- Research Article
- Abstract
- Introduction
- Methods
- Inclusion and Exclusion Criteria
- Data Processing and Analysis
- Data Quality Control Measures
- Ethical Considerations
- Results
- Prevalence of Pregnancy Induced Hypertension
- Variables Related to Obstetric Conditions
- Medical and Family History Related Variables/Factors
- Variables Related to Personal Risks
- Association between Dependent and Independent Variables
- Discussion
- Conclusion
- Declaration
- Acknowledgement
- References
Pregnancy Induced Hypertension and Associated Factors among Pregnant Women Receiving Antenatal Care Service at Jimma Town Public Health Facilities, South West Ethiopia
Tesfaye Abera Gudeta1, Tefera Belachew Lema2 and Sena Belina Kitila2
1Department of nursing, Mizan Tepi University, Ethiopia
2Department of Population and Family health, Jimma University, Ethiopia
3Department of Nursing and Midwifery, Jimma University, Ethiopia
Submission: April 24, 2018; Published: July 17, 2018
*Corresponding author: Tesfaye Abera Gudeta, Department of nursing, Mizan Tepi University, Ethiopia, Email: tesfeabera2013@gmail.com
How to cite this article: Tesfaye A G, Tefera B L, Sena B K. Pregnancy Induced Hypertension and Associated Factors among Pregnant Women Receiving Antenatal Care Service at Jimma Town Public Health Facilities, South West Ethiopia. J Gynecol Women’s Health. 2018: 10(3): 555792. DOI: 10.19080/JGWH.2018.10.555792
- Research Article
- Abstract
- Introduction
- Methods
- Inclusion and Exclusion Criteria
- Data Processing and Analysis
- Data Quality Control Measures
- Ethical Considerations
- Results
- Prevalence of Pregnancy Induced Hypertension
- Variables Related to Obstetric Conditions
- Medical and Family History Related Variables/Factors
- Variables Related to Personal Risks
- Association between Dependent and Independent Variables
- Discussion
- Conclusion
- Declaration
- Acknowledgement
- References
Abstract
Background: Hypertensive disorders of pregnancy are a major health burden in the obstetric population as it is one of the leading causes of maternal and perinatal morbidity and mortality. World Health Organization estimates that at least one woman dies every seven minutes from complications of hypertensive disorders of pregnancy.
Objective:To assess prevalence of pregnancy induced hypertension and associated factors among pregnant women receiving antenatal care service at Jimma town public health facilities, Southwest Ethiopia.
Methods:Health facility based cross-sectional study was carried out from March 01-30, 2015. The study was used the total sample size of 356 pregnant women who were proportionally allocated to the hospitals and health centers. Then the study participants were systematically selected from each health facility. The data was collected using pre-tested structured questionnaireadaptedfrom validated questionnaire, content validity was checked by experts and reliability of the scaled tools were tested by cronbach’s alpha test( 0.70). Prior to analysis data was entered and checked using Epi data and exported in to Statistical Package for Social Sciences (SPSS) version 20.00. Bivariate analysis was carried out between the dependent and independent to identify variables candidate for multivariable logistic regression. Multivariable logistic regression analysis was made to obtain odds ratio and the confidence interval of statistical associations between pregnancy induced hypertension and its associated factors.
Result:Prevalence of pregnancy induced hypertension was 10.3% and among mothers had pregnancy induced hypertension, preeclampsia 23(63.9%) was the most common type. This study also showed that rural residence (Adjusted Odds Ratio (AOR)=5.310, 95%CI=1.518-18.574), positive family history of chronic hypertension (AOR=9.90, 95%CI=2.31-42.44), Positive family history of pregnancy induced hypertension (AOR=9.13(2.33-35.78)), kidney diseases (AOR=3.97, 95%CI=1.36-11.56) and psychological stress (AOR=5.79, 95%CI=1.66-20.25) were statistically significant association with pregnancy induced hypertensi
Conclusion:According to this study, the prevalence of pregnancy induced hypertension was high. Address, family history of chronic hypertension, family history of pregnancy induced hypertension, kidney diseases, psychological stress during pregnancy were the factors contributing pregnancy induced hypertension.
Keywords: Pregnancy induced hypertension; Pregnancy; Antenatal care service; Women
Abbrevations: HDP: Hypertensive Disorders of Pregnancy; PIH: Pregnancy Induced Hypertension; EDHS: Ethiopian Demographic health survey; SD: Standard Deviation; ANC: Antenatal Care; AOR: Adjusted Odds Ratio; BP: Blood Pressure; CI: Confidence interval; DBP: Diastolic Blood pressure; SBP: Systolic Blood Pressure
- Research Article
- Abstract
- Introduction
- Methods
- Inclusion and Exclusion Criteria
- Data Processing and Analysis
- Data Quality Control Measures
- Ethical Considerations
- Results
- Prevalence of Pregnancy Induced Hypertension
- Variables Related to Obstetric Conditions
- Medical and Family History Related Variables/Factors
- Variables Related to Personal Risks
- Association between Dependent and Independent Variables
- Discussion
- Conclusion
- Declaration
- Acknowledgement
- References
Introduction
Hypertension in pregnancy is defined as a systolic blood pressure ≥140 or diastolic blood pressure ≥90 mmHg or both. Both systolic and diastolic blood pressure elevations are important in the identification of Hypertension Disorder of Pregnancy (HDP) [1].
Pregnancy Induced Hypertension (PIH) is hypertension in pregnancy that occurs after 20 weeks of gestation in a woman with previously normal blood pressure. The general classification of PIH during pregnancy are Gestational hypertension (without proteinúria), pre-eclampsia (with proteinúria), and eclampsia (pre-eclampsia with convulsions) [2] and there are three primary characteristics of pregnancy induced hypertension conditions; high blood pressure (a blood pressure reading higher than 140/90mmHg or a significant increase in one or both pressures), protein in the urine, abnormal edema [3]. PIH is a global problem and the most common medical problem requiring special attention in the intrapartum period [4,5].
The PIH is usually diagnosed in late pregnancy by the presence of hypertension with proteinuria and /or edema. Clinical, biophysical, and biochemical tests have been proposed for prediction or early detection of PIH. Despite the fact that diagnostic criteria, the clinical manifestation of the disease, the management and the prognosis are clear and homogenous, the prevalence of maternal and fetal complications still differ considerably among studies [6].
As a study conducted in Latin American and Caribbean, Pakistan, New York, and Sri lanka identified the following risk factors for developing pregnancy induced hypertension: null parity, multiple pregnancies, history of chronic hypertension, gestational diabetes, fetal malformation and obesity [7], extreme maternal age (less than 20 or over 40 years), history of PIH in previous pregnancies, preexisting diseases like renal disease, diabetes mellitus, cardiac disease, unrecognized chronic hypertension, positive family history of PIH which shows genetic susceptibility, psychological stress ,alcohol use, rheumatic arthritis, very underweight and overweight, and low level of socioeconomic status are the risk factors for PIH [5,8-10].
According to a population based study in South Africa the incidence of hypertensive disorders of pregnancy was 12% and hypertension disorder of pregnancy was the commonest cause of maternal death which contributed 20.7% of maternal deaths [11]. Similarly Ethiopian Demographic Health survey (EDHS) 2011 reported, maternal mortality ratio is 676 deaths per 100,000 live births and pregnancy induced hypertension the second leading cause of maternal death [12]. A review study conducted on the causes of maternal mortality in Ethiopia showed that, the proportion of maternal mortality in Ethiopia due to hypertensive disorders between 1980 and 2012 is in increased trend from 4%-29% [13].
Pregnancy induced hypertension is leading causes of pregnancy associated morbidity and it is most frequent cited cause of maternal death [14]. Despite the fact that hypertensive disorders in pregnancy is leading causes of maternal morbidity and mortality during pregnancy but little is known about the current magnitude and associated factors among pregnant women in Ethiopia and specifically in Jimma. This study therefore aims to fill this gap by assessing the current status and factors associated with hypertensive disorders in pregnancy among pregnant women attending antenatal service in Jimma town, south west Ethiopia, through health facility based cross sectional study. It is hoped that the results of the study will provide valuable information for the design of possible programs and interventions.
- Research Article
- Abstract
- Introduction
- Methods
- Inclusion and Exclusion Criteria
- Data Processing and Analysis
- Data Quality Control Measures
- Ethical Considerations
- Results
- Prevalence of Pregnancy Induced Hypertension
- Variables Related to Obstetric Conditions
- Medical and Family History Related Variables/Factors
- Variables Related to Personal Risks
- Association between Dependent and Independent Variables
- Discussion
- Conclusion
- Declaration
- Acknowledgement
- References
Methods
Study area and period
The study was conducted in Jimma town public health facilities from March 01-30/2015.The town is located 357 kilometers to southwest of Addis Ababa.The total population projection of 2014/15 Jimma town was 184925. The town has one referral hospital, one district hospital, four health centers and 47 private clinics. The total reproductive age groups and targets of pregnant women of Jimma town was 40692, 6834 respectively.
The study was conducted in all public health facilities found in Jimma town namely; Jimma University Specialized Hospital, Shenen Gibe Hospital, Jimma Health Center, Higher-2-Health Center, Mendera Kochi Health Center and Bacho Bore Health Center.
Study design
Health facility based cross-sectional study design with quantitative data collection method was used.
Source and study population
All pregnant women attending antenatal care service at Jimma town public health facilities during the study period were considered as source of population and all sampled pregnant women attending antenatal care service at Jimma town public health facilities during the study period were considered study subjects.
- Research Article
- Abstract
- Introduction
- Methods
- Inclusion and Exclusion Criteria
- Data Processing and Analysis
- Data Quality Control Measures
- Ethical Considerations
- Results
- Prevalence of Pregnancy Induced Hypertension
- Variables Related to Obstetric Conditions
- Medical and Family History Related Variables/Factors
- Variables Related to Personal Risks
- Association between Dependent and Independent Variables
- Discussion
- Conclusion
- Declaration
- Acknowledgement
- References
Inclusion and Exclusion Criteria
All pregnant women attending antenatal care service with gestational age greater than 20 weeks were included in the study whereas pregnant women gestational age less than 20 weeks and those of critically ill and unable to communicate after full course of treatment were excluded from the study.
Sample size determination and sampling techniques
The samples ize was calculated by using a single population proportion sample size calculation formula, then the final sample size was 356. The source of population was taken from twelve months report of pregnant women attending antenatal care service at all public health facilities of Jimma town. Then the average was taken, which was 2072 pregnant women monthly. The total sample size was allocated proportionally to the different care giving public health facilities found in Jimma town according to the number of pregnant women attending antenatal care service in the respective health facilities .Then the study participants were systematically selected from each health facilities.The first pregnant woman was selected based on lottery method and the rest were selected every six interval.
Operational definition
In this study, pregnancy induced hypertension was operationalized as if the blood pressure of pregnant women receiving antenatal care service is 140/90mmHg after 20 weeks of gestation, measured two times six hours apart by trained data collectors and with or without proteinuria. Pregnancy induced hypertension includes gestational hypertension, preeclampsia, and eclampsia, superimposed preeclampsia on chronic hypertension, andPsychologicalstress operationalized as psychological stress measurement items of 9 questions score of single woman greater than that of the mean score was considered as psychologically stressed.
Data collection and Instruments
The data was collected using pre-tested structured questionnaire adapted and customized from validated questionnaire [15-17]. Questionnaires were first adapted in English then translate to Afan Oromo and Amharic by expert and translated back to English to see consistency of the question. Seven data collectors who were four diploma midwives and three nurses in qualification and four supervisors who were BSc nurses by qualification and who were fluent in speaking, writing and reading AfanOromo and Amharic language were recruited purposefully from their respective facilities to maintain the quality of the data. Data were collected through direct interview and supported by reviewing of medical record or reports for pregnant women referred from different health facilities to the study area for the purpose of taking blood pressure and protein in urine at time of diagnosis. Pretested structured questionnaire was used by trained data collectors. Blood pressure measurements were taken in the sitting position after the woman has rested at least 10 minutes by using a mercury sphygmomanometer apparatus from non-dominant arm and for referred women; BP and protein urea at time of diagnosis were taken.
- Research Article
- Abstract
- Introduction
- Methods
- Inclusion and Exclusion Criteria
- Data Processing and Analysis
- Data Quality Control Measures
- Ethical Considerations
- Results
- Prevalence of Pregnancy Induced Hypertension
- Variables Related to Obstetric Conditions
- Medical and Family History Related Variables/Factors
- Variables Related to Personal Risks
- Association between Dependent and Independent Variables
- Discussion
- Conclusion
- Declaration
- Acknowledgement
- References
Data Processing and Analysis
EPI data Statistical software version 3.1 and Statistical Package for Social Sciences (SPSS) software version 20.0 were used for data entry and analysis. After organizing and cleaning the data, frequencies and percentages were calculated to all variables that are related to the objectives of the study. Variables with P-value of less than 0.25 in binary logistic regression analysis were entered into the multivariable logistic regression. Odds ratio with 95% confidence interval was used to examine associations between dependent and independent variables. P. value less than 0.05 was considered as statistically significant.
- Research Article
- Abstract
- Introduction
- Methods
- Inclusion and Exclusion Criteria
- Data Processing and Analysis
- Data Quality Control Measures
- Ethical Considerations
- Results
- Prevalence of Pregnancy Induced Hypertension
- Variables Related to Obstetric Conditions
- Medical and Family History Related Variables/Factors
- Variables Related to Personal Risks
- Association between Dependent and Independent Variables
- Discussion
- Conclusion
- Declaration
- Acknowledgement
- References
Data Quality Control Measures
The quality of the data was assured by using validated pretested questionnaires. Prior to the actual data collection; content validity was checked by experts, pretest was done on 5% of the total study eligible subjects.The questions used to measure psychological stress adapted from validated questionnaire then after modification of the questions the reliability of the questions tested yielding cronbach’s alpha value of 0.70. Data collectors were trained for one day intensively on the study instrument and data collection procedure that includes the relevance of the study, objective of the study, confidentiality of the information, informed consent and interview technique. The data collectors were worked under close supervision of the supervisors to ensure adherence to correct data collection procedures, supervisors and investigator checked the filled questionnaires at the end of data collection every day for completeness. Moreover, the data were carefully entered and cleaned before the beginning of the analysis.
- Research Article
- Abstract
- Introduction
- Methods
- Inclusion and Exclusion Criteria
- Data Processing and Analysis
- Data Quality Control Measures
- Ethical Considerations
- Results
- Prevalence of Pregnancy Induced Hypertension
- Variables Related to Obstetric Conditions
- Medical and Family History Related Variables/Factors
- Variables Related to Personal Risks
- Association between Dependent and Independent Variables
- Discussion
- Conclusion
- Declaration
- Acknowledgement
- References
Ethical Considerations
Written ethical clearance obtained from Jimma University, college of health science of Institutional Review Board. Permission was obtained from respective health institutions and written consent (signed on the informed consent sheet) was obtained from pregnant mother attending antenatal care service after discussing the objective of the study. For pregnant women were under 18 years old, the written informed consent were taken from parent. The right of the respondents to refuse answering for few or all of the questions were also be respected. The letter of ethical approval was attached with manuscript.

- Research Article
- Abstract
- Introduction
- Methods
- Inclusion and Exclusion Criteria
- Data Processing and Analysis
- Data Quality Control Measures
- Ethical Considerations
- Results
- Prevalence of Pregnancy Induced Hypertension
- Variables Related to Obstetric Conditions
- Medical and Family History Related Variables/Factors
- Variables Related to Personal Risks
- Association between Dependent and Independent Variables
- Discussion
- Conclusion
- Declaration
- Acknowledgement
- References
Results
A total of 351 pregnant women participated in the study, 272(77.5%) from antenatal clinics and the rest were from pregnant women admitted to maternity wards. The mean age of the respondents was 24.83 with SD±4.85, 119(33.9%) were between age group of 25-29 years and 210(59.8%) were from urban and the rest were from rural areas. Ethnicity of the study subjects indicated that, 252(71.8%) were Oromo followed by Amhara 42(12%). Majority of the study subjects, 242(68.9%) were Muslims, 341(97.2%) were married, 158(45.0%) had primary education, 257(73.2%) were housewives, 232(66.1%) of them were in the middle income class and 143(40.7%) of them had family size of 1-2 (Table 1).
- Research Article
- Abstract
- Introduction
- Methods
- Inclusion and Exclusion Criteria
- Data Processing and Analysis
- Data Quality Control Measures
- Ethical Considerations
- Results
- Prevalence of Pregnancy Induced Hypertension
- Variables Related to Obstetric Conditions
- Medical and Family History Related Variables/Factors
- Variables Related to Personal Risks
- Association between Dependent and Independent Variables
- Discussion
- Conclusion
- Declaration
- Acknowledgement
- References
College of Respondents and Knowledge and Usage of Ecs
The prevalence of PIH among pregnant women receiving antenatal care services was 36(10.3%). The minimum, maximum and mean systolic blood pressure were 80mmHg, 190mmHg and 110.78mmHg with SD±17.10 respectively. The minimum, maximum and mean diastolic blood pressures were 50mmHg, 140mmHg and 71.85mmHg with SD±13.04 respectively. The result dipstick urine test, proteinuria ranges from negative to +++ .Out of the total of 36 pregnant women who had PIH, 11(30.6%) were gestational hypertension, 23 (63.9%) were preeclampsia and 2 (5.6%) were eclampsia.
- Research Article
- Abstract
- Introduction
- Methods
- Inclusion and Exclusion Criteria
- Data Processing and Analysis
- Data Quality Control Measures
- Ethical Considerations
- Results
- Prevalence of Pregnancy Induced Hypertension
- Variables Related to Obstetric Conditions
- Medical and Family History Related Variables/Factors
- Variables Related to Personal Risks
- Association between Dependent and Independent Variables
- Discussion
- Conclusion
- Declaration
- Acknowledgement
- References
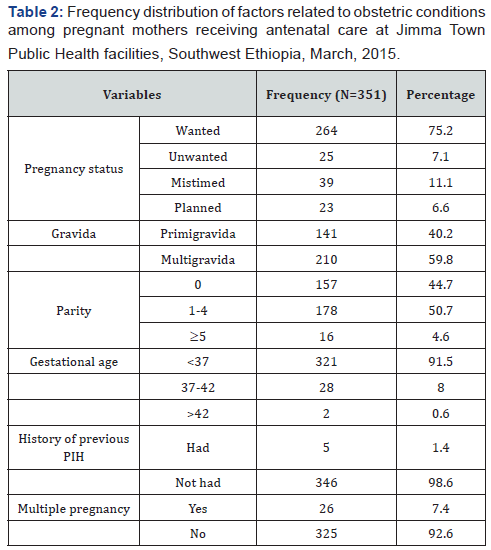
Variables Related to Obstetric Conditions
From the total study participates, 264(75.2%) of pregnancies were wanted and 210(59.8%) of pregnancy were multigravida. Parity of the women showed that 178(50.7%) of women had 1-4 children and majority, 321(91.5%) had gestational age less than 37 weeks. Only 5(1.4%) of pregnant mothers receiving antenatal care service had previous history of PIH and 26(7.4%) of the women had multiple pregnancies (Table 2).
- Research Article
- Abstract
- Introduction
- Methods
- Inclusion and Exclusion Criteria
- Data Processing and Analysis
- Data Quality Control Measures
- Ethical Considerations
- Results
- Prevalence of Pregnancy Induced Hypertension
- Variables Related to Obstetric Conditions
- Medical and Family History Related Variables/Factors
- Variables Related to Personal Risks
- Association between Dependent and Independent Variables
- Discussion
- Conclusion
- Declaration
- Acknowledgement
- References
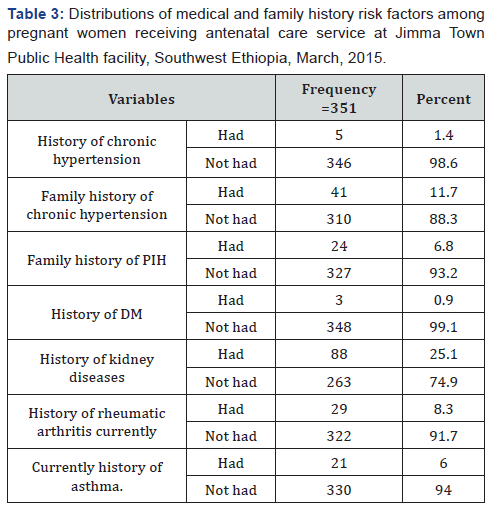
Medical and Family History Related Variables/Factors
Medical and family histories of illness formed the major predisposing factors, 5(1.4%) had history of chronic hypertension and 41(11.7%) of them had family history of chronic hypertension, 24(6.8%) of them had family history of PIH commonly from women’s relatives, 88 (25.1%) of the respondents had history of kidney diseases during current pregnancy, 3(0.9%) had history of diabetic mellitus, 29(8.3%) and 21(6.0%) had history of rheumatic arthritis and asthma respectively (Table 3).
- Research Article
- Abstract
- Introduction
- Methods
- Inclusion and Exclusion Criteria
- Data Processing and Analysis
- Data Quality Control Measures
- Ethical Considerations
- Results
- Prevalence of Pregnancy Induced Hypertension
- Variables Related to Obstetric Conditions
- Medical and Family History Related Variables/Factors
- Variables Related to Personal Risks
- Association between Dependent and Independent Variables
- Discussion
- Conclusion
- Declaration
- Acknowledgement
- References
Variables Related to Personal Risks
All of the respondents did not smoke cigarette, but 35(10%) had family members particularly their husbands who smoke cigarette (94.3%) and only 19(5.4%) of the women had any alcoholic drink in the past two years. Out of the total study participants, 308(87.7%) of the pregnant women used caffeine (coffee & tea) drinks .Among the users, 263(85.4%) use coffee and 45(14.6%) use tea commonly. A greater proportion, 318(90.6%) of the respondents had mid upper arm circumference ≥21cm. More than half, 209(59.5%) of the respondents sleep 7-8 hours per night, 52(14.8%) sleep 6 hours, 90(25.6%) sleep ≥9 hours per night and 104(29.6) had a nap at day time. Only 31(8.8%) of the women were involved in scheduled regular physical exercise during their current pregnancy. Based on the nine items used to assess psychological stress, 140(39.9%) of the pregnant women had psychological stress. Only 27 (7.7%) did not get diversified diet (Table 4).
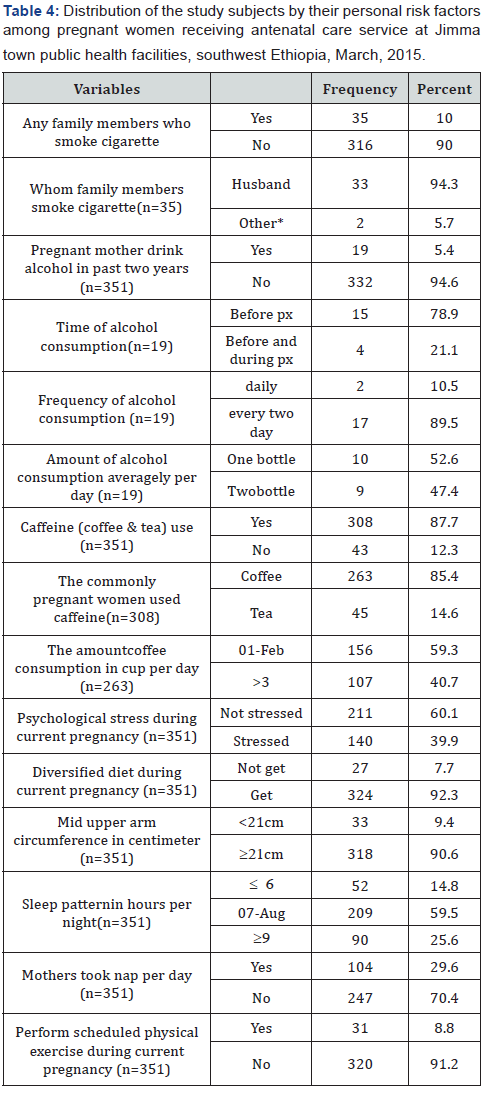
PX=pregnancy
Other*= Children, Relatives, any other person live with family members
- Research Article
- Abstract
- Introduction
- Methods
- Inclusion and Exclusion Criteria
- Data Processing and Analysis
- Data Quality Control Measures
- Ethical Considerations
- Results
- Prevalence of Pregnancy Induced Hypertension
- Variables Related to Obstetric Conditions
- Medical and Family History Related Variables/Factors
- Variables Related to Personal Risks
- Association between Dependent and Independent Variables
- Discussion
- Conclusion
- Declaration
- Acknowledgement
- References
Association between Dependent and Independent Variables
Age, family size, gestational age, multiple pregnancy, positive history of chronic hypertension, diversified diet and antenatal care follow up before data collection periodwere found to have significant association with pregnancy induced hypertension. Family history of PIH, family history of chronic hypertension, kidney disease, number of routine antenatal care follow up and psychological stress had strong statistical association with pregnancy PIH in binary logistic regression.
In multivariable logistic regression analysis, the factors contributing pregnancy induced hypertension were identified: Address, positive family history of chronic hypertension, positive family history of pregnancy induced hypertension, kidney diseases during current pregnancy and psychological stress had statistically significant association with pregnancy induced hypertension.
Pregnant women from a rural residence weremore likely to report having PIH when compared to those of pregnant women residing in urban areas (AOR=5.31, 95%CI=(1.52-18.57), p=0.009), those who had family history of chronic hypertension were 9.903 times more likely to develop PIH when compared with pregnant women those who did not have family historyof chronic hypertension (AOR=19.9 at 95% CI= (2.31-42.44), p=0.002) and those pregnant women who had family history of pregnancy induced hypertension weremore likely to developed pregnancy induced hypertension than those did not have family history of chronic hypertension(AOR=9.13 at95%CI= (2.33- 35.78),p=0.002).
Findings of the study showed that those pregnant women with kidney disease during current pregnancy were more likely to developed PIH as compared to pregnant women with pregnant did not have kidney disease during pregnancy (AOR=3.97 at 95%CI=(1.36-11.56),p=0.012) and being psychologically stressed during pregnancy increases the like hood of PIH by 5.79 times. (AOR= 5.79, 95%CI= (1.66-20.25, P=0.006) when compared to those pregnant women who did not have psychological stress during pregnancy (Table 5).

The above table shows variables the statistically significant variables in the multiple logistic regression analysis after adjusting variables candidate for multivariable logistic regression (Age of women, address, occupational status, monthly income, family size, gestational Age, multiple pregnancies, history of chronic hypertension, family history of chronic hypertension, family history of PIH, kidney diseases, alcohol intake, diversified diet, sleep pattern, had a nap at day time, (Antenatal) ANC follow up, non-routine ANC follow up, utilization of health facility for other problem and Psychological stress)
- Research Article
- Abstract
- Introduction
- Methods
- Inclusion and Exclusion Criteria
- Data Processing and Analysis
- Data Quality Control Measures
- Ethical Considerations
- Results
- Prevalence of Pregnancy Induced Hypertension
- Variables Related to Obstetric Conditions
- Medical and Family History Related Variables/Factors
- Variables Related to Personal Risks
- Association between Dependent and Independent Variables
- Discussion
- Conclusion
- Declaration
- Acknowledgement
- References
Discussion
Hypertensive disorders of pregnancy are an important cause of severe morbidity, long-term disability and death among mothers and their babies [18]. In this study, the prevalence of pregnancy PIH among pregnant women receiving antenatal service was 36(10.3%).This reflects that the morbidity and mortality of the mother and the fetus high due to this diseases condition. If appropriate preventive measures are not taking place, the risk of PIH among pregnant women might be ranked as first cause of maternal mortality.This finding was slightly higher than global prevalence of pregnancy induced hypertension which ranges between 5-10% [18] and also systematic review study conducted in Nigeria shows that the prevalence of PIH ranges between 2% to 10% [19]. In addition to the above studies, the prevalence of PIH in this study was higher than the studies conducted in Iran which was 9.8% [20], India 7.8% [21], Port Elizabeth 6.69% [6], and Ethiopia (Tikur Anbessa hospital 5.3% [22] and Jimma University specialized hospital 8.5% [23]. The possible explanation for this difference mightbe the difference in study period, study design which most of them used longitudinal study design, sample size and study area. In addition to this, the gap might be due to current health policy of the country which was focused on implementation of focused ANC and exempted service for maternal care might be increases the health care seeking behaviour of pregnant women which increases the detection of the case. On the other hand an increment of the prevalence of PIH might be related to an increased burden of non-communicable diseases in our country
On the other hand, the prevalence of PIH in this study was lower than the studies conducted in Brazil [14] and South Africa [11] which were 13.9% and 12% respectively. This gap might be due to the differences in the study period, sample size, geographical difference of the study areas and health seeking behavior of the pregnant women in the area.
This study also revealed that factors associated with pregnancy induced hypertension; residence, positive family history of chronic hypertension, positive family history of pregnancy induced hypertension, kidney diseases and psychological stress are statistically significant association with PIH. Pregnant women from a rural residence were five times more likely to develop PIH when compared to those of pregnant women residing in urban areas.
This finding was in line with the study conducted at Jimma University Specialized Hospital which showed that rural residents were more suffered with pregnancy induced hypertension than urban dwellers [23] but inconsistent with the comparative cross sectional study conducted in Ghana showedthat pregnancy induced hypertension common among urban than rural area (3.1% versus 0.4% ) [24]. The discrepancy might be due to the difference in the study area, health polices of the country, lifestyle of urban women’s of Ghana and health seeking behavior Ghana’s rural community.
According to this study, those womenwho havepositive family history ofchronic hypertension and positive family history of pregnancy induced hypertension had about ten and nine times respectively greater odds of developing pregnancy induced hypertension as compared to those whohaven’t it. This finding is consistent with that of studies conducted in Pakistan [8], Ghana [24] and New York [25] shows that family history of chronic hypertension and family history of PIH had strong association with PIH and also text book of current diagnosis and treatment in obstetrics and gynecology support this finding [2]. This might have occurred due to genetic factors that contribute to the physiologic predisposition of pregnancy induced hypertension.
As this study showed, having kidney disease during pregnancy increases the likelihood of pregnancy induced hypertension by 3.97 times. This finding is similar with the study conducted in the United Kingdom [26] and Netherlands and New York [25] which showed that preexisting renal disease had a significant association with pregnancy induced hypertension and other theories support that renal physiological function had direct relationship with cardiovascular system [27].
According to this study, being psychologically stressed during pregnancy increases the likelihood of pregnancy induced hypertension by 5.79 times. This result was consistent with a study conducted in New York [9] and also this finding is in lined with a study conducted in Sri Lanka with a slight difference [10]. Stress activates the hypothalamus-pituitary-adrenal cortex system (HPA), which in turn increases in levels of corticosteroids and catecholamine. Stress also activates the sympathetic nervous system and affects the immune system and increased levels of corticotrophin-releasing hormone and increased sympathetic activity which increases the risk of PIH [28].
This study identified the factors contributing pregnancy induced hypertension, so all pregnant women having such risk factors should supplemented with calcium, low dose of aspirin to prevent it and early detection and treatment mandatory to reduce the morbidity and mortality of women secondary to PIH. This cross-sectional study has possible limitations that may arise from pregnant women’sreadiness and ability to provide every information about themselves and their family correctly based on which PIH was measured and recall bias may be introduced during data collection from the pregnant women as they were self-referred.
However; measure has been taken to minimize these limitations were using questions targeted information. The others limitation of this study was few variables have small observation which causes lower precision, so it was carefully interpreted.Moreover, the use of pretested and validated questionnaire, inclusion of all public health institutions found in Jimma town and data collection from both in patient and ANC unit were other strengths of this study.
- Research Article
- Abstract
- Introduction
- Methods
- Inclusion and Exclusion Criteria
- Data Processing and Analysis
- Data Quality Control Measures
- Ethical Considerations
- Results
- Prevalence of Pregnancy Induced Hypertension
- Variables Related to Obstetric Conditions
- Medical and Family History Related Variables/Factors
- Variables Related to Personal Risks
- Association between Dependent and Independent Variables
- Discussion
- Conclusion
- Declaration
- Acknowledgement
- References
Conclusion
The prevalence of pregnancy induced hypertension among pregnant women receiving antennal care service was 36(10.3%). Among pregnancy induced hypertension, preeclampsia was the most common especially among those pregnant women admitted to maternity ward. The rural residence, positive family history of chronic hypertension, positive family history of pregnancy induced hypertension, chronic renal diseases (kidney diseases) and psychological stress during pregnancy were the associated factors with pregnancy induced hypertension.
- Research Article
- Abstract
- Introduction
- Methods
- Inclusion and Exclusion Criteria
- Data Processing and Analysis
- Data Quality Control Measures
- Ethical Considerations
- Results
- Prevalence of Pregnancy Induced Hypertension
- Variables Related to Obstetric Conditions
- Medical and Family History Related Variables/Factors
- Variables Related to Personal Risks
- Association between Dependent and Independent Variables
- Discussion
- Conclusion
- Declaration
- Acknowledgement
- References
Declaration
Ethical approval and consent to participants
Written ethical approval was obtained from Jimma University, college of health science of Institutional Review Board. Permission was obtained from respective health institutions and written consent was obtained from pregnant mother attending antenatal care service after discussing the objective of the study. And also we attached the ethical declaration letter at the annex of this manuscript.
Availability of data and material
The data set during the current study is available from the corresponding author on reasonable request.
Funding
The budget of this study was funded by Jimma University and the researchers of Jimma University and Mizan-Tepi University participated on this study from proposal development, data collection and analysis, and writing the manuscript.
Authors’ contribution
T A, TB and SB were developed a concept of research work, proposal development, data collection, analysis, writing findings. All authors read and approved the final manuscript.
- Research Article
- Abstract
- Introduction
- Methods
- Inclusion and Exclusion Criteria
- Data Processing and Analysis
- Data Quality Control Measures
- Ethical Considerations
- Results
- Prevalence of Pregnancy Induced Hypertension
- Variables Related to Obstetric Conditions
- Medical and Family History Related Variables/Factors
- Variables Related to Personal Risks
- Association between Dependent and Independent Variables
- Discussion
- Conclusion
- Declaration
- Acknowledgement
- References
Acknowledgment
We would like to express our deepest gratitude to Jimma University, College of Public Health for financially supporting us. Our appreciation also goes to our data collectors, supervisors, Jimma town health facilities and study participants for their valuable contribution in the realization of this study.
- Research Article
- Abstract
- Introduction
- Methods
- Inclusion and Exclusion Criteria
- Data Processing and Analysis
- Data Quality Control Measures
- Ethical Considerations
- Results
- Prevalence of Pregnancy Induced Hypertension
- Variables Related to Obstetric Conditions
- Medical and Family History Related Variables/Factors
- Variables Related to Personal Risks
- Association between Dependent and Independent Variables
- Discussion
- Conclusion
- Declaration
- Acknowledgement
- References
References
- Kacica M, Dennison B, Aubrey R,Kus C,White J, et al. (2013) Hypertensive disorders in pregnancy guideline summary. New York state department of health.
- Aghajanian PP, Ainbinder S, Andrew E (2006) Current Diagnosis and Treatment in Obstetrics and Gynecology, the McGraw-Hill.
- Aline CJ (2009) Maternal bloods lead levels and the risk of pregnancyinduced hypertension. Environmental Health Perspectives 117: 10- 1526.
- Shaman A (2010) Management of pregnancy induced hypertension. Int J of research in Ayurveda and pharmacy1(2): 390-398.
- Bethesda M (2000) Report of the National High Blood Pressure Education Program working group on high blood pressure in pregnancy. Am J Obstet Gynecol 183(1): S1-S22.
- Ojodun O, Villiers PD (2010) The prevalence of hypertensive complications of pregnancy in Dora hospital, Port Elizabeth, Eastern Cape.
- Dolea C, Abou ZC (2003) Global burden of hypertensive disorders of pregnancy in the year 2000, Evidence and Information for Policy (EIP), World Health Organization. Geneva, Switzerland.
- Parveen N, Haider G, Shaikh IA, Ujjan ID (2009) Presentation of Predisposing Factors of Pregnancy Induced Hypertension at Isra University Hospital, Hyderabad. Jlumhs08(03).
- Abeysena C, Jayawardana P, Seneviratne RA (2010) Effect of psychosocial stress on maternal complications during pregnancy. A cohort study. Int. J. of Collaborative Research on Internal Medicine and Public Health 2(12): 436-448.
- Landsbergis PA, Hatch MC (1996) psychological work stress and pregnancy induced hypertension. Journal of Epidemiology7, (4): 346- 351.
- Moodey J (2004) Maternal death associated with hypertensive disorders of pregnancy: A population based study. Hypertension in pregnancy23(3):247-256.
- CSA [Ethiopia] and ICF International (2011) Ethiopia demographic and health survey report. Addis Ababa, Ethiopia .and Calverton, Maryland, USA: Central Statistical Agency and ICF International; 2012.
- Berhan Y, Berhan A (2014) Cause of maternal mortality in Ethiopia: a significant decline in abortion related death.
- Ethiop J Health Sci 24(suppl): 15-28.
- Maria S, Vasconcellos J (2008) Pregnancy-induced hypertension and the neonatal outcome. Acta Paul Enferm 21(1):53-58.
- Kilembe DF, Hussain A, Pedersen BS (2008) Hypertensive disorders of pregnancy: Prevalence, Maternal Complications and Perinatal Outcomes at Lilongwe Central Hospital, Malawi.
- Waugh J, Halligan A, Shennan A (2000) Ambulatory monitoring and self-monitoring of blood pressure during pregnancy. Blood Pressure Monitoring 5(1): 3-10.
- Center for Disease Control and Prevention (CDC) (2009) Pregnancy Risk Assessment Monitoring System, Phase 6 Core Questionnaire.
- Duley L (2012) Maternal mortality associated with Hypertensive Disorders of Pregnancy in Africa, Asia, Latin America and the Caribbean. Br Obstet Gynecol99(7): 547-553.
- Osungbade KO, Ige OK (2011) Public Health Perspectives of Preeclampsia in Developing Countries. Implication for Health System Strengthening. Journal of Pregnancy, p. 6.
- Khosravi S, Dabiran S, Lotfi M, Asnavandy M (2014) Study of the Prevalence of Hypertension and Complications of Hypertensive Disorders in Pregnancy. Open Journal of Preventive Medicine4(11): 860-867.
- Sajith M, Vandana NV, Modi A,Sumariya R, Pawar A, et al. (2014) Incidence of pregnancy induced hypertension and prescription pattern of antihypertensive drugs in pregnancy. IntJof Pharma Sciences and Research5(4): 163-170
- Teklu S, Gaym A (2006) Prevalence and clinical correlates of the hypertensive disorders of pregnancy. Ethiop Med J44(1): 17-26.
- Wolde Z, Segni H, Woldie M (2011) Hypertensive Disorders of Pregnancy in Jimma University Specialized Hospital.Ethiop J Health Sci21(3): 147-154.
- Middendorp VD, Asbroek TA,Bio YF, Edusei A (2013) Rural and urban differences in blood pressure and pregnancy-induced hypertension among pregnant women in Ghana. Global Health 9: 59.
- Mustefa R, Ahmed S, Gupta A, Venuto RC (2012) Comprehensive Review of Hypertension in Pregnancy. Journal of Pregnancy P. 19.
- Chappell LC, Enye S, Seed P, Briley AL, Poston L, et al. (2008)Adverse Perinatal Outcomes and Risk Factors for Preeclampsia in Women with Chronic Hypertension. A Prospective Study. Hypertension51(4): 1002- 1009.
- Hernandez-Diaz S, Toh S, Cnattingius S (2009)Risk of pre-eclampsia in first and subsequent pregnancies: prospective cohort study. BMJ338: b2255.
- Coussons-Read ME, Okun ML, Nettles CD (2007)Psychosocial stress increases inflammatory markers and alters cytokine production across pregnancy. Brain Behav Immun21(3): 343-350.






























