The Relationship between Haemoglobin Concentration and Pregnancy Outcomes in Women with Pre-Eclampsia in a Tertiary Hospital in South-Southern, Nigeria
Unamba BC and Rosemary NO*
Department of Obstetrics and Gynaecology, University of Port Harcourt Teaching Hospital, Nigeria
Submission: October 14, 2017; Published: October 30, 2017
*Corresponding author: Rosemary NO, Department of Obstetrics and Gynaecology, University of Port Harcourt Teaching Hospital, Rivers state, Nigeria, Email: rosemaiy.ogu@uniport.edu.ng
How to cite this article: Unamba BC, Rosemary NO. The Relationship between Haemoglobin Concentration and Pregnancy Outcomes in Women with Pre-Eclampsia in a Tertiary Hospital in South-Southern, Nigeria. J Gynecol Women�s Health 2017; 7(2): 555713. DOI: 10.19080/jgwh.2017.07.555713
Abstract
Background: Pre-eclampsia is a multi-systemic disorder defined as hypertension with significant proteinuria occurring in the second half of pregnancy in a woman who was previously non- hypertensive and non-proteinuric. Its incidence ranges between 2% to 8% of all pregnancies worldwide and between 2% to 16.7% in Nigeria. The measurement of the haemoglobin concentration in pre-eclamptics may be of great prognostic value for the mother and the foetus. This study investigated the haemoglobin concentration in pre-eclamptics and its relationship with feto-maternal outcomes.
Methods: This cross-sectional longitudinal study included 63 pregnant women with pre-eclampsia who were between the gestational ages of 28 weeks and 41 weeks at the University of Port Harcourt Teaching Hospital (UPTH). This study population consisted of a crosssection of pregnant women with sustained elevated blood pressure and proteinuria. Haemoglobin concentrations were assayed in the UPTH Haematology laboratory. A structured questionnaire was used to obtain socio-demographic information.
Results: The mean haemoglobin concentration for the study population was 11.70±1.7g/dl. The mean haemoglobin concentration for severe and mild pre-eclampsia was 11.95±1.74g/dl and 11.39±1.69g/dl, respectively (p=0.21). Mean haemoglobin concentration for subjects who had worsening proteinuria was 12.33±1.08g/dl, while that for those without worsening proteinuria was 11.38±1.62g/dl (p=0.04), suggesting that those subjects with worsening proteinuria had higher intrapartum haemoglobin concentration than those without. Bivariate analysis showed that haemoglobin concentration and postpartum haemorrhage were significantly associated (r= -0.278, p= 0.027), even after controlling for estimated blood loss (r= -0.407, p= 0.001), suggesting that postpartum haemorrhage is likely to occur with decreasing haemoglobin concentration.
Conclusion: Postpartum haemorrhage had an inverse relationship with haemoglobin concentration suggesting that postpartum haemorrhage is likely to occur with decreasing haemoglobin concentration. Our results indicate that the maternal haemoglobin concentration is a potential prognosticator of post-partum haemorrhage in patients with pre-eclampsia. Hence, post-partum hemorrhage in women with pre-eclampsia should be anticipated especially in those with low hemoglobin concentration, and proactive measures taken to obviate the risk.
Introduction
Pre-eclampsia is one of the most common diseases worldwide [1]. It is a human-pregnancy-specific disease defined as the occurrence of hypertension and significant proteinuria in a previously healthy woman on or after the 20th week of gestation [2,3]. Worldwide, it complicates 2% to 8% of all pregnancies [14]. With other hypertensive disorders, pre-eclampsia is a leading cause of maternal foetal, and neonatal morbidity and mortality worldwide [5-7] including developing countries like Nigeria [8-10]. Worldwide, preeclampsia and related hypertensive disorders are responsible for about 50,000 to76,000 maternal deaths [11,12].
The World Health Organization (WHO) estimates its incidence to be seven times higher in developing countries than developed countries [12,13]. In Nigeria, the prevalence of preeclampsia ranges between 2% to 16.7% [13-15]. In the University of Port Harcourt Teaching Hospital, preeclampsia accounted for 3.8% of all antenatal admissions and 9.7% of all caesarean deliveries amongst booked patients [16]. Pre-eclampsia/ Eclampsia accounted for 36% of all maternal deaths in the University of Port Harcourt in 2013 and remains the highest contributor to maternal deaths [16-18]. In normal pregnancy, plasma volume increases with gestation to about 40% above pre-pregnancy levels at 30 weeks followed by a small decrease at term [19].
Red cell mass increases linearly with gestation to about 25% above pre- pregnancy levels at term [20]. Consequently, hemoglobin decreases with gestation reaching a nadir of about 15% below pre-pregnancy levels at 30 weeks [21]. The purpose of this physiological hemo dilution is to create a low- viscosity intravascular system that allows an optimal red cell circulation in the low-velocity placental circulation [22] and a low- resistance system for the maternal left ventricle to contract against. Failure to achieve this low blood viscosity milieu during pregnancy is likely to decompensate both the maternal and fetal/ placental homeostasis. It is therefore not surprising that there is an association between adverse pregnancy outcome with increasing haemoglobin levels (and thus whole blood viscosity) [23,24] and a strong correlation between the prevalence of preeclampsia and plasma volume restriction and hemorheological disorders [25,26].
Alterations of haemoglobin and erythrocytic parameters which are features of pre-eclampsia frequently manifest as increased haematocrit due to haemoconcentration [27]. So other investigators however showed that there was a reduction in hemoglobin concentration in pre-eclamptic patients when compared to their non-pre-eclamptic counterparts [28]. To date, the relationship between maternal hemoglobin concentration and feto-maternal outcomes has not been analyzed in a subset of women with preeclampsia of a distinctly African population.
Materials and Methods
This was a cross-sectional longitudinal study involving all booked pregnant women with pre-eclampsia, who presented in the antenatal clinic, antenatal wards and labour wards at the UPTH. Consecutive patients with pre-eclampsia were counseled to participate in this study, and the purpose of the study was duly explained to the participants. The minimum sample size of patients required for the study will be calculated using the method of Kish [29].
Nf = Final sample size
n = The desired sample size when population is greater than
10,000
z = The standard normal deviation, usually set at 1.96 which corresponds to 95% confidence level
p = Proportion of patients with pre-eclampsia using a prevalence of 6.5% in UPTH [30].
q = 1.0-P =1.0- 0.065 = 0.94
d = degree of accuracy required, = 0.05
N = Estimation of population size (new patients with preeclampsia managed in UPTH, Port Harcourt annually) =145 [30].
The minimum sample size is thus calculated to be 57.
Giving allowance for a 10% attrition rate, the minimum sample size for the study is therefore 63 pre-eclamptic women.
Definitions
Pre-eclampsia was defined as sustained elevated blood pressure (of equal or greater than 140/90mmhg measured on at least two occasions four to six hours apart), with proteinuria, (of 1+ or more on dipstick on at least two occasions four or more hours apart), in a pregnant woman at greater or equal to twenty weeks of gestation [31]. Eligible women were counselled to participate in the study. Informed consent was obtained and indicated on their antenatal cards.
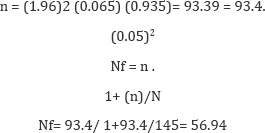
Characteristics
The 63 eligible patients recruited for the study had their sociodemographic and antenatal features such as age, parity, blood pressure, the degree of proteinuria, and antenatal complications, documented in a structured proforma. Three milliliters of venous blood samples was collected by venepuncture into EDTA and plain bottles. All blood samples were assayed for full blood count including haemoglobin concentration by the automated method with the use of an auto analyzer in the UPTH Haematology laboratory. The structured proforma for each participant was completed immediately after delivery and, the foetal and maternal outcomes such as intrapartum complications, APGAR scores, birth weight and estimated blood loss at delivery were documented. Primary postpartum haemorrhage was defied as blood loss of 500milliliters and above after vaginal delivery and 1,000milliliters and above after caesarean section within twenty- four hours [32]. In carrying out this study, confidentiality and respect for persons were considered and consent was obtained from all participants. Ethical approval was obtained from the hospital's Ethical Review Committee of the University of Port Harcourt Teaching Hospital, Port Harcourt, Rivers state, Nigeria.
Statistical Analysis
Proportions or categorical parameters were compared with the chi-square test. Relations among continuous variables were assessed using Pearson's correlation coefficient, while Spearman's correlation coefficient assessed the relations among continuous and discrete variables. The differences in all variables between groups were compared using ANOVA. The relationship between maternal haemoglobin concentration and maternal complications was determined by linear regression analysis. A p-value of less than 0.05 was considered statistically significant.
Results
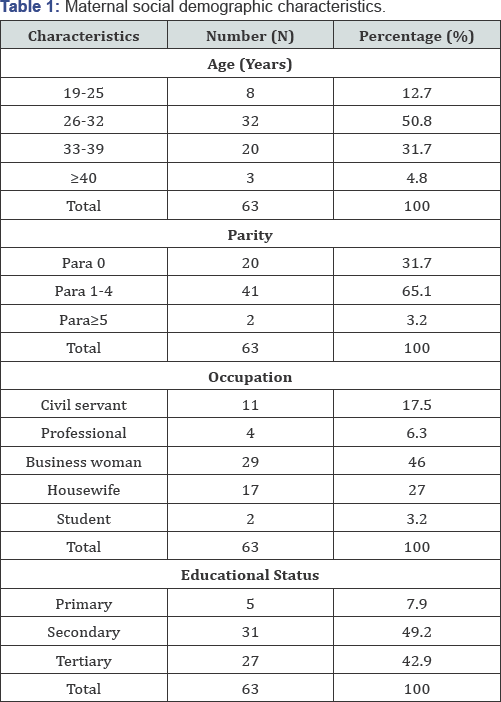
In our study, 63 women with pre-eclampsia were assessed to be eligible and recruited for the study. The maternal demographic characteristic and parity are given in (Table 1) and the mean maternal clinical characteristics in (Table 2). The mean maternal haemoglobin concentration and haematocrit levels of the study population were 11.70g/dl ±1.72 and 35.06 ±5.17 respectively The prevalence of caesarean section and vaginal delivery among the study population is shown in (Figure 1), while the mean maternal and foetal clinical characteristics with haemoglobin values with respect to severity of pre-eclampsia are shown in (Table 3).
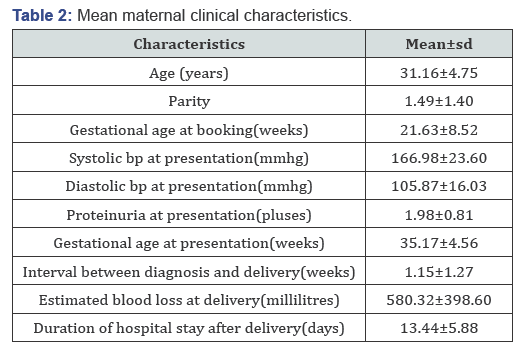
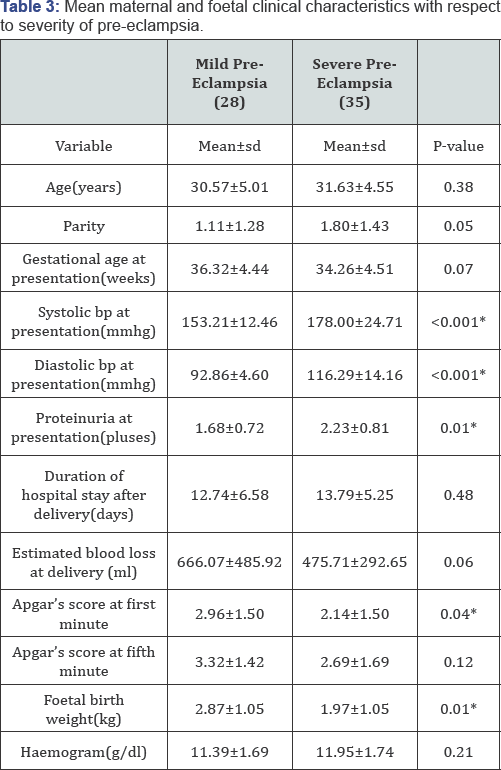
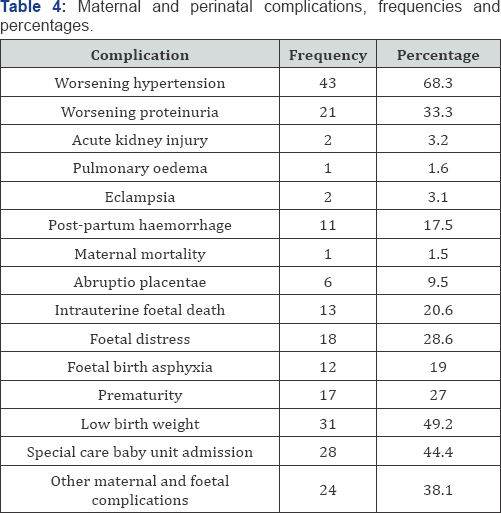
Among the population studied, 66.67% had caesarean section while 33.33% had vaginal delivery. Twenty-eight women (44.44%) had mild pre-eclampsia, while 35(55.56%) had severe pre-eclampsia. The mean haemoglobin concentration of the subjects with mild pre-eclampsia was 11.39±1.69while the mean haemoglobin concentration of the subjects with severe pre-eclampsia was11.95±1.74, p-value= 0.21.This was not statistically significant as shown in (Table 3). The maternal and perinatal complications, frequencies and percentages are shown in (Table 4). The mean haemoglobin concentration with respect to maternal and foetal complications is in (Table 5).
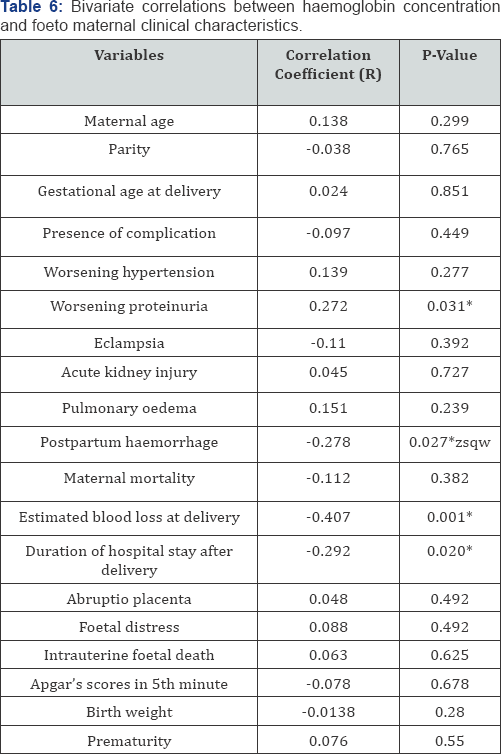
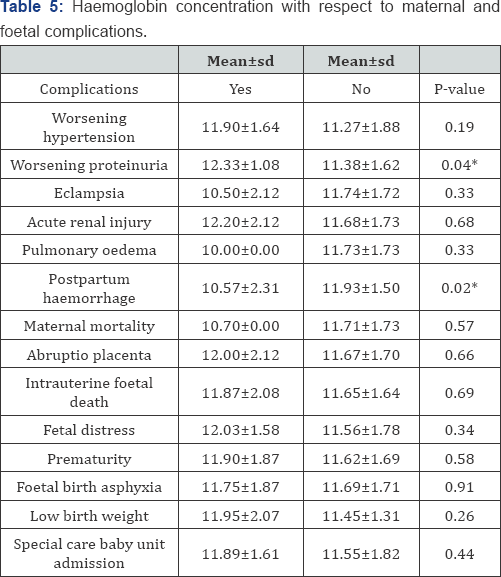
The bivariate correlation between haemoglobin concentration and foeto-maternal clinical characteristics is shown in (Table 6). Among the population studied, 92.06% of the subjects had maternal or perinatal complications while 7.94% neither had maternal nor perinatal complications. Eleven (17.5%) had postpartum haemorrhage as shown in (Table 4). The mean haemoglobin concentration of the subjects with postpartum haemorrhage was 10.57±2.31 and 11.93±1.50 for the subjects without postpartum haemorrhage, p-value=0.02 as shown in Table 5. The mean haemoglobin concentration of the subjects with worsening proteinuria was 12.33±1.08 and 11.38±1.62, p-value=0.04 as seen in (Table 5). The mean haemoglobin concentration of the subjects with maternal or perinatal complications was 11.64±1.72g/dl, while the mean haemoglobin concentration of the subjects without maternal or perinatal complications was 12.34±1.57g/dl, p=0.39. There was no statistical significance. The mean haemoglobin concentration for subjects who had caesarean section was 11.48±1.58 g/dl while the mean haemoglobin concentration for subjects who had vaginal delivery was 12.14±1.95, p=0.15.
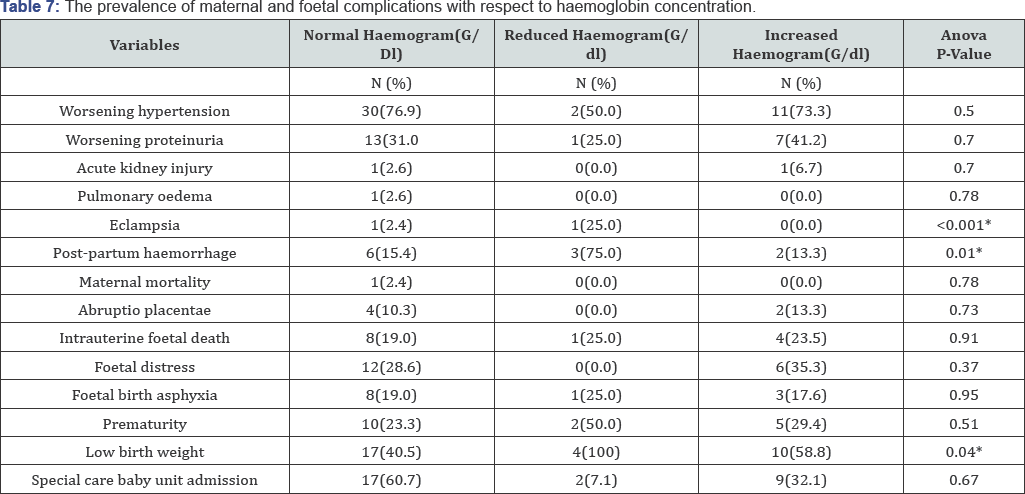
There was no statistical significance. A Bivariate correlation between haemoglobin concentration and foeto-maternal clinical characteristics shows a statistically significant direct correlation between haemoglobin concentration and worsening proteinuria and an inverse correlation between haemoglobin concentration with postpartum haemorrhage, blood loss at delivery as well as duration of hospital stay, as shown in (Table 6). The prevalence of maternal and foetal complications with respect to haemoglobin concentration category is shown in (Table 7) and the correlation between haemoglobin concentration and the severity of preeclampsia is shown in (Figure 2).
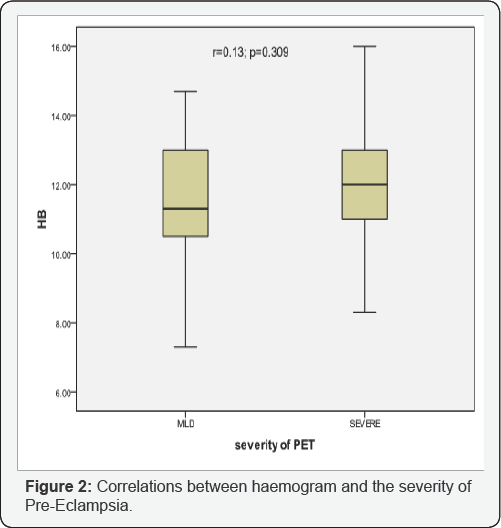
All the subjects (100%) with reduced haemoglobin concentration had low birth weight, 58% of those with increased haemoglobin concentration had low birth weight, while only 40% of the category with normal haemoglobin concentration had low birth weight and this was statistically significant as shown in (Table 7). Haemoglobin concentration, however, did not correlate in a statistical manner with the severity of pre-eclampsia as shown in (Figure 2); r= 0.13, p=0.309.
Discussion
Pre-eclampsia is a potentially dangerous complication of the second half of pregnancy, labour or early period after delivery [33]. In this study, the prevalence of severe pre-eclampsia was 35% and this was similar to 30% reported by Sandhlya et al. [34] and 32% reported by Wael et al. [35]. The frequency of vaginal delivery amongst pre-eclamptics was 33.33% while caesarean section was 66.7% and this was similar to the prevalence of caesarean section of 58% reported by Vinodhini et al. [36]and lower than 71.2% caesarean section rate among pre-eclamptic patients reported by Koffreh et al. [33] in Calabar, South- Southern Nigeria. Sandhya et al [34] however, reported the prevalence of caesarean section as 32% which was much lower than the findings in this study
The high caesarean section rate in this study may have been due to the lower mean gestational age at delivery of 35weeks as compared to the mean gestational age of 37 weeks reported by Sandhlya et al. [34].
Our results suggest that lower hemoglobin concentration is associated with a higher risk of some poor pregnancy outcomes in women with pre-eclampsia. In this study, the prevalence rate of anaemia was 6.3%. This was far lower than the 48.3% reported by Ekine et al. [37] in Bayelsa South-Southern Nigeria. This disparity in values may be due to the population demographics as their study was a rural based study with the attendant ignorance, socio-economic deprivations and lack of adequate ante-natal care. In this study, the mean haemoglobin concentration amongst the study subjects was 11.70±1.72g/dl and this was similar to the findings of Cordina et al. [38] who reported a mean haemoglobin concentration amongst pre- eclamptics as 11.34±1.00g/dl. Sandhlya et al. [34] however, found a lower haemoglobin concentration of 10.24g/dl in a similar study but Malihe et al. [39] reported a higher mean haemoglobin concentration of 12.70±1.19g/dl.
The mean haemoglobin concentration of 11.70±1.72g/ dl amongst pre-eclamptics in this study which is also similar to values reported by other researchers in similar studies may be due to contraction of intra-vascular space and subsequent haemos-concentration as is seen in pre-eclampsia as well as due to routine administration of antenatal haematinics which is the practice in this environment. We discovered that subjects with primary postpartum haemorrhage had significantly lower intrapartum haemoglobin concentration than those who did not have primary postpartum haemorrhage. The mean haemoglobin concentration for the subjects who had primary postpartum haemorrhage was 10.57±2.31g/dl and 11.93±1.50g/dl for those who did not have primary postpartum haemorrhage p-value=0.02.
Altenstadt et al. [40] in a study to investigate the association between haemoglobin concentration and postpartum haemorrhage also reported an inverse correlation between low haemoglobin concentration and postpartum haemorrhage amongst pre-eclamptics. Similarly, Kaima reported a link between low intrapartum haemoglobin concentration and the potential risk of postpartum haemorrhage and a significant inverse correlation between intrapartum haemoglobin concentration and blood loss at delivery [41]. Low intra-partum haemoglobin concentration leading to primary post-partum haemorrhage may be due to maternal anaemia resulting in impaired oxygenation of the uterus. This causes tissue enzyme and cellular dysfunction, culminating in impaired myometrial contractility and uterine atony [42].
These findings may also explain why in this study, haemoglobin concentration correlated inversely with estimated blood loss at delivery, as well as duration of hospital stay after delivery as was also reported by Kaima et al. [41] The mean duration of hospital stay in this study was 13.44±5.88 days and was higher than the findings of Curiel Basera et al who reported mean duration of hospital as 5 days [43]. This may be due to the higher prevalence of complications amongst pre-eclamptics in this study which is 92.06% as compared to the prevalence of 14% reported by Curiel et al. [43] Reduced oxygen delivery from low intra-partum haemoglobin can also result in impaired wound healing translating to increased duration of hospital stay [42].
We also found that there was a statistically significant difference between the mean haemoglobin concentration for the pre-eclamptics who had worsening proteinuria and those who did not have (12.33±1.08g/dl versus 11.38±1.62g/dl; p=0.04). This may be due to the presence of plasma volume restriction seen in pre-eclamptics, leading to increased haemoglobin concentration which causes reduced plasma viscosity and may further impair renal function by worsening glomerular damage thereby increasing proteinuria in these patients [38-45]. In this study, all the subjects (100%) with reduced haemoglobin concentration had low birth weight, 58% of those with increased haemoglobin concentration had low birth weight, while only 40% of the category with normal haemoglobin concentration had low birth weight and this was statistically significant. Indeed, several studies including the study by Murphy et al have shown a U-shaped association between maternal haemoglobin concentrations and birth weight, with reduced and increased maternal haemoglobin concentration leading to foetal growth restriction [46].
Abnormally high haemoglobin concentration usually indicates poor plasma volume expansion, which is a feature in pre-eclampsia, and a risk factor for low birth weight [47]. In like manner, low birth weights in anaemic women have been reported by Ezechi & Kalejaiye [48]. This may not be unrelated to the fact that maternal anaemia leads to impaired oxygen transport to the uterus, placenta and foetus leading to preterm birth and low birth weight [42]. In this study however, haemoglobin concentration did not influence other foeto-maternal complications like worsening hypertension, acute kidney injury, pulmonary oedema, maternal mortality, abruptio placenta, foetal distress, intra-uterine foetal death, birth asphyxia, prematurity and admission into neonatal intensive care unit (Special Care Baby Unit). This was similar to the findings of Sandhlya et al [34] and Jaleel & Khan [42] who reported that haemoglobin concentration did not influence these foeto-maternal outcomes.
Conclusion
This study revealed the inverse relationship between haemoglobin concentration and post-partum haemorrhage amongst pre-eclamptics. Post-partum haemorrhage is a major cause of maternal mortality and morbidity in resource-poor countries like ours. Haemoglobin concentration estimations may therefore serve as a cheap and readily available tool to predict post-partum haemorrhage especially in women with preeclampsia. Maternal haemoglobin concentration was also able to prognosticate the fetal birth weight in U-shaped association, indicating that both anaemia and elevated haemoglobin levels may lead to fetal growth restriction and low birth weight which further worsens the prognosis of pre-eclampsia.
In this study also, there was an inverse correlation between haemoglobin concentrations with postpartum haemorrhage, hence postpartum haemorrhage should be anticipated when pre-eclamptics have low haemoglobin concentration values so as to optimize these patients and take steps to prevent blood loss at delivery. Future research may however, be useful in determining the cut-off haemoglobin concentration that may predict postpartum haemorrhage in pre-eclamptics as this may help obstetricians better anticipate and prevent morbidities and mortalities associated with postpartum haemorrhage in this condition.
Limitations of this Study
A single haemoglobin concentration estimation may not be adequate in the assessment of these patients with respect to management, as some pre-eclamptics may need further monitoring of deranged parameters for possible worsening condition. However, assessment of the haemoglobin concentration at delivery may help to mitigate this limitation. Our study comprised of patients with pre-eclampsia, irrespective of the gestational ages and severity of disease. This may possibly affect their haemoglobin concentration, hence in this study however this confounder was absent since all the subjects were within the third trimester of pregnancy (28 -41 weeks of gestation).
References
- Alexandre H, Philippe L (2010) New markers in preeclampsia. Clin Chim Acta 411(21-22): 1591-1595.
- Ghulimiyyah L, Sibai B (2012) Maternal mortality from pre-eclampsia/ eclampsia. Semin Perinatol 36(1): 56-59.
- Moodley J (2004) Maternal deaths associated with hypertensive disorders of pregnancy: a population-based study. Hypertens Pregnancy 23(3): 247-256.
- Onah HE, Okaro JM, Umeh U, Chigbu CO (2005) Maternal mortality in health institutions with emergency obstetric care facilities in Enugu State, Nigeria. J Obstet Gynaecol 25(6): 569-574.
- Hogberg U (2005) The World Health Report 2005: make every mother and child count including Africans. Scand J Public Health 33(6): 409411.
- Khan KS, Wojdyla D, Say L, Gülmezoglu AM, Van Look PF (2006) WHO analysis of causes of maternal death: a systematic review. Lancet 367(9516): 1066-1074.
- Steegers EA, Dadelszen VP, Duvekot JJ, Pijnenborg R (2010) Preeclampsia. Lancet 376(9741): 631-644.
- Salako BL, Odukogbe AA, Olayemi O, Adedapo KS, Aimakhu CO (2002) Burden and Pattern of Hypertension in Pregnant Mothers attending Antenatal Care at the University College Hospital Ibadan. Paper presented at the 6th International Congress of the Society of Gynaecology and Obstetrics of Nigeria (SOGON), held in Abuja, Nigeria.
- Onuh SO, Aisien AO (2004) Maternal and Fetal Outcome in eclamptic patients in Benin City, Nigeria. J Obstet Gynaecol 24(7): 765-768.
- National Study on Essential Obstetric Care Facilities in Nigeria, Federal Ministry of Health, Abuja, Nigeria. 2003. p. 37.
- Omole OA, Ashimi AO (2008) Preeclampsia: a study of risk factors, Nigerian. Medical Practitioner 53(6): 99-102.
- Dulley L (1992) Maternal mortality associated with hypertensive disorders of pregnancy in Africa, Asia, Latin America and the Caribbean. Br J Obstet Gynaecol 99(7): 547-553.
- Nwagha UI, Nwachukwu D, Dim C, Ibekwe PC, Onyebuchi A (2010) Maternal mortality trend in South East Nigeria: less than a decade to the millennium developmental goals. J Womens Health (Larchmt) 19(2): 323-327.
- Olapade FE, Lawon TO (2009) Maternal mortality in a Nigerian maternity hospital. Afr J Biomed Res 11: 267-273.
- Population Council Nigeria (2009) Administering magnesium sulphate to treat severe pre-eclampsia and eclampsia.
- Department of Obstetrics and Gynaecology Annual Report (2013) University of Port Harcourt Teaching Hospital. Port Harcourt, Nigeria.
- George IO, Jeremiah I (2009) Perinatal Outcome of Babies Delivered to Eclamptic Mothers: A Prospective Study from a Nigerian Tertiary Hospital. Int J Biomed Sci 5(4): 390-394.
- Uzoigwe SA, John CT (2004) Maternal Mortality in the University of Port Harcourt Teaching Hospital, Port Harcourt in the Last Year Before the New Millennium. Niger J Med 13(1): 32-35.
- Hytten F, Paintin D (1963) Increase in plasma volume during normal pregnancy. J Obstet Gynaecol Br Emp 70: 402-427.
- Taylor DJ, Lind T (1979) Red cell mass during and after normal pregnancy. Br J Obstet Gynaecol 86(4): 364-370.
- Buchan PC, Donald MHN (1981) Rheological factors in Obstetrics and Gynaecology. In: Lowe GDO, Barbenel JC, Forbes CD, eds. Clinical aspects of blood viscosity and cell deformity. Berlin, Heidelberg, New York, USA, pp. 465-478.
- Steer PJ (2000) Maternal hemoglobin concentration and birth weight. Am J Clin Nutr 71(5 suppl): 1285S-1287S.
- Garn SM, Ridella SA, Petzold AS, Falkner F (1981) Maternal hematologic levels and pregnancy outcomes. Semin Perinatol 5(2): 155-162.
- Murphy JF, ORiordan J, Newcombe RG, Coles EC, Pearson JF (1986) Relation of haemoglobin levels in first and second trimesters to outcome of pregnancy. Lancet 1(8488): 992-995.
- Hobbs JB, Oats JN, Palmer AA, Long PA, Mitchell GM, et al. (1982) Whole blood viscosity in preeclampsia. Am J Obstet Gynecol 142(3): 288-292.
- Sagen N, Koller O, Haram K (1982) Haemoconcentration in severe preeclampsia. Br J Obstet Gynaecol 89(10): 802-805.
- Kuzniar J, Piela A, Skert A, Szmigiel Z, Zaczek T(1982) Echocardiographic estimation of hemodynamics in hypertensive pregnancy. Am J Obstet Gynecol 144(4): 430-437.
- Ceyhan T, Beyan C, Baser I, Kaptan K, Gingor S et al. (2006) The effect of pre-eclampsia on complete blood count, platelet count and mean platelet volume. Ann Hematol 85(5): 320-322.
- Kish L (1965) Survey Sampling, John Wiley and Sons, New York, USA, p. 643.
- Department of Obstetrics and Gynaecology Annual Report (2013) University of Port Harcourt Teaching Hospital, Port Harcourt, Nigeria.
- National High Blood Pressure Education Program Working Group on High Blood Pressure in Pregnancy. (1990) Am J Obstet Gynecol 163(5): 1691-1712.
- Naz H, Sanwar I, Fawad A, Nisa AU (2008) Maternal morbidity and mortality due to primary PPH: experience at Ayub Teaching Hospital Abbottabad. J Ayub Med College Abbottabad 20(2): 59-65.
- Kooffreh M E, Ekott M, Ekpoudom DO (2014) The prevalence of pre-eclampsia among pregnant women in the University of Calabar Teaching Hospital, Calabar. Saudi J for Health Sciences 3(3): 133-136.
- Sandhya S, Bhat BV, Ashok BB (2007) Effect of Pregnancy Induced Hypertension on Mothers and their Babies. Indian J Pediatr 74(7): 623-625.
- Wael AEKA, Moharam AHH, Mahmoud AG, Mohamed IM (2014) Evaluation of platelet indices and their significance in Preeclampsia. Nat Sci 12 (3): 147-153.
- Vinodhini R, Kumari L (2014) Evaluation of platelet count as a prognostic index in eclampsia and pre eclampsia. Int J Modn Res Revs 2(10): 447-452.
- Ekinne AA, Jeremiah I, Harry TC, West OL (2015) Factors influencing the prevalence of preeclampsia-Eclampsia in booked and unbooked patients: 3 years retrospective study in NDUTH, Okolobiri. World Journal of Medicine and Medical sciences 3(1): 1-14.
- Cordina M, Bhatti S, Fernandez M, Syngelaki A, Nicolaides KH, et al. (2015) Maternal hemoglobin at 27-29 weeks' gestation and severity of pre-eclampsia. J Matern Fetal Neonatal Med 28(13):1575-1580.
- Malihe N, Soghrat F, Hamid AM, Farid Z, Noorosadat K, et al. (2015) Longitudinal discriminant analysis of haemoglobin level for predicting pre-eclampsia. Iran Red Crescent Med J 17(3):e19489.
- Altenstadt JV, Hukkelhoven CWPM, Roosmalen JV, Bloemenkamp KWM (2013) Pre-eclampsia Increases the Risk of Postpartum Haemorrhage: A Nationwide Cohort Study in The Netherlands. PLoS One 8(12): e81959.
- Kaima AF (2015) Postpartum hemorrhage is related to the hemoglobin levels at labor: Observational study. Alexandria J Med 51: 333-337.
- Jaleel R, Khan A (2008) Severe anemia and adverse pregnancy outcome. Journal of Surgery Pakistan (International) 13(4): 147-150.
- Curiel BE, Prieto PMA, Munoz BJ, Ruiz de Elvira MJ, et al. (2011) Analysis of maternal morbidity and mortality among patients admitted to Obstetric Intensive Care with severe pre-eclampsia, eclampsia or HELLP syndrome. Med Intensiva 35(8): 478-483.
- Magnus GO, Magnus C, Sigurbjorg R, Stenfors I, Jorgen G, et al. (2009) Increased levels of cell-free hemoglobin, oxidation markers, and the antioxidative heme scavenger alpha (1)-microglobulin in preeclampsia. Free Radic Biol Med 48(2): 284-291.
- Chandiramani M, Waugh J, Shennan A (2007) Preeclampsia in pregnancy, Management of hypertension. Trends in Urology Gynaecology & Sexual Health 12: 23-28.
- Murphy JF, ORiordan J, Newcombe RJ, Coles EC, Pearson JF (1986) Relation of hemoglobin levels in first and second trimesters to outcome of pregnancy. Lancet 1(8488): 992-995.
- Steer PJ (2000) Maternal hemoglobin concentration and birth weight. Am J Clin Nutr 71(5 suppl): 1285S-1287S.
- Singla PN, Tyagi M, Kumar A, Dash D, Shankar R (1997) Fetal growth in maternal anemia. J Trop Pediatr 43(2): 89-92.






























