Laparoscopic Transabdominal Cerclage: Surgical Technique and Review of Literature
Andres Vigueras1*, Monica Tessman2, Ivy Quirino1 and William Kondo2
1Gynecology, Sugisawa Hospital, Brazil
2Department of Gynecology, Sugisawa Hospital, Brazil
Submission: April 05, 2018; Published: May 11, 2018
*Corresponding author: Vigueras A, Gynecology unit of Sugisawa medical center, 1236, Iguafu Avenue, Curitiba, Brazil, Tel: 41-32596500; Email: afvigueras@gmail.com
How to cite this article: Andres Vigueras, Monica Tessman, Ivy Quirino, William Kondo. Laparoscopic Transabdominal Cerclage: Surgical Technique and Review of Literature. J Gynecol Women's Health. 2018: 9(4): 555767. DOI: 10.19080/JGWH.2018.09.555767
Abstract
Objectives: To analyze the current data available about the laparoscopic abdominal cerclage as treatment for cervical incompetence.
Methods: A semantic review of literature was made of all English language publications on databases Pubmed and Google following a Mesh and key word searching. The studies were finally selected by one author according to the aim of this review.
Results: A laparoscopic cerclage is a rising technique with good obstetrical outcomes, although it has a lack of optimal quality of evidence.
Conclusion: The laparoscopic transabdominal cerclage is an option for women with cervical incompetence when transvaginal approach is not indicated. Despite the lack of good quality evidence, laparoscopy had demonstrated better obstetrical outcomes when compares to laparotomy, with all the advantages of the minimally invasive surgery and avoiding the vaginal route. Different techniques have been described and apparently there is no significant difference among them. Large analytical prospective experimental studies are required to confirm this data and to know if there is a better laparoscopic technique.
Keywords: Laparoscopic surgery; Cervical incompetence; Cerclage; Cervical insufficience; Recurrent miscarriage
Abbreviations: LAC: Laparoscopic Transabdominal Cerclage; AJOG: American Journal of Obstetrics and Gynecology; JMIG: Journal of Minimally Invasive Gynecology; NICE: National Institute of Health and Care Excellence
Introduction and History
According to the definition of the American College of Obstetricians and Gynecologists in its practice bulletin of 2014, the cervical incompetence is defined as the inability of the cervix to retain the pregnancy on the second trimester, in absence of contractions [1]. Additionally, Drakeley defined in the Obstetrics and Gynecology of 2003, as a painless dilatation of cervix resulting in bulging or ruptured membranes and a final mid trimester miscarriage [2]. Hence, the lack of a universally accepted definition and pathognomonic confirmatory diagnostic test challenges the clinical abilities for a correct diagnosis.
The cervical incompetence is present in 0.1 to 1% of all pregnancies, showing a recurrence rate of almost 30%, and constitutes about 15% of recurrent miscarriages and preterm births lower than 28 weeks [3,4]. The risk factors for this pathology are widely studied and includes congenital malformations of uterine cervix, cervical postpartum trauma, intrauterine exposure to diethylstilbestrol, mechanical dilatation of cervix, and elastin and collagen insufficiency [5-7].
There are many treatments described for this pathology nowadays, including medical (pessaries) and surgical (cerclage) options. In the surgical group the primary approach will be the vaginal route. Within this approach, many techniques has been describe but the most performed on this days are the Mcdonald and Shirodkar cerclages, generally during pregnancy.
The first cerclage ever made was described by Lash and Lash on 1955. Later Shirodkar in the Antiseptic, described his homonymous vaginal technique placing a suture high over the cervix, prior bladder reflection [8]. Afterwards in 1957, Mcdonald described in the BJOG his own technique, probably the most simple and used to date, consisting in a transvaginal approach with placement of a pursestring suture around the body of the cervix, lower than Shirodkar technique, without any dissection and leaving the knot exposed to the vagina [9].
When the usual handlings treatments for cervical incompetence (pessaries or vaginal cerclage) are failed, can't be done or when a deep cervical defect is present, the abdominal approach appears as an option to deal with the disease [6,7,10]. This transabdominal cerclage placement can be done either by laparoscopy or laparotomy methods, as well as prior or during pregnancy [11,12].
Specifically, the transabdominal approach was described firstly by Benson and Durfee in the Obstetrics and Gynecology in 1965, who places the cerclage by laparotomy prior to pregnancy [13]. Since then, the technique gain popularity and emerge as an effective and safe procedure [5,14,15]. The primary indication, as said by Novy in 1982, will be the failed vaginal cerclage in previous pregnancy. Also, is a reasonable option for cases where the vaginal approach is not feasible due the shortening or abnormal anatomy of cervix.
Classic laparotomy approach is an invasive procedure and the way of birth is mostly c- section. With the aim to avoid this two laparotomies, a laparoscopic approach for cerclage placement, described by Lesser and Childers in the Obstetrics and Gynecology 1998, could be an interesting choice [16].
With the advance in endoscopic techniques applied to laparoscopy, this approach appears to be a real therapeutic option to avoid the disadvantages of the large incisions needed in laparotomy [6]. Many techniques are described in the literature and it's necessary to know the steps, security and effectiveness of it.
Objective
To analyze the current information related to laparoscopic transbadominal cerclage as a treatment of cervical incompetence, focused on different surgical techniques described for this approach. As a secondary aim, a comparison with other surgical methods was made.
Material and Methods
A comprehensive review of literature was carried out conducting a total computerized search for all English publications on databases Pubmed and Google Scholar related to laparoscopic transabdominal cerclage (LAC) and the surgical technique. We included all studies (excluding including gray literature) found under the search of following Mesh and key words terms: laparoscopic AND cerclage OR cervical incompetence OR cervical insufficiency OR recurrent miscarriages. One author independently made a selection of relevant abstracts according the aim of this review. The primary objective of the review was to know the surgical technique, effectiveness and security of LAC. The secondary aim was to discuss this approach with other surgical methods.
The primary and secondary data of this review were recorded and tabulated uniquely by the authors in the Microsoft Excel program database. We start describing the surgical technique used in our center. After, a review of techniques variants are presented. Finally, we discuss the general and obstetrics results of LAC, and compare it with other surgical approaches.
Laparoscopic Cerclage: the Surgical Technique
Under general anesthesia and following the standard surgical and preoperative protocol of our hospital, a 8 Hegar cannula is inserted transcervical for uterine mobilization and then secured to a Pozzi clamp fixed in anterior labia of the cervix. The pneumoperitonium was created using the classic closed technique with Veress needle, with an entrance and working pressure of 20 and 12mmhg respectively. A 10mm trocar was placed intraumbilical for a 10mm zero degrees Hopkins optic. Two 5mm trocars were placed in both iliac fossas under direct vision. After complete exploration of pelvic and abdominal cavity, the procedure begins.
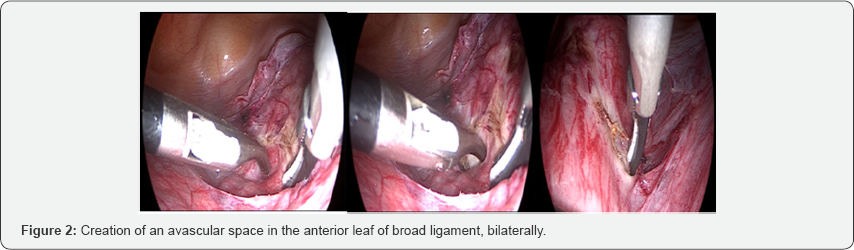
Firstly and using harmonic scalpel and graspers, the anterior peritoneal reflection is opened over the plica uterovesicalis and then extended laterally until the uterine artery could be clearly identified in both sides. Afterward, the vesicle cervical avascular space is reach before an atraumatic mobilization of the bladder.
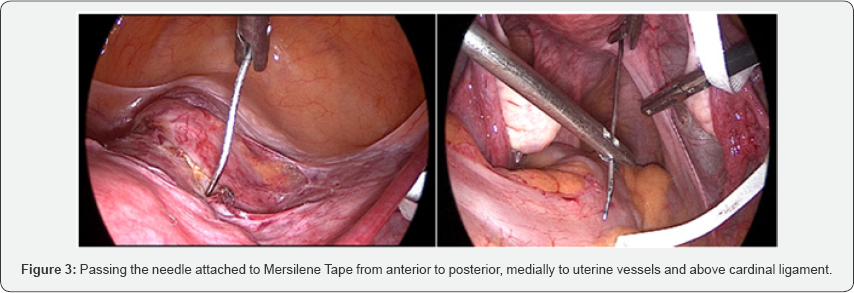
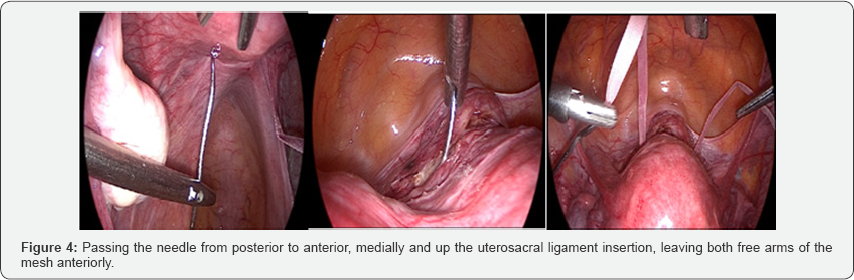
A 5mm Mersilene tape with straight needle is introduced by suprapubic trocar into abdominal cavity. Before a complete identification of uterine vessels at both sides and using atraumatic graspers, the needle is grasped on the proximal portion in a 90 degrees angle. Posteriorly and helped by a cranial and posterior uterine mobilization, the needle passes through the right broad ligament in the avascular space created on the anterior leaf, medially from the uterine artery until the tip of needle is seen in the posterior face above the uterosacral ligament. All the steps are possible by synchronic uterine mobilization. The procedure is then repeated contra-laterally following the same anatomical and technical precepts, but from posteriorly to anteriorly.
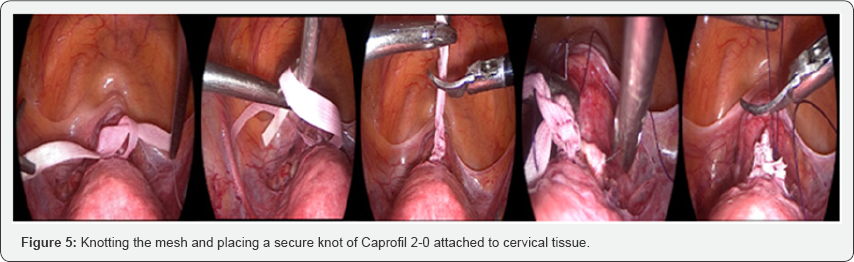
Once the position of the mesh is complete and checked, far away from ureter and medial to uterine arteries, the tape is knotted seven times anteriorly at the cervicoithsmic junction and Caprofyl 2-0 stitch is made to fix the knot and left it horizontally.
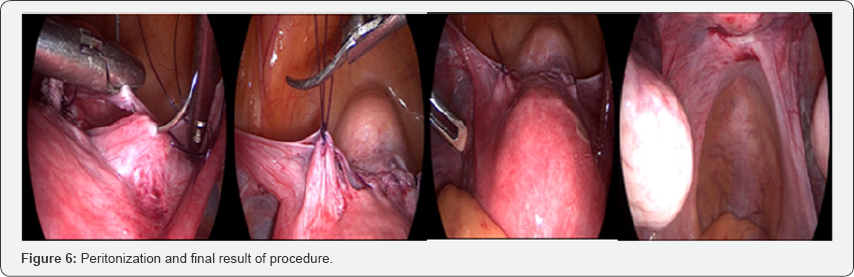
Finally, the procedure is ended with the anterior peritonization, covering all the plica uterovesicalis and the mesh, leaving completely extra peritoneal. The principal steps of the surgery are shown in Figures 1- 6: A good visualization of the vessels is essential in LAC, which could be garanteed by following an anterior to posterior approach starting with the opening of the plica uterovesicalis, continuing through the broad ligament in the avascular space medially from the uterine artery and ending above the uterosacral ligaments.

Variations in Surgical Technique for Lac
Broadly talking, the primary outcome of the surgery and no matter the technique that is applied, the placement of a specific tape medially to uterine artery and upper to cardinal and uterosaccral ligaments in the right cervico isthmic level brings the best results. This is difficult to achieve by the vaginal way and generally needs major surgical dissections. Besides, when laparoscopy is used, the dissection and surgery itself becomes easily and avoiding the vaginal exposure, fact that theoretically could reduce the risk of surgical site infections [17].
Commonly, the cerclage placement does not represent a difficult procedure, but in cases when the anatomy is changed or loss due to previous surgeries and or pregnancy, the technique becomes more arduous. Many materials have been described and used to perform it, usually a large needle attached to a Mersilene, Prolene or other polyester-component tape. It is then passed through a non-sharp tunneling in broad ligament, lateral to cervix, medial to uterine vessels and above uterosacral and cardinal ligaments [18,19]. These tapes usually are a typical macro-pore mesh associated with quick action and fewer risk of intra-abdominal adhesions, infections or allergic responses [4].
The technique described by the Belgium group of Marilien Gebreuers and Yves Jacquemin in the Surgical Science in 2013, is one of the most performed actually. They published their simplified technique applied in 12 patients with cervical incompetence, treated with LAC following an atraumatic dissection of tissue and a needle-removed cerclage tape, showing good obstetrics results [20]. The technique consists in a consecutive four steps procedure. Under general anesthesia, the patient is placed in dorsal litothomy, a foley catheter is placed and the uterine manipulator is inserted. Three trocars are placed, a 10mm intraumbilical and two 5mm ancillary ports in each iliac fossa. The first step is the development of paravesical and vesicovaginal spaces, helped with an injection of solution of vasopressine under the peritoneum of the uterovesical reflection and lateral to lower uterus. The next tread is the creation of a window in the broad ligament, identifying branches of uterine vessels and excluding those, for a final atraumatic perforation of an avascular area by an atraumatic grasper, medially to uterine vessels in both sides. This grasper is visually guided its way trough and perforate the posterior leaf, medial to the uterossacral ligament. The third step is the placement of the suture material through the broad ligament window - which is the major difference to the classic abdominal technique described by Al-Fadhli and Migione in the Human Reproduction of 2003. A 5mm Polyester tape without the needles is introduced to the pelvic cavity by the umbilical port and passed through the hollows created in broad ligament, leaving both free ends of the tape on the anterior side. Due the fact that the window is medially the uterosacral ligaments and a small part of cervical tissue is included in the loop, there is no need for anchoring the suture to uterus. The last stage consist in secure the cerclage to the anterior side of the uterus by three knots, resulting in a tension free loop around the cervix above the insertion of uterosacral ligaments. The close of peritoneum is dismissed and no preoperative antibiotics are used.
Kedar Jape and Phillip Rowland of the PIVET medical center in Australia, followed the same surgical principles, including the creation of a 5 to 6mm avascular plane in both sides of broad ligament. They reflect the bladder caudally after opening the utero vesical fold. The main difference came when they left the free ends of the Mersilene tape laying posteriorly at the level of sacral crus. Following, intracorporeal knots are made at the posterior aspect of uterus. Before the end of the procedure, ureteric vermiculation and well perfused uterus are always checked [17].
Feys, in the Journal of clinical case report of 2015, described his experience following the classic technique of Gebreuers. The initial steps of establishing pneumo peritoneum and trocar placement are similar to operative laparoscopy. According to Grebauers technique, a solution of vasopresine is administrated under the peritoneum of utero vesicle reflection prior any dissection. Then, branches of uterine artery and vein are identified, allowing the perforation of the cardinal ligament from anterior to posterior in an avascular area, on the median side of the uterine vessels. Straight atraumatic clamp is employed, avoiding the use of large needles into abdominal cavity. They left both free ends of tape at anterior side of uterus and perform three knots leaving a tension-free tape. They do not close the peritoneum over the knot [21].
Following the same surgical rules for LAC, Tawde explained her technique in a case report of 2016. She introduced a Mersilene tape posteriorly to anteriorly, specifying that this enter has to be done one centimeter superiorly and laterally to the uterosacral ligaments insertion. They performed six intracorporeal knots to safe the tape, and also secured it with a final Vicryl 2-0 stitch. A visual confirmation of the correct tape position on the posterior aspect is always realized prior finish.[22] Pawel also followed the classical steps of the procedure, related to establish pneumoperitoneum following closed Veress technique, port placement for operative laparoscopy, development of avascular area over anterior leaf and anterior to posterior pass of a Mersilene tape. They left both free ends of tape and knotted anteriorly. The additional movements that they perform are placing a knot in the posterior part of isthmus to stabilize the cerclage and leave a 500cc of ringer solution in the peritoneum cavity. They forsake the tape in the isthmus for subsequent pregnancies, always covered by peritoneum [5].
There is another device used to perform a LAC called the “Goldfinger” device of Ethicon End surgical, originally designed to place laparoscopic gastric bands and carry out distal Pancreatectomies. It is a flexible tip and blunt end instrument that gave the surgeon an easy pass between structures, reducing the risk of damage adjacent tissues. In 2015 Bolla published 18 cases treated with Goldfinger, reporting a mean surgical time of 55 minutes, with no serious intra or postoperative complications. All patients were discharged within three days post operatory and 91% of term deliveries without complications were obtained [23,24].
Discussion
Cervical incompetence is widely accepted as a cause of preterm birth and recurrent miscarriages in the first or second trimester and the current treatment for this disease is the cervical placement of a cerclage. [10,11,25]. Generally talking and no matter the approach selected, cerclage can be placed previously or during pregnancy, mostly between 12 to 16 weeks. The benefits of this performance in a non pregnant state is the less bleeding, less maternal and fetal risk, the better uterus manipulation and to avoid technical difficulties due the enlargement gravid uterus or other anatomical variations[15.20] . Furthermore, the use of a Hegar 8 or similar for uterine manipulator, enables better control in the force and the tying of the knots placed on cervix, providing the right tension in tape. Despite the absence of large prospective analytical experimental studies comparing the better moment to place it, most authors agree to perform it before the pregnancy to avoid the risks previously stated [24,26].
The indications for a transabdominal cerclage prior pregnancy will be the agenesis, lacerate or extreme shortening of the cervix and failed previous vaginal cerclage [5,6,11,27,28]. This abdominal approach let to attach the tape higher, in the upper part of cervical isthmus. Specifically to laparoscopic method and according to Ades in the JMIG of 2015, the indication will be the clear diagnosis of cervical incompetence, associated with: previous failed transvaginal cerclage, irregular cervix anatomy, fore shortened cervix due LEEP biopsy or similar [29].
When the efficacy of transabdominal and transvaginal prophylactic cerclage is compared in patients with failed transvaginal cerclage, Davis and Berghella found in their retrospective cohort, a significant higher rate of deliveries after 33 weeks in the transabdominal group (90% vs 62%) [30]. Despite the arduous technique required in this approach, some interesting intrinsic advantages as a lack of foreign body inside the vagina, absent of mesh slippage (reducing potential migration due the proximal placement) and high placement of the suture are also found.
Now, even when laparoscopic procedure requires expertise in general laparoscopy and laparoscopic suture, clear benefits in terms of less or no hospitalization, less postoperative pain and faster recovery are obtain [20] Moreover, laparoscopic itself has less membranes rupture and chorioamnionitis rate.[6.15.20] . Regardless of the absence of large series studying the transabdominal cerclage and its approach, it is accepted that bleeding and the indication of c-section for delivery are the main problems of this technique. The C-section can be avoided in cases of first trimester miscarriage and late second trimester fetal loss, where laparoscopic removal of cerclage can be done [24,31].
Despite the fact that the laparoscopic procedures are still relatively infrequent, when compared to other approaches, many studies report encouraging results [3,6,7,28]. Its seems that this procedure has at least equal results in terms of complications rate and final obstetric outcomes. Wittle, in the AJOG of 2009, reported general and obstetrics outcomes in 65 LAC and compared these results with classical laparotomy studies previously published. No differences in terms of perioperative complications and obstetrical outcomes were found, with 89% of births and mean gestational age of 35 weeks in both approaches. Also, among the seven laparoscopic cerclage performed, five required conversion to laparotomy due uterine vessels bleeding [23] . In another cohort study of 19 patients treated with LAC and compared to an historical control group of patients who underwent to laparotomy, the author found equal pregnancy rate (75%) and concluded that laparoscopic approach is an effective alternative to laparotomy in patients with indication of abdominal cerclage [32].
In August 2007, the Royal College of Obstetrics and Gynecology published a NICE green top guidance of laparoscopic cerclage for prevention of recurrent pregnancy loss due the cervical incompetence. Explicitly, guideline recommend the closed technique for pneumoeritonum under general anesthesia, during or prior pregnancy. The use of an uterine manipulator is preferred in non pregnant woman. The technique itself must incorporate the dissection and mobilization of the bladder away from uterus and a ligature mesh secured around cervical isthmus above cardinal and uterosacral ligaments. Since removing suture vaginally is practically impossible and has to be avoided, they counsel a cesarean section delivery for all transabdominal cerclages, either laparotomy or laparoscopy performance. In cases of early miscarriages, there is no problem to leave the tape placed while performing dilatation and curettage.
Concerning to safety and efficacy issues, the information came mostly from small case series fewer than 40 patients each, and they advise about this lack of evidence. Two case series with a total of 32 pregnancy treated with LAC and followed until delivery reports a live birth rate between 83 to 95%, with a 70% final term deliveries. Among 35 pregnancies coming from three cases series, the rate of uterine injuries reported extended from 5% to 33%, with one case of small bowel damage and subsequent pelvic abscess. The mean operating time was 68 minutes, with an average blood loss fewer than 40cc. This guide was updated in 2011 considering 13 case series and one controlled non randomized study, giving equal recommendations. The final statement was that there is no evidence to support laparoscopy over laparotomy for the insertion of abdominal cerclage, but it is still a level III recommendation [33].
In 2013, seventeen studies mostly restrospective and case series, with a total of 360 patients treated evaluated the prophylactic abdominal cerclage before or during pregnancy, either laparotomy and laparoscopy. Related to the laparoscopic, ten retrospective cohort and small series with a total of 130 patients reported the obstetrical outcomes. A seventy-five to 100% of live born infants and a 89 to 100% of deliveries above 34 weeks were obtained [20].
Finally, two recent systematic reviews have been published. Tulandi on the JMIG in 2014, including 678 abdominal cerclages from 16 studies, concluded that the rate of live births and third trimester deliveries after LAC were higher than those performed by laparotomy. Additionally, he recommends performing it prior pregnancy whenever possible [34] Later in the JMIG of 2017, Moawad published a systematic review including 41 studies and 1844 patients, 1116 submitted to a laparotomic and 728 to laparoscopic abdominal cerclage. In terms of obstetrical outcomes, the laparoscopic group showed a higher rate of deliveries upper to 34 weeks (82.9 vs 76%) and a lower rate of deliveries at gestational age of 23 to 33 weeks. Beside, LAC has fewer second trimester losses when compares to laparotomy (3.2% vs 7.8%). Authors concluded that laparoscopic approach offers not only the benefits of minimally invasive surgery, but also better obstetrical outcomes [35].
The use of robotic is clearly less used and more expensive than others, but providing all the advantages of robotics in terms of degrees of motion and depth of perception. The final choice between laparotomy or laparoscopy in the abdominal procedures has to be made considering the own center sources (instrumental-medical formation), knowing that greater part of studies evidenced that laparoscopy shown at least equal success rate in obstetrics outcomes with all advantages of a minimally invasive technique in terms of less postoperative pain, need of drug administration, shorter hospitalization and fewer risks of adhesions. Despite the approach, the pregnancy termination after abdominal cerclage usually is a cesarean section, always performed before labor at 38 to 39 weeks.
Conclusion
To date, the lack of good evidence, provided mostly by small case series and retrospective data, hinder the final evaluation of efficacy, security and obstetrics results of LAC procedures for treatment of cervical incompetence. Regardless the surgical method selected, the laparoscopic cervical cerclage placed prior pregnancy is a real, feasible and non inferior choice when compared to a vaginal or laparotomy approach.
Finally, we believe that the best understanding of the pathology and specific surgical technique by whole surgical team, will be fundamental to maximize the benefits of the surgical act. In the future, it will be necessary to confirm the profits of the laparoscopic method through large-scale randomized studies with adequate follow-ups.
References
- American College of Obstetricians and Gynecologists (2014) ACOG Practice Bulletin No.142: Cerclage for the management of cervical insufficiency. Obstet Gynecol 123(2 pt 1): 372-379.
- Drakeley AJ, Roberts D, Alfirevic Z (2003) Cervical cerclage for prevention of preterm delivery: Meta-analysis of randomized trials. Obstet Gynecol 102(3): 621-627.
- Al-Fadhli R, Tulandi T (2004) Laparoscopic Abdominal Cerclage. Obstetrics & Gynecology Clinics of North America, 31(3): 497-504.
- Pawel P, Wojciech O, Andrzej M (2009) Laparoscopic abdominal cercical cerclage before conception- case report. Ginekol Pol 80(12): 949- 952.
- Groom K, Jones B, Edmonds DK, Bennett PR (2004) Preconception transabdominal cervicoisthmic cerclage. Am J Obstet Gynecol 191(1): 230-234.
- Mingione M, Scibetta J, Sanko S (2003) Clinical outcomes following interval laparoscopic transabdominal cervico-isthmic cerclage placement: case series. Hum Reprod 18(8): 1716-1719.
- Gallot D, Savary D, Laurichesse H (2003) Experience with three cases of laparoscopic transabdominal cervico-isthmic cerclage and two subsequent pregnancies. BJOG 110(7): 696-700.
- Shirodkar VN (1955) A new method of operative treatment for habitual abortion in the second trimester of pregnancy. Antiseptic 52: 299-303.
- McDonald IA (1957) Suture of the cervix for inevitable miscarriage. J Obstet Gynaecol Br Emp 64(3): 346-350.
- Krasomski G (2006) Obstetrics outcome and nervesstate women after transabdominal isthmocervical cerclage. Ginekol Pol 77: 614-616.
- Daskalakis G, Papantoniou N, Mesogitis S, et al. (2006) Management of cervical insufficiency and bulging fetal membranes. Obstet Gynecol 107(2 pt 1): 221-226.
- Darwish A, Hassan Z (2002) Feasibility of laparoscopic abdominal cerclage in the second trimester. Gynaecol Endosc 11(5): 327-329.
- Benson RC, Durfee RB (1965) Transabdominal cervicouterine cerclage during pregnancy for the treatment of cervical incompetency. Obstet Gynecol 25: 145-155.
- Anthony GS, Walker RG, Cameron AD, Price JL, Walker JJ, et al. (1997) Transabdominal cervico-isthmic cerclage in the management of cervical incompetence. Eur J Obstet Gynecol Reprod Biol 72(2): 127130.
- Lotgering FK, Gaugler-Senden IP, Lotgering SF, Wallenburg HC (2006) Outcome after transabdominal cervicoisthmic cerclage. Obstet Gynecol 107(4): 779-784.
- Lesser KB, Childers JM, Surwit EA (1998) Transabdominal cerclage: a laparoscopic approach. Obstet Gynecol 9(5 pt 2): 855-856.
- Jape K, Rowlands P, Yovich J (2001) Preconception laparoscopic cervical cerclage: The preferred technique for cervical incompetence?” JFIV Reprod Med Genet 6: 4s1.
- Luo L, Chen SQ, Jiang HY, Niu G, Wang Q, et al. (2014) Successful treatment of cervical incompetence using a modified laparoscopic cervical cerclage technique: a cohort study. Eur J Obstet Gynecol Reprod Biol 179: 125-129.
- Ades A, May J, Cade TJ, Umstad MP (2014) Laparoscopic transabdominal cervical cerclage: a 6-year experience. Aust N Z J Obstet Gynaecol 54(2): 117-120.
- Gebreuers M, Jacquemyn Y, Cornette J (2013) Laparoscopic transabdominal cerclage. Surgical Science 4: 231-235.
- Feys S, Faes E, Leroij Y, Jaquemyn Y (2015) Laparoscopic placement and removal of abdominal cerclage: a case report. J Clin Case Rep 5: 11.
- Tawde S, Bavishi H, Bavishi HF, Bavishi P (2016) Laparoscopic cerclage in a patient of cervical incompetence. J Clin Gynecol Obstet 5(4):129- 130.
- Whittle WL, Singh SS, Allen L, Glaude L, Thomas J, et al. (2009) Laparoscopic cervico-isthmic cerclage: surgical technique and obstetric outcomes. Am J Obstet Gynecol 201: 364.e1-364.e7.
- Bolla D, Raio L, Imboden S, Muller MD (2015) Laparoscopic cercalge as a treatment option for cervical insufficiency. Geburtsh Frauenheilk 75(8): 833-838.
- Scarantino S, Reilly J, Moretti ML, Pillari VT (2000) Laparoscopic removal of a transabdominal cervical cerclage. Am J Obstet Gynecol 182(5): 1086-1088.
- Burger NB, Einarsson JI, Brolmann HA, Vree FE, McElrath TF, et al. (2012) Preconceptional laparoscopic abdominal cerclage: a multicenter cohort study. Am J Obstet Gynecol 207(4): 273.e1-273.e12.
- Theobald VP (2002) Laparoscopic cerclage of the isthma. J Gynecol Obstet Biol Reprod 31(3): 273-275.
- Reid G, Wills H, Shukla A, Hammill P (2008) Laparoscopic transabdominal cervico-isthmic cerclage: A minimally invasive approach. Aust N Z J Obstet Gynaecol 48(2): 185-188.
- Ades A, Dobromilsky KC, Cheung KT, Umstad MP (2015) Transabdominal Cervical Cerclage: Laparoscopy versus Laparotomy. J Minim Invasive Gynecol 22(6): 968-973.
- Davis G, Berghella V, Talucci M, Wapner RJ (2000) Patients with a Prior Failed Transvaginal Cerclage: A Comparison of Obstetric Outcomes with Either Tansabdominal or Transvaginal Cerclage. American Journal of Obstetrics & Gynecology 183(4): 836- 839.
- Cho CH, Kim TH, Kwon SH et al. (2003) Laparoscopic transabdominal cervicoisthmic cerclage during pregnancy. J Am Assoc Gynecol Laparosc 10(3): 363-366.
- Carter J, Soper D, Goetzl L, Dorsten PV (2009) Abdominal Cerclage for the Treatment of Recurrent Cervical Insuffficiency: Laparoscopy of Laparotomy? American Journal of Obstetrics & Gynecology 201(1):e1-111.e.
- Royal College of Obstetricians and Gynaecologists guidelines (2011) Cervical cerclage, Green top guideline number, p. 60.
- Tulandi T, Alghanaim N, Hakeem G, Tan X (2014) Pre and post- conceptional abdominal cerclage by laparoscopy or laparotomy. J Minim Invasive Gynecol 21(6): 987-993.
- Moawad GN, Tyan P, Bracke T, Khalil AED, Vargas V, et al. (2017) Systematic Review of Transabdominal Cerclage Placed via Laparoscopy for the Prevention of Preterm Birth. J Minim Invasive Gynecol 25(2): 277-286.






























