stay of diagnostic evaluation in modern investigations of infertility. Congenital uterine anomalies and polycystic ovaries remain more common in primary as compared to higher incidence of adhesions (PID), Endometriosis and tubal blockage in secondary cases. The incidence of Pelvic Tuberculosis remains high.
Recommendations
Higher prevalence of PID in secondary cases can have an association with non-sterile conditions of delivery in this part of the world. Propagation of efforts on safe delivery are recommended. High prevalence of pelvic Tuberculosis demands more focus on TB control programs.
Note: Our study is based on
a) An honest approach to natural findings in a developing country with no prejudice and bias in the results.
b) Results compared to other studies on the laparoscopic findings of infertile patients in other developing countries and some developed countries.
c) A duration of 4 years with a large number of patients (874) being considered.
d) An attempt to elucidate the role of Laparoscopy in providing diagnostic evidence in infertility.
e) The limitations of the study are:
f) Retrospective analysis.
g) Hysteroscopic visualisation couldn’t be done.
h) Tubal function couldn’t be assessed.
1) The outcome/success of infertility management in these primary and secondary infertile patients was not considered in this study due to two reasons:
2) In underdeveloped countries, very few patients show up for follow up, hence the success of treatment cannot be assessed.
3) We do not have all latest fertility management options available in our setup, hence patients had to be referred to other infertility centres (with no facilities of integrated care), due to which the outcome could not be assessed in all of them. The study is basically being done on the “laparoscopic findings” in primary and secondary infertile patients and therefore does not relate directly to the operative interventions made in some of these cases.
Acknowledgement
Special thanks to Dr. Mumtaz, Research Supervisor, IREB Committee, PGMI, Peshawar for guidance on proper research protocols. I would also like to thank Dr. Ilyas rafiqi for their help regarding access to department data and previous publications.
Funding
Wholly funded by the authors.
Ethics Approval
Reference No 6128, IREB/Ethics Committee, Post Graduate Medical Institute, Peshawar, Dated: 30/4/2014.
Authors’ Contributions
a) ZA and WP conceived, designed, collected data and did the statistical analysis.
b) AA and FNS has been involved in planning, financial management, compilation of the study and manuscript writing.
MO helped in data retrieval, reviewed and finally approved the manuscript.
References
- Lindsay TJ, Vitrikas KR (2015) Evaluation and treatment of infertility. Am Fam Physician91(5): 308-314.
- worldometers.info
- Shetty S, Shetty H (2013) Diagnostic laparoscopy in infertility-A retrospective study. Int J Biomed Res4(7):343-348.
- Badawi IA, Fluker MR, Bebbington MW (1999) Diagnostic laparoscopy in infertile women with normal hysterosalpingograms. J Reprod Med 44(11): 953-957.
- Boricha YG, Sharma RK (2011) Laparoscopy in 50 infertile couples: prospective study. Int J Med Clin Res2(2):63-66.
- Khurshid N (1995) Prevention and Management of Infertility in: Conference on Reproductive health at CPSP, pp. 88-90.
- Practice Committee of American Society for Reproductive Medicine (2012) Diagnostic evaluation of the infertile female: a committee opinion. Fertil Steril98(2):302-307.
- Naz T, Hassan L, Gulmeen NF, Nighat F, Sultan S, et al. (2009) Laparoscopic evaluation in infertility. J Coll Physicians Surg Pak19(11):704-707.
- Aziz N (2010) Laparoscopic evaluation of female factors in infertility. J Coll Physicians Surg Pak20(10):649-652.
- Talib W, Ikram M, Maimoona H, Saeed M (2007) Infertile female; laparoscopic evaluation. Professional Med J14:562-566.
- Kabadi YM, Harsha B (2016) Hysterolaparoscopy in the Evaluation and Management of Female Infertility. J Obstet Gynaecol India66(Suppl 1):478-481.
- Enda McVeigh (2004) Polycystic ovarian syndrome. In: Baker PN, Leusley DM (eds.), Obstetric and gynaecology: an evidence- based text for Mrocg. Oxford University Press, London, UK, p. 588-593.
- Haider G, Rani S, Talpur S, Zehra N, Munir A, et al. (2010) Laparoscopic evaluation of female infertility. J Ayub Med Coll Abbottabad22(1):136-138.
- Khaula K (2005) Role of diagnostic laparoscopy in evaluation of female subfertility. Serv Inst Med Sci 3:31-34.
- Ikechebelu JI, Mbamara SU (2011) Should laparoscopy and dye test be a first line evaluation for infertile women in southeast Nigeria?Niger J Med20(4):462-465.
- Moore J, Kennedy S (2000) Causes of chronic pelvic pain. Best Pract Res Clin Obstet Gynaecol14(3):389-402.
- Osuga Y, Koga K, Tsutsumi O, Yano T, Maruyama M, et al. (2002) Role of laparoscopy in the treatment of endometriosis-associated infertility. Gynecol obstet invest53(Suppl1):33-39.
- Speroff L, Fritz MA (2005) Clinical’ gynecologic endocrinology and infertility. In: Speroff L, Fritz MA(Eds.), Lippincott Williams & Wilkins, USA.
- Sinawat S, Pattamadilok H, Seejorn K (2005) Tubal abnormalities in Thai infertile females. J Med Assoc Thai88(6):723-727.






























