Macrosomia: Obstetric and Perinatal Complications
Kuznetsova O*, Kerchelaeva S, Zarubeeva E, Meshcherin V and Kavalgi O
Department of obstetrics and gynecology, Pirogov Russian National Research Medical University, Russia
Submission: February 02, 2018 ; Published: February 27, 2018
*Corresponding author: Kuznetsova O, Department of obstetrics and gynecology, Pirogov Russian National Research Medical University, Russia, Email: doctor_oljal973@mail.ru
How to cite this article: Kuznetsova O, Kerchelaeva S, Zarubeeva E, Meshcherin V, Kavalgi O. Macrosomia: Obstetric and Perinatal Complications. J Gynecol Women�s Health 2018; 8(4): 555745. DOI:10.19080/JGWH.2018.08.555745
Abstract
The purpose of the study: To carry out a retrospective analysis of pregnancy and childbirth as well as perinatal outcomes when macrosomia.
Material and methods: An analysis was conducted of 110 stories of birth and babies. It include 80 stories of the birth and development of the newborn with a macrosomia (main group) and 30 stories of birth and stories of infants with normal weight newborns (control group) for the year 2016.
Results: Cases with emergency operative delivery was performed significantly more often in the main group and in the structure of indications to cesarean section clinically narrow pelvis was leading. The total duration of delivery in the studied groups had no significant differences. However, second period was longer in the 1st group. In the structure of pregnancy's complications in the main premature rupture of membranes is leading. Birth injuries in the form of rupture of the perineum I-II. in the 1st group are met significantly more often. Also episiotomy has been made significantly more often in first group. Birth injuries were recorded only in group 1: fractured clavicle, facial nerve paresis, neurological disorders. Weight of newborns with perinatal complications exceeded 4300g.
Conclusion: Pregnancy, childbirth and the puerperium with macrosomia have higher risks of obstetric and perinatal complications, which increases the frequency of operative delivery, birth trauma. Prevention of the macrosomia and obstructed complications during the pregnancy, childbirth and the neonatal period justified take its place in the structure of the priority tasks of perinatal obstetrics and in research, the findings of which should be reflected in the clinical recommendations for healthcare practice.
Introduction
The priority task of modern obstetrics is to reduce perinatal morbidity and mortality. Any complication of pregnancy and the pathology of fetal development pose difficult problems for specialists, which, as a rule, require an emergency solution.
The perinatal risk group includes pregnant women with a large fetus. According to some authors, the frequency of occurrence of macrosomia in Russia is about 12.7-15% of cases [1,2], in world statistics the frequency of large fruit varies in the range from 2.5% to 20.7% of cases [3].
High rates of birth trauma of the mother and fetus are not only of medical importance, but also social. Labor with a large fetus increases both obstetric [4] and perinatal risks [5,6]. It has been proved that in newborns weighing more than 4000 grams, born through natural birth canals, such violations as cerebrovascular accidents, damage to the brachial plexus are more often observed [7-9].
The course of pregnancy and childbirth with macrosomia in the literature is assessed ambiguously. According to the published studies, the course of pregnancy with a large fetus is often accompanied by a threat of abortion, polyhydramnios, anemia, preeclampsia, labor is complicated by the weakness of labor, usually secondary, birth trauma, mismatch in the size of the fetus in the pelvis of the mother, dystocia of the shoulders. The postpartum period, respectively, is threatened with hypotonic bleeding and the development of purulent-septic complications [4,10].
It is also obvious that the presence of a large fetus increases the frequency of surgical intervention both in childbirth and in the postpartum period, which in turn leads to anesthetic risk and the risk of surgery itself. The frequency of the clinically narrow pelvis is in the range from 1.4 to 8.5% of cases to the total number of births, and in the structure of births with a large fetus is from 5.8 to 60% of cases [9,11].
The dilemma in practical obstetrics remains the diagnosis of macrosomy and the tactics of giving birth in this pathology [4,12].
The purpose of this study was to conduct a retrospective analysis of the course of pregnancy and childbirth, as well as perinatal outcomes in macrosomia.
Material and Methods of Investigation
We conducted a retrospective analysis of 110 birth and newborn histories, including 80 birth and development histories of a newborn with a large fetus (the main group) and 30 birth histories and development histories of a newborn with a normal body weight of the newborn (control group) for 2016 at the clinical base of the department "Maternity home number 10”, branch number 1 of the Center for Advanced Research. In the control group, patients were selected without chronic extragenital pathology and with a relatively physiological course of pregnancy and childbirth.
Results of the Study and Discussion
The age of the patients we examined in the 1 st group ranged from 19 to 44 years, the average age was 30±1.7 years, in the 2nd group it ranged from 18 to 34 years, the average age was 26±1.2 years.
Having studied the anamnesis of the examined patients, we did not determine the dependence of the influence of harmful production factors and living conditions on the course of pregnancy in both groups. However, it should be noted that in the 1st group, non-working patients accounted for 29.6% (37 patients), in the second group of such patients there were 10% (3 patients) (p<0.05), among working patients equally there were occupations from the fields of health, education and record keeping - 13.4%; 12.7% and 14.6% of cases, respectively .
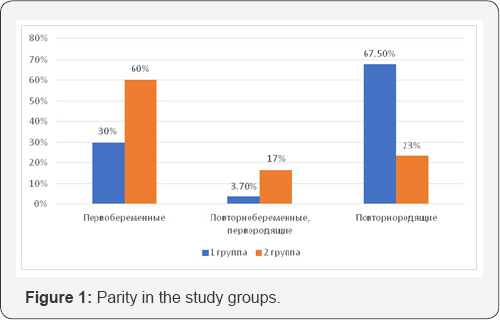
In the main group, the number of first-borns was 19.2% (24 patients), re-pregnant, primiparous - 3.7% (3 patients) and maternity patients - 67.5% (54 patients), of which high parity (4 or more births) - 9.2% (5 patients), in the control group, respectively 60% (18 patients), 16.6% (5 patients) and 23.3% (7 patients). In the control group, pregnant women with high parity were not. Reliably more often, the mating was observed in the main group in comparison with the control group (p<0.05) ( Figure 1).
In the main group, 11 patients had a major fetal history among the maternity patients, which was 13.75%.
Thus, in the main group, there were significantly more recurrent patients compared to the control group, and births of newborns weighing more than 4000g in the history were noted only in the 1st group.
Studying the hereditary history, in pregnant women of the 1st group, we detected type II diabetes in 6.2% of cases and arterial hypertension in 3.7% of cases, in the 2nd group the hereditary anamnesis according to the nosologies was not burdened.
The body mass index (BMI) in the main group was 26.4±4.5 kg/m2, in the control group - 22.3±4.2kg/m2, while the pregnant women with the initial normal BMI in the control group were 82.2 %, against 52.5% in the main, which corresponds to the data of earlier studies [4,13].
Analysis of the course of this pregnancy in groups did not reveal significant differences during the first trimester of pregnancy. The structure of complications of pregnancy in the second and third trimesters of pregnancy in groups had significant differences (Figure 2). For example, in the main group, preeclampsia occurred in 21.25% (17 cases) versus 9.9% (3 cases) in the control group (p <0.05). This fact is explained by the presence of constitutional features of the patients of the main group, in 47.5% of pregnant BMI before pregnancy indicated the presence of excess weight.
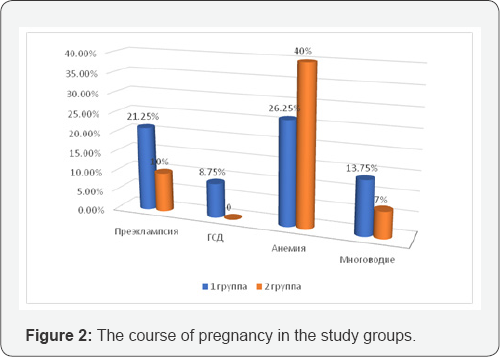
Only in the main group was revealed gestational diabetes mellitus, adjusted by dietary therapy in 8.75% (7 cases), which corresponds to the literature data [9]. Gestational pyelonephritis and gestational hypothyroidism with drug compensation complicated the course of pregnancy in group 1 with the same frequency of occurrence in 5 cases, which was 4%.
Anemia complicated the course of pregnancy of both groups, but more often it was found in the control group - 39.96% (12 pregnant women), in the main group - 26.25% (21 pregnant).
Polyhydramnios were significantly more often noted in the main group - 13.75% (11 cases), in the control group - 6.7% (2 cases) (p<0.05). The combination of polyhydramnios and gestational diabetes in group 1 was observed in 4(5%) cases. Polyhydramnios in macrosomy is explained by fetal hyperglycemia, an increase in osmotic diuresis, which subsequently leads to polyuria [9] (Figure 2).
The main prevention of complications of the course of pregnancy, childbirth, and the postpartum period is the timely diagnosis of a large fetus. Diagnosis of a large fetus was based, first of all, on the data of an external obstetric examination - the calculation of the estimated weight of the fetus according to the Jordan formula (OC (cm) x VDM (cm) = PMP (g)), as well as on the basis of the ultrasound data (Hadlocka formula ). According to the literature, the error in determining the mass of the fetus during macrosomia by 200 g is according to the Jordan formula in 66.4%, and according to the US, 57.3% [4].
We did not conduct in our study a detailed analysis of errors in determining the estimated weight of the fetus. However, the diagnosis of a large fetus, exposed on the basis of an external obstetric examination, was confirmed by ultrasound in 67.5% of cases. The cases of errors in the determination of the weight of the fetus according to Jordania's formula were explained by the presence in the patients of the main group of excess body weight and / or polyhydramnios.
Delivery in time in the main and control groups is 100%, in view of the exclusion from the analysis groups of preterm labor. In the main group, spontaneous labor amounted to 71.25% (57 births), delivery by cesarean section 28.75% (23 births), in the control group deliveries through natural birth canals were 86.58% (26 births), cesarean section - 13.32% (4 genera) (Figure 3).
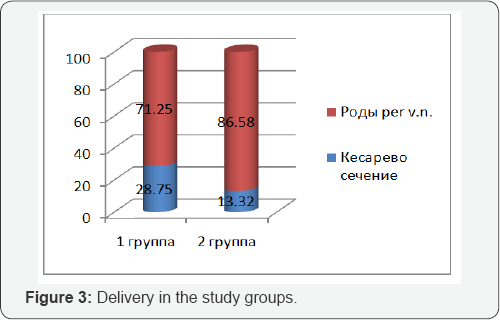
Abdominal delivery in the first order in the first group was performed in 7 patients, which was 30.43%, respectively, in urgent order in 16 parturient women (69.6%). In 8 cases, the indication for emergency delivery was a clinically narrow pelvis, in 4 cases - the weakness of labor and in 3 cases - the combination of a large fetus, premature rupture of amniotic fluid, and the “immature” cervix.
The structure of indications for planned delivery in the main group was as follows: a scar on the uterus after a caesarean section operation and combined indications (infertility, IVF, perinatal losses) - 3 cases; the weakness of labor and the tendency to overstate pregnancy (gestation period> 41 weeks, biologically “immature” cervix) - 1 case.
In the control group, abdominal delivery was planned in 3 patients (75%), the indications were: a gestation period of 42 weeks and a biologically “immature” cervix, a mixed breech presentation and an estimated fetal weight of 3800, 1 patient (25%) was urgently given birth , the indication for the operation was: acute hypoxia of the fetus. Our data confirm the literature data that macrosomia increases the rate of delivery by cesarean section. According to the literature, among the indications for abdominal delivery with macrosomia, the clinically narrow pelvis leads, in the second place - the weakness of labor activity [4,12].
The analysis of births through the natural birth canal in the study groups showed that the average length of labor in the 1st group was in the primipara 10 hours 5 minutes ±1 hour 2 min; in repetitious - 6 hours 34 minutes ±45 minutes; in the 2nd group, respectively, 9 hours 47 minutes ±1 hour 21 minutes and 6 hours 12 minutes ±1 hour 9 minutes. There were no significant differences in the total duration of labor in the study groups, however, the duration of the II stage of labor is of interest: in the first group in primiparas it was 1 hour 57 minutes ±12 minutes, in re-births 1 hour 2 minutes ±23 minutes, and in The second group in the primiparous second period of labor was 1 hour 03 minutes ±15 minutes, and in the reproducible 27 minutes ±9 minutes. From which it should be concluded that during macrosomia the second period of labor is longer in comparison with the births with a normal fetal mass, the advance of the head through the birth canal slows down in the second period, and this fact requires the obstetrician to closely monitor the woman in labor, in order to timely diagnose complications, in first of all, clinical inconsistencies.
In the structure of complications of labor in the main group, premature outpouring of amniotic fluid is the first place, registered in 15% of cases (in 12 patients), which is significantly more frequent than in the control group in 2 patients (6.6%) (p<0.05) and corresponds to the literature data [4,13]. The untimely outflow of amniotic fluid is explained by the absence of a contact belt in macrosomia. Weakness of labor in the study groups was found without significant differences: in 7(8.75%) patients of the 1st group, and in 3 (9.9%) patients of the 2nd group.
Birth traumatism in the form of rupture of the perineal I-IIst in the 1st group was significantly more frequent than in the 2nd group - 25% (in 20 parturient women) and 6.7% (in 2 parturient women), respectively (p <0.05 ). Episiotomy in the study groups was performed significantly more often in the 1st group - 28.7% (in 2 3 parturient women) than in the second group - 13.3% (in 4 parturient women) (p <0.05). Cervical rupture I-IIst met only in the main group in 3 patients, which amounted to 3.75% of cases (Figure 4).
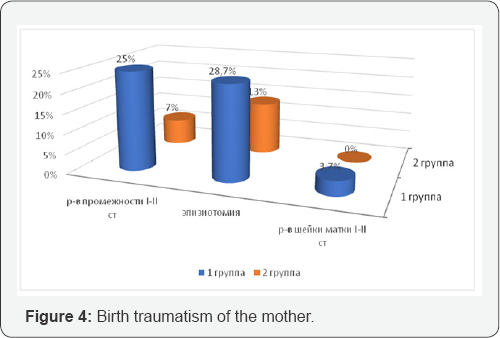
There were no cases of rupture of the uterus in the study groups, from which it should be concluded that the delivery was timely by cesarean section with a clinical mismatch in Group 1 and careful selection of patients for planned abdominal delivery, assessing risk factors in patients with macrosomia.
The volume of blood loss in the study groups did not differ significantly, but in the 1st group there was more blood loss. In childbirth through the natural birth canal, blood loss in the 1st group was: - 490ml±74.5 ml, in the second group - 284.4±54.7ml. With operative delivery, the volume of blood loss is 780±154.5ml and 620±128.5ml, respectively. There were no cases of pathological hemorrhage in both groups. Expected pathological blood loss in the main group of patients with macrosomia, but in the cases we studied, pathological blood loss during childbirth and during the operation of caesarean section was not allowed, assessing its risks and taking timely preventive measures.
In 5 patients (6.25%) of the main group in the early postpartum period, a control manual examination of the uterus was performed: for the defect of the afterbirth in 4 cases (5%) and in 1 case (1.25%) for the birth of a child in an asphyxia of the middle severity. In the control group, there were no complications of the early postpartum period.
Analyzing the course of the late postpartum period, we found that such a complication, as a lochiometer, was found only in the main group in 2 (2.5%) patients. There were no purulent-septic complications in the postpartum period in both groups, which is explained by their timely prevention.
The mass of newborns in the 1st group was 4577.5±154.2g, in the 2nd - 3585.3±270.5g, the growth was respectively 54.313±1.8cm and 50.28±2.2cm. The birth of giant fruits in the main group was not observed.
The Apgar score in the main group at the 1st minute was 7.3±0.7 points, at the 5-1 minute 8.8±0.4 points, in the control group, respectively, 9.0±0.5 and 9.5±0.7 points.
In the first group, 2 births of newborns were recorded in an average degree of asphyxia with an Apgar score of 6 points in the 1st minute and 7 points in the 5 th minute. In the first case, the parental incubation lasted 9 hours and 10 minutes, with the opening of the uterine pharynx 7cm, meconial amniotic fluid flowed, the second period of labor lasted 40 minutes, the anhydrous interval was 2 hours and 10 minutes. The weight of the child at birth was 4500g, height 55 cm., Apgar score at the 1st minute 6 points, in the 5th minute - 7 points.
The condition of the child is regarded as a severe, aspiration- induced meconial amniotic fluid, in the birth department, resuscitation was carried out, including intubation of the trachea and transfer to mechanical ventilation. The newborn on the 4th day was transferred to the Department of Pathology of Newborn Children's Hospital. Diagnosis in translation: Aspiration pneumonia. Aspiration syndrome with meconial waters. Hypoxic-ischemic lesions of the central nervous system. In the second case, the birth was also repeated, the total length of labor was 6 hours and 50 minutes, the second period of labor lasted 20 minutes. The anhydrous interval was 20 minutes. A child was born with a mass of 4380g, 52 cm, an Apgar score of 6-7 points. The condition is estimated at birth as a severe, aspiration-induced meconial amniotic fluid. The newborn was also transferred to the department of neonatal pathology. Diagnosis in translation: Aspiration pneumonia. Aspiration syndrome with meconial o/ water. Hypoxic-ischemic lesions of the central nervous system.
The syndrome of oppression
As a result of the analysis, the fact that the Apgar scale of newborns in the main group is relatively low is evident. newborns with macrosomia, which is possible due to complications of pregnancy, and complications in childbirth, which in turn increases the risk of neonatal complications.
In the main group, cases of birth traumatism such as fracture of the collarbone in 3(3.7%) and in 1 (1.25%) case - paresis of the facial nerve are noted. The above cases of fetal birth injury required the transfer to the departments of newborn pathology. Neurologic disorders in newborns were met only in the group with macrosomia - in 4 newborns, which amounted to 5% of observations. According to our observations, the mass of newborns with these perinatal complications exceeded 4300g.
In the control group, cases of asphyxia, birth trauma and neurologic disorders in newborns were not recorded.
Conclusion
Hereditary anamnesis in pregnant women of the main group is weighed down with diabetes mellitus, preeclampsia significantly more often complicated the course of pregnancy of this group, which is more likely due to constitutional features of patients of this group whose body mass index indicates excess weight. Gestational diabetes, polyhydramnios also occurred only in the main group.
Abdominal delivery for emergency indications was reliably more often performed in the main group, and in the structure of the indications for delivery the clinically narrow pelvis was leading. The total length of labor in the study groups did not have significant differences, while the second period of labor in the 1st group was longer than in the 2nd group.
Maternal traumatism occurred in both study groups. However, the rupture of the perineum I-II degree was diagnosed more reliably, and episiotomy in the main study group was performed.
The complicated course of labor causes complications in the postpartum period. There were no cases of purulent-septic complications in the groups. Lokhiometra was found only in the main group, which is due to a decrease in contractile activity of the uterus in macrosomia.
Neonatal complications, fetal birth traumatism and neurologic disorders were also significantly more frequent in the 1st group. The result of the study is the determination of the mass of the newborn in 4300 and more, at which the frequency of these complications increases.
Thus, our analysis once again showed that pregnancy, childbirth and the postnatal period with macrosomia have high risks of obstetric and perinatal complications, increase the frequency of operative delivery, birth trauma.
Prevention of a large fetus and prevention of complications of pregnancy, labor and the neonatal period in case of macrosomia justifiably occupy a niche in the structure of priority tasks of modern perinatal obstetrics and in scientific research, the conclusions of which should be reflected in clinical recommendations for practical public health.
References
- Slabinskaya TB (2003) Perinatal diagnostic criteria for macrosomia of the fetus in a modern population of pregnant women in the middle Urals: The dissertation author's abstract on the degree of candidate of medical sciences.
- Tomic V, Bosnjak K, Petrov B (2007) Macrosomia biths at Mostar Clinical Hospital: a 2-year review. Bosh J Med Sci 7(3): 271-274.
- Tcherepnin AT (2006) Large fetus: modern tactics of management of pregnancy and childbirth. Perinatal outcomes: Abstract. dis. to receive a degree of med, Russia, p. 24.
- Nikiforovsky NK, XPokusaeva VN, Stas LI (2010) Obstetric and pesrinatal outcomes with a large fetus. Russian bulletin of the obstetrician-gynecologist 1: 55-58.
- Tomic V, Bosnjak K, Petrov B (2007) Macrosomic births at mostar clinical hospital: a 2-year review. Bosnian journal of basic medical sciences 7(3): 271-274.
- Boulet SL, Alexander GR, Salihu HM (2003) Macrosomic births in the united states: determinants, outcomes, and proposed grades of risk. Am J Obstet Gynecol 188(5): 1372-1380.
- Kravchenko EN (2009) Birth trauma: obstetric and perinatal aspects. Russia.
- Vlasyuk VV (2014) Pathology of the brain in a newborn and young children. Russia.
- Mudrov VA, Mochalova MN, Ponomareva Yu N, Mudrov AA (2016) Outcomes of pregnancy and childbirth of a large fetus. Journal of Obstetrics and Women's Diseases 65(6): 36-44.
- Begova SV, Magomedova IA (2007) Perinatal outcomes in macrosomia in maternity and multiplying women. Bulletin of New Medical Technologies 14(1): 90-91.
- Chernukha EA, Volobuev AI, Puchko TK (2005) Anatomically and clinically narrow pelvis. Triada-X, Moscow, Russia.
- Lubyana SS, Manishchenkov SN (2011) Obstetrical and perinatal aspects of a large fetus. Ukrainian Journal of Extreme Medicine named after GO Mozhaev 12(4): 139-143.
- Mylnikova Yu V, Protopopova NV (2009) A large fruit. Modern tactics of management of pregnancy and childbirth. Bulletin of the Buryat State University 174-178.
- Mylnikova Yu V, Protopopova NV (2010) Modern aspects of macrosomia. Siberian Medical Journal 1: P86-P89.
- Tanysheva GA, Kinayatova Sh K, Zhelpakova MS, Sidorova OG, Abykenova LA (2016) Structure and frequency of complications of labor in macrosomia. Science and Health Care 4: S93-S103.
- Milanova K, Marinov B, Borisov I (2006) Yhe incidence of foetal macrosomia and method of delivery for a two-year period in the University Hospital of Obstetrics and Gynecology Maichin Dom-Sofia. Akush Ginekol (Sofiia) 45(6): 3-6.






























