The Lead Level of Umbilical Cord Blood in Newborns; Related Contributing and Underlying Factors
Leyla Taherinia1*, Zahra Movahedi2, Mohammad Reza Shocrollahi2, Nastaran Khosravi1*, Shima Javadinia3 and Azardokht Tabataba1
1 Research Center of Pediatric infectious diseases, University of Medical Sciences, Iran
2 Research Center ofPediatric Infectious Diseases, QomUniversity of Medical Sciences and Health services, Iran
3 Department of Lung disease, Zabol University of Medical Sciences, Iran
Submission:September 14, 2018 ; Published: October 10, 2018 ;
*Corresponding author: Dr Leila Taherinia and Nstaran Khosrvi to Research Center of Pediatric Infectious Diseases, Institute of Immunology and Infectious disease, Iran University of Medical Sciences, Tehran, Iran, Tel:+982166516049 ; Fax:+982166516049 ; Email:azardokht_tabatabaei@yahoo.com
How to cite this article: Leyla Taherinia, Zahra Movahedi, Mohammad Reza Shocrollahi, Nastaran Khosravi, Shima Javadinia, Azardokht Tabataba. The Lead Level of Umbilical Cord Blood in Newborns; Related Contributing and Underlying Factors. J Gynecol Women’s Health. 2018: 12(2): 555834. DOI: 10.19080/JGWH.2018.12.555834
Abstract
Introduction: The assessment of serum lead concentration in the newborns could be effective in detection of lead poisoning. The neurodevelopmental disorders and neuropsychological behaviors could be preventable. This study aimed to assess the serum lead levels of cord blood in some hospitalized newborns.
Methods: This cross-sectionalstudy was conducted on 60 newborns who were born in two hospitals in Tehran, during the years 2011-12. The cord blood sampling was performed in the first day of birth and the cord blood lead levels were measured by atomic absorption spectrophotometer. All data were analyzed including thecord blood lead levels, gender, place of residence and drug history of mother. The serum lead concentration >5μg/dL was considered valuable.
Results: In total , 61.4% of newborns were male. 70% of mothers were living in urban area, 13% had a history of drug use and 5% were current smokers .The mean (±SD) of cord blood lead level was 2.97±2.24μg / dL. The cord blood lead levelin 16.7% of samples was >5μg/dL. The cord blood lead levels were associated with maternal age, weight and fetal age (P=0.02, P=0.004, P=0.03), which wasn’t associated with gender, place of residence, drug history and smoking.
Conclusions: Despite the relatively higher cord blood lead level than other studies, the prevalence of high risk newborns (with serum blood Lead levels greater than 5) was low. Further researches are recommended to assess the serum lead level in different areas in order to identify and prevent neurodevelopmental risk factors.
Keywords:Lead; Cord blood; Newborn
Introduction
The lead element is found in various organs, including the heart, bones, intestines, kidneys, and the nervous system. It enters the body through the air, water, soil and food [1-3]. Increasing lead levels in the body causes poisoning known as “Plumbism”[4]. As the first effect of lead poisoning, it binds with sulfidryl group enzymes and reacts with them in order to deactivate their function. Replacement of lead in place of other metals in enzymes such as iron, calcium and zinc disrupts the catalytic action of some vital enzymes in the body. Other consequences of lead poisoning include: the disruption of some enzymes involved in the production of hemoglobin cofactor [5-7], disorder in release of neurotransmitters especially glutamate resulting in learning disabilities and disruption in natural development of the nervous system and the brain [8-10].
According to the study by Woolf et al. [1] In the United States, the lead levels above 5μg/dL in neonates were considered to be associated with increased risk of toxicity. An increase in blood lead levels of more than 10μg/dl was associated with reduced intelligence, short-term memory, concentration and attention [10-12]. Even lead levels of less than 10μg/dl could also cause complications such as severe reduced intelligence and learning disorders[2]. In some cases, lead poisoning in children has been reported with dangerous complications such as seizure, coma and death.
Due to the transfer of lead from fetus to placenta from the 12th week of pregnancy, high levels of lead in maternal blood increases the level of this element in fetus and causes complications in the central nervous system during fetal and neonatal periods
Therefore, the most important way of reducing neural tube disorders and developmental abnormalities in infancy and childhood is primary prevention of lead contact in pregnant mothers[11,12].
The lead level in neonates is typically evaluated by lead measuring in umbilical cord blood [13]. In areas with high level of environmental pollutants such as Tehran, where in some areas concentration of lead air is higher than the established standards, there is a potential for lead exposure. The assessment of serum lead concentration in the umbilical cord blood of neonates in these areas can be useful in identification of highly exposed neonates. The aim of this study was to assess lead concentrations in umbilical cord blood of newborns in neonatal department of Akbarabadi and Rasoul-Akram Hospitals.
Method and Materials
This analytical and cross-sectional study was conducted in the neonatal department of Akbar Abadi and Rasool Akram hospitals during 2011 to 2012. A total number of 60 newborns were selected in a simple andunpredictable manner in the study. After receiving written consent letter from the mothers, all infants received umbilical cord blood sampling during birth. Then, all blood samples were collected in heparin tubes and sent to the laboratory. The cord blood lead was measured by Atomic Absorption Spectrometry (AAS8000 Atomic Absorption Spectrometer by Hogyedong Anyang, 431-836, Korea). The data was recorded in prepared checklists containing the umbilical cord blood lead concentration and the basic information including gender, weight, gestational age, maternal age, history of drug and tobacco use (before and after pregnancy), and place of living (in the city or suburbs). The data was entered into SPSS software version 20 and analyzed statistically.
The frequency of blood cord blood lead was calculated by descriptive statistics (mean and standard deviation). The relationship between the lead concentration and sex, age, weight in newborn, place of residence, history of drug use and smoking in mothers were analyzed by multivariate regression analysis. In this study, lead values above 5μg/dL were considered as a limit value. P value less than 0.05 was considered significant[14,15].
Result
From the total number of 60 neonates in this study, 35 (61.4%) were male and (22.6%) were female. These newborns were born with gestational age ranging from 28 to 42 weeks. The mean and standard deviation of gestational age were 37.2±4.64 weeks, and the mean and standard deviation of birth weight were 2701.8±642 grams. The maternal age was between 16 and 42 years with a mean of 29.20±6.73.
According to the data, 70% (42 mothers) were living in Tehran, 13% (8 mothers) had a positive drug history, 5% (3 mothers) were current smokers and 3.3% (2 mothers) had a history of quitting their smoking. The mean and standard deviation of smoking in the mothers was 0.9±5.45 cigarettes per day. The mean and standard deviation of umbilical cord blood lead concentration in total neonates were 2.97±2.24μg/dL.
The multivariate regression analysis showed that the cord blood lead concentration (P=0.99) was not related to factors including place of residence (P=0.2), drug use (P-value=0.2), tobacco use (P-value 0.2). Totally, 16.7% (10 neonates) had lead levels above 5μg / dL and 83.3% (50 neonates) were reported with lead levels below 5μg/dL.
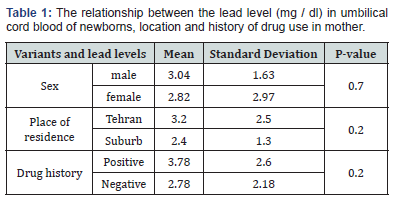
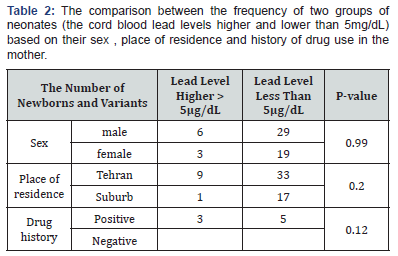
The frequency of newborns with lead levels higher and lower than 5μg/dL was not significantly different in terms of sex (P-value=0.99), place of residence (P-value=0.2), history of drug use (P-value=0.12), and Smoking (=P-value). The two groups of high risk neonates (the lead level less than 5) were considerably different regarding their mean fetal age (P=0.03), the neonatal weight (P=0.004) and maternal age (P=0.02)(Table 1&2).
Discussion and Conclusion
In present study, the concentration of umbilical cord blood lead in all neonates was reported about 3μg/dL. In some studies, the level of cord blood lead was mentioned less than the result of present study. In the study by Needleman et al. [8], Conducted in Boston, USA in 1979, the neonatal cord blood lead concentration was reported around 0.6μg/dL. Based on the findings of this study, the neonatal umbilical cord blood lead levels more than 10μg/dL could result in neurological disorders in the first few years of life. Another study by Satin et al. [13]. In California in 1991 showed the cord blood lead levels of about 0.5μg/dL. However, lead level was detected more than 10μg/dL in 3% of the samples.
The higher levels of umbilical cord blood lead in newborns, in the present study, may be due to air pollution in Tehran. Nowadays, the effect of air pollution has been proven on blood lead levels in children. The blood lead levels of children aged 1 to 5 years has been reduced by controlling the causes of air pollution and other environmental factors in the United States. The prevalence of serum lead levels higher than 10μg/dL decreased from 6.6% in 1986-1991 to 1.4% in 2006 [7]. In some studies, the neonatal blood lead concentrations were higher than results in this study.
In another study in Tehran, conducted by Khosravi et al. [16] total 60 children with an average age of 32 months old were assessed based on their blood lead level. The lead level in children with a history of seizure was 4.36±3.65 and in children without seizure was 3.38 + -4.73μg/dl. The higher blood lead level in this study could be attributed to the higher age of samples compared to the present study.
Dietrich et al. [17]Measured the blood lead levels in pregnant women and infants less than 3 months old. It was reported approximately 30μg/dL. In the present study, 16.7% of the neonates had the lead level of higher than 5μg/dL and 83.3% of neonates were considered as the lead level of lower than 5μg/dL. Some studies reported similar results to this finding[8,12,13].
Among the recent studies in Infectious Diseases Research Center of Children of Iran University of Medical Sciences, 10% of children had blood lead levels higher than 10μg/dL [16]. In this study, different factors were evaluated regarding their relationship with high levels of lead in umbilical cord blood. The level of umbilical cord blood lead was correlated with two factors: the maternal age and fetal weight. In other words, the lead level in neonatal cord blood is expected to increases parallel to maternal age and neonatal weight.
These risk factors had been investigated in some other studies. In a recent study in this center, no difference in blood lead level was reported between the two groups of children with and without a history of seizure. The blood lead level was not related to the age, gender, and other variables of children. This result was similar to the findings of present study. The results of Jones et al. [18]. study indicated that the increase in maternal age was associated with an increase in lead levels in the neonate, similar to the present study. Moreover, living in old houses, poverty, and black race were other risk factors associated with higher blood lead level
In a study by Rossi [4], there was no association between the serum lead levels of patients with the age and the presence of fever in patients. This was contrary to the findings of the present study.Because of the importance of lead poisoning in newborns and the lack of safe blood lead levels in neonates for developing neurodegenerative disorders, it is highly recommended that in future studies, the serum lead levels should be evaluated in other infants. Such studies should be repeated in the different regions and compared the obtained results with each other in order to identify risk factors and prevent neurodevelopmental complications in newborns.
Totally, in current study, the concentration of lead level in the umbilical cord blood was reported about 3μg/dL, which was higher than lead levels in other studies. However, neonates with higher serum lead levels (the lead levels more than 5μg/dL) had a low frequency in the present study. Fortunately, the risk of lead poisoning was observed in only 16.7% of newborns. Additionally, the lead level of umbilical cord blood in neonates was directly associated withthe maternal age and infant weight.
References
- Woolf AD, Goldman R, Bellinger DC (2007) Update on the clinical management of childhood lead poisoning. Pediatr Clin North Am 54(2): 271-294.
- Bellinger D, Leviton A, Needleman HL, Waternaux C, Rabinowitz M, et al. (1986) Low-level lead exposure and infant development in the first year. Neurobehav Toxicol Teratol 8(2): 151-161.
- Guidotti TL, Ragain L (2007) Protecting children from toxic exposure: three strategies. Pediatr Clin North Am 54(2): 227-235.
- Rossi E (2008) Low level environmental lead exposure-a continuing challenge. Clin Biochem Rev 29(2): 63-70.
- Patrick L (2006) Lead toxicity, a review of the literature. Part 1: Exposure, evaluation, and treatment. Altern Med Rev 11(1): 2-22.
- Barbosa F, Tanus-Santos JE, Gerlach RF, Parsons PJ (2005) Acritical review of biomarkers used for monitoring human exposure to lead: advantages, limitations, and future needs. Environ Health Perspect 113(12): 1669-1674.
- Fujita H, Nishitani C, Ogawa K (2002) Lead, chemical porphyria, and heme as a biological mediator. Tohoku J Exp Med 196(2): 53-64.
- Needleman H (2004) Lead poisoning. Annu Rev Med 55: 209-222.
- Xu J, Yan HC, Yang B, Tong LS, Zou YX, et al. (2009) Effects of lead exposure on hippocampal metabotropic glutamate receptor subtype 3and 7 in developmental rats. Journal of negative results in biomedicine 8: 5.
- Sanders T, Liu Y, Buchner V, Tchounwou PB (2009) Neurotoxiceffects and biomarkers of lead exposure: a review. Rev Environ Health 24(1): 15-45.
- Meyer PA, McGeehin MA, Falk H (2003) A global approach to childhood lead poisoning prevention. International journal of hygiene and environmental health 206(4-5): 363-369.
- Bellinger DC (2008) Very low lead exposures and childrens neurodevelopment. Curr Opin Pediatr 20(2): 172-177.
- Satin KP, Neutra RR, Girgis G, Flessel P (1991) Umblical cord blood lead levels in California. Arch Environ Health 46(3): 167-173.
- Meshkinian A, Asilian H, Nazmara S, Shahtaheri J (2003) Determination of lead in the environment and in the urban service workers in a Tehran manicipility district. SJSPH 1(3): 31-40.
- Bound JP, Harvey PW, Francis BJ (1997) Involvement of deprivation and environmental lead in neural tube defects: a matched case-control study. Arch Dis Child 76(2): 107-112.
- Khosravi N, Tabatabai A, Izadi A, Norbakhsh S, Ashouri S, et al. (2014) Assessments of blood lead levels in children with febrile convulsion. MJIRI 28(97).
- Dietrich KN, Krafft KM, Bornschein RL, Hammond PB, Berger O, et al. (1987) Low-level fetal lead exposure effect on neurobehavioral development in early infancy. Pediatrics 80(5):721-730.
- Jones RL, Homa DM, Meyer PA, Brody DJ, Caldwell KL, et al. (2009) Trends in blood lead levels and blood lead testing among US children aged 1 to 5 years, 1988-2004. Pediatrics 123(3): e376-385.






























