Evaluation of Ultrasound Scoring Model for Pre-Natal Diagnosis of Placenta Accrete in A Tertiary Referral Center
Elsayed Elbadawy M Awad1, Amal Z Azzam1, Nahed M Badour2, Tamer M Abdel Dayem1* and Soha A Khalil1
1Department of Obstetrics and Gynecology, university of Alexandria, Egypt
2Pathology Department, university of Alexandria, Egypt
Submission: August 05, 2017; Published: August 28, 2017
*Corresponding author: Tamer M Abdel Dayem, Department of Obstetrics and Gynecology, university of Alexandria, 18 pharanaa Street Azarita, Alexandria, Egypt, Tel: 00201226720766; Email: tmdaeim@gmail.com
How to cite this article: Elsayed Elbadawy M, Amal Z A, Nahed M B, Tamer M Abdel D, Soha A K. Evaluation of Ultrasound Scoring Model for Pre-Natal Diagnosis of Placenta Accrete in A Tertiary Referral Center. J Gynecol Women's Health 2017; 6(4): 555692. DOI: 10.19080/JGWH.2017.06.555692.
Abstract
Background: Morbidly adherent placenta (MAP) is one of life threatening complication of pregnancy. The precise etiology is unknown; however an abnormally adherent placenta is associated with factors which predispose to abnormal myometrial invasion by placental villi. It is associated with considerable morbidity including postpartum haemorrhage and obstetric hysterectomy. The most important factor affecting the outcome is the prenatal diagnosis of this condition. It gives the opportunity to make a delivery plan that properly anticipates the expected blood loss and other potential complications of delivery. In addition, it gives the opportunity for electively timing the procedure since prevention of complications ideally requires the presence of a multidisciplinary surgical team.
Aim of the work: The aim of this study was to evaluate the efficacy of ultra sonographic scoring system in diagnosis of MAP.
Patients and methods: During the study period, 105 pregnant women with prior cesarean delivery with either placenta previa or low- lying placenta underwent 2-D and Doppler ultrasonic examination in the third trimester. Confirmation was based on histologic evidence of placental invasion. In the final analysis, 45 pregnant women (42.8%) had histologic confirmation of MAP; the remaining 60 (57.2%) served as control group.
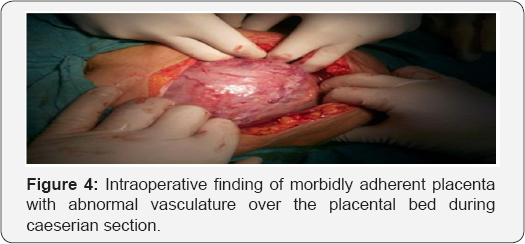
Results: Use of ultrasound scoring model in detection of pregnancy complicated by placenta accreta is highly predictive. It includes: Placental lacunar spaces, myometrial thickness, bridging vessels, uterovesical hyper vascularity were the most significant parameters in diagnosis of morbidly adherent placenta. The optimal management after delivery of the neonate is vague. Hysterectomy immediately after delivery of the neonate without attempts at placental removal had been recommended to lower mortality and morbidity.
Introduction
Placenta accreta, increta and percreta are all forms of morbidly adherent placenta (MAP) with abnormally invasive placentation. It is a life threatening complication of pregnancy [1]. It is defined by trophoblastic invasion of the myometrium in the absence of intervening decidua. Superficial myometrial invasion is classed as accreta, deeper myometrial invasion as increta, and invasion through the serosa or into adjacent pelvic organs as percreta [2]. The condition was of such rarity 60 years ago that many experienced practicing obstetricians had never encountered a case, and the associated maternal morbidity rate was extremely high (37-67% of cases managed) [3]. It remains the current most common cause of obstetric hysterectomy, with mortality rate 7% even in best hands [4]. Despite the fact that, awareness of the condition and its attendant risks is increasing, no consensus exists regarding the best management strategies to maximize outcomes [5]. Women with placenta accreta or any of its variants are at high risk of life -threatening massive obstetric hemorrhage, bladder injury, uterine perforation and rupture, peripartum hysterectomy and maternal death [6]. The commonest etiologic factors seen with MAP are previous myometrial injury in conjunction with a low lying placenta [7]. Women with placenta previa and a previous cesarean delivery are now well established as being at greatest risk for MAP [8].
Currently, it could be suspected in the late first trimester, but most cases are detected in the second trimester, although the diagnosis may remain inconclusive until the later stages of pregnancy when there are no symptoms of vaginal bleeding to prompt earlier investigation [9]. Ultrasound imaging has a good negative predictive value for the diagnosis of MAP ranging between 92% and 98%, a fact which is invaluable in any good screening program [10]. Proper management should be based on accurate early diagnosis with appropriate perioperative multidisciplinary planning to anticipate and avoid massive obstetric hemorrhage at delivery [11]. The antenatal diagnosis of MAP depends on 2D grey scale imaging and 2D color Doppler Imaging [12]. The 2D Sonographic parameters include, location of placenta ,loss of retroplacental clear zone, irregularity and thickness of the uterine bladder interface, the smallest myometrial thickness in the sagittal plane, presence of lacunar spaces, placental bulge and focal exophytic mass [13]. The 2D Color Doppler Parameters include, utero-vesical hypervascularity, subplacental hypervascularity, bridging vessels and placental lacunae feeder vessels [14]. Aim of the work was to asses the efficacy of the use of the ultrasound scoring model in detection of pregnancy complicated by placenta accreta.
Patients
It is a prospective descreptive study of 45 cases of morbidly adherent placenta managed by cesarean hysterectomy at El- Shatby Maternity University hospital
Inclusion criteria include
A. Sonographic confirmation of placenta previa or low lying anterior placenta in the third trimester.
B. Age (20-45years).
C. Presence of uterine scar e.g. previous caesarean section, previous myomectomy or history of uterine perforation.
D. MAP managed by cesarean hysterectomy
Exclusion criteria include
No exclusion criteria.
Methods
Every patient will be subjected to
1. History taking, which include
1. Age.
ii. Number of prior cesarean deliveries.
iii. Previous uterine surgeries.
2. Ultrasound and color Doppler examination:
i. Routine ultrasound examination: fetal biometry amniotic fluid and placental location.The study will be carried out on pregnant females during the third trimester with placenta).
ii. Score system for diagnosis of MAP, which include:
Location of placenta: placenta previa (placental tissue covering the internal cervical os) or anterior low lying placenta (the placenta within 2 cm from the internal cervical os but did not cover it or antrior low lying placenta.
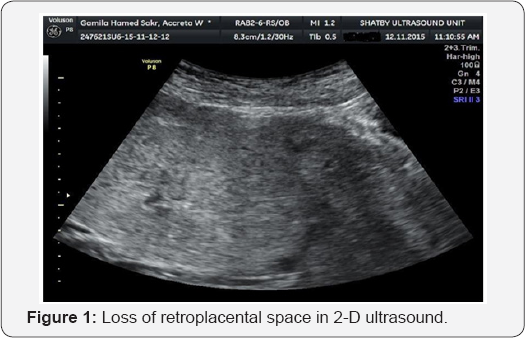
Loss of retroplacental clear space: the echolucent line that sonographically represent vascular decidua basalis and extends through the entire length of placenta is obliterated.
Irregularity of uterine bladder interface: caused by abnormal bridging vasculature that is easily seen with Doppler.
Thinning of uterine bladder interface: normally thick and echogenic interface is replaced by ingrowth of morbidly adherent placenta.
Myometrial thickness: retroplacental myometrium is thin as result of abnormal ingrowth of placenta. The smallest myometrial thickness in sagittal plane <1mm.
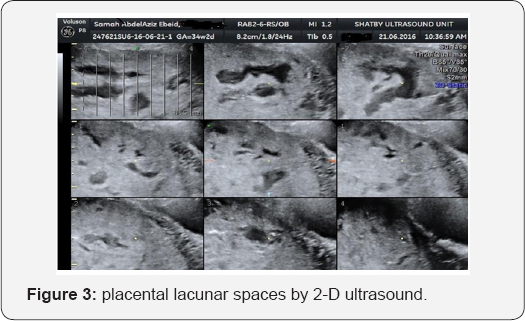
Placenta lacunar spaces: sonolucent areas througthout placenta that vary in size and shape and give placenta "Swiss cheese "appearance. Lacunar spaces are graded according to Finberg and Williams as follows:
i. Grade 0: No lacunar spaces are seen.
ii. Grade 1:1-3 lacunar spaces present and generally small.
iii. Grade 2: 4-6 lacunar spaces present and tending to be larger and more irregular.
iv. Grade 3: many lacunar spaces throughout the placenta and appearing large and bizarre.
Placental bulge: Deviation of the uterine serosa away from the expected plane, caused by an abnormal bulge of placental tissue into a neighboring organ, typically the bladder. The uterine serosa appears intact but the outline shape is distorted.
Focal exophytic mass: Placental tissue seen breaking through the uterine serosa and extending beyond it. Most often seen inside a full urinary bladder.
Bridging vessels: Doppler colored mapping demonestrates abnormal vasculature that bridge from placental mass to uterine bladder interface and some times beyond.
Utero-vesical hypervascularity: stricking amount of colour signal seen between the myometrium and the posterior wall of the bladder.
Sub-placental hypervascularity: stricking amount of colour signal seen in the placental bed.
Placental lacunae feeder vessels: vessels with high velocity blood flow leading from myometrium into the placental lacunae, causing turbulence upon entry
Confirmation of morbidly adherent placenta will based on histologic evidence of placental invasion from hysterectomy specimen. Sonographic parameters will be evaluated by histopathology as much as possible.
Results
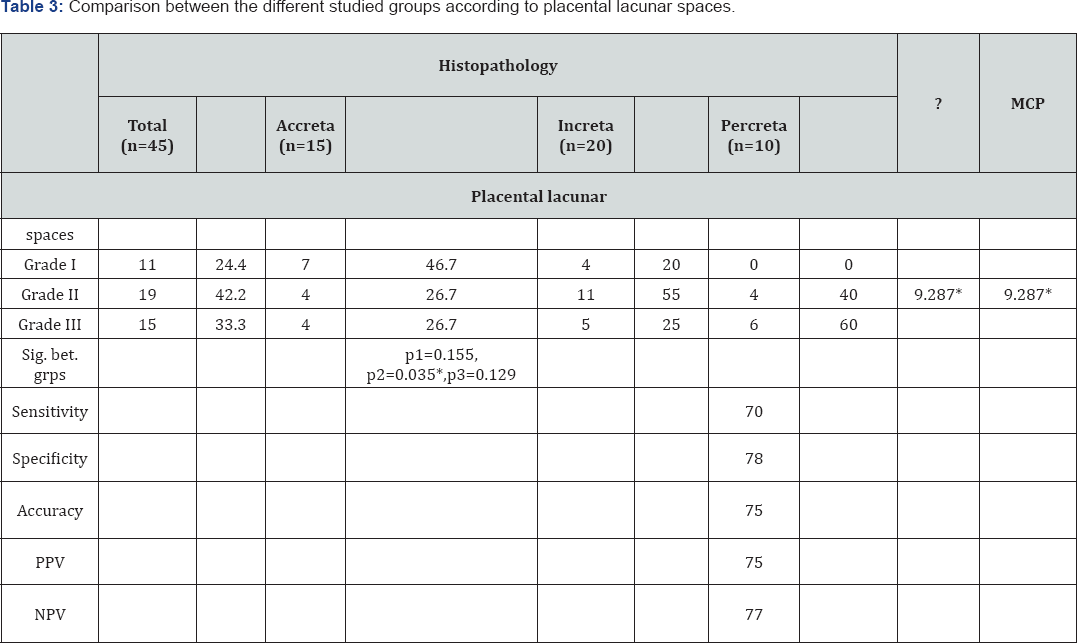
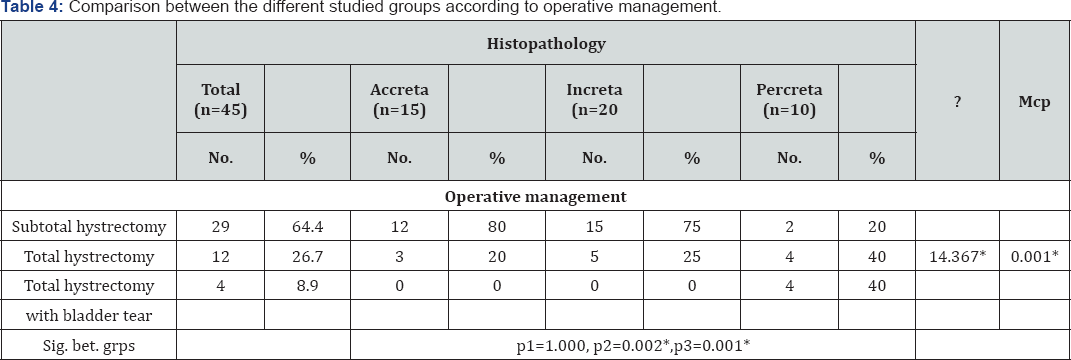
During the study period between October 2015-March 2017, 105 pregnant women presented to the antenatal care clinic of El Shat by Maternity Hospital with suspicion of morbidly adherent placenta on ultrasound examination. In 45 pregnant women (42.8%) the placenta could not be separated from the uterus during delivery and cesarean hysterectomy was performed. The histopathologic reports confirmed the diagnosis in all cases. The other 60 pregnant women (57.2%) had complete separation of placenta and served as control group. According to antenatal ultrasonography, 23 cases (51.1%) were placenta previa complete centralis. 22 cases (48.9%) was placenta previa incomplete centralis. Antenatal ultrasonography showed that loss of retroplacental spaces seen in 71.1% of cases, 8 cases (53.3%) diagnosed by histopathology as placenta accreta while 14 cases (70%) placenta increta and 10 cases (100%) placenta percreta. Preserved retro placental spaces seen in 13 according to cases (28.9%), 7 cases (46.7%) diagnosed by histopathology as placenta accreta while 6 cases (30%) placenta increta and no cases (0%) was placenta percreta Table 1-4, Figure 1-4. Placental lacunar spaces seen by ultrasonography divided into 3 grades according to the number of lacunae inside the placenta. 24.4% was grade 1lacunar spaces, 42.2% was grade 2 while 33.3% was grade 3, with sensitivity 70%, specificity 78%, accuracy 75%, PPV 75% and NPV 77%.
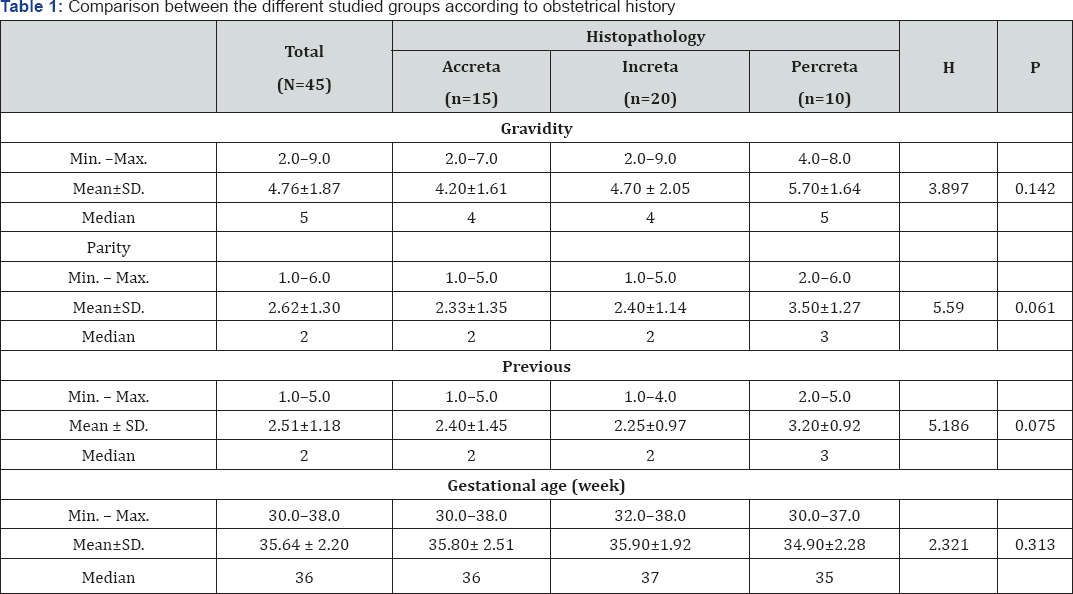
H, p: H and p values for Kruskal Wallis test.
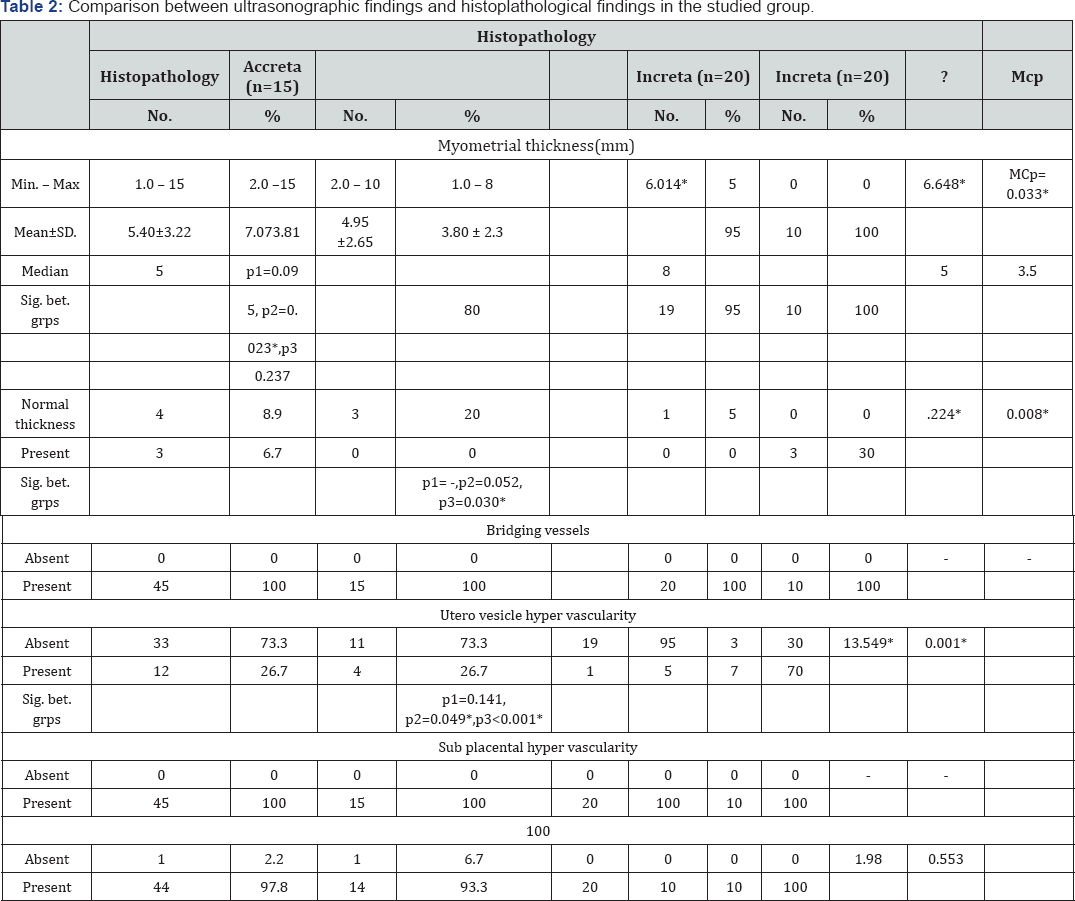
The lost retro placental space was statistically significant (p=0.033), with sensitivity 65%, specifity 74%, 70% accuracy, positive predictive value 67% and negative predictive value 72% . Of the included 45 cases, the myo metrial thickness measured by 2-D ultrasound ranged between 1mm and 15mm with a mean of 5.40±3.22.
Myo mertrial thickness was <5mm in 14 cases (31.1%), 5-10mm in 23 cases (51.1%) and >10mm in 8 cases (17.8%) of cases.
The myo metrial thickness was statistically significant (p=0.049). With sensitivity 86.7%, specificity 73.3% and 75.5% accuracy.
?, p:?2 and p values for Chi square test
MC: Monte Carlo for Chi square test
p1: p value for comparing between accrete and increta
p2: p value for comparing between accrete and percreta
p3: p value for comparing between increta and percreta
*: Statistically significant at p≤0.05.

Discussion
Placenta accrete remains the leading cause of obstetric hysterectomy worldwide, with 7% mortality in best conditions available. Prenatal ultrasonographic diagnosis helps in reducing morbidity and mortality resulting from this condition. Our study aimed at evaluating ultrasonographic scoring system for diagnosis of placenta accreta. Our study included 105 women suspected by ultrasonogram to have placenta accrete. In 45 cases, the placenta couldnot be separated and hysterectomy with done. Histopathological examination confirmed the presence of placenta accreta in these cases
Silver et al. [3] found that in the setting of placenta previa, the risk of accreta was 11%, 40%, and >60% in women with 1, 2, and 3 prior cesarean deliveries. The number of prior cesarean deliveries was highly predictive of placental invasion among pregnancies at increased risk. It may be used for counseling and preoperative planning, by either heightening awareness for morbidly adherent placenta or providing reassurance to a woman who desires future fertility. Our scoring model includes the following parameters: loss of retroplacental space, irregularity and thickness of the uterine bladder interface, myometrial thickness, lacunar spaces, bridging vessels, subplacental and uteovesical hypervascularity and placental lacunar feeder vessels. We have evaluated the value of various ultrasound parameters used in diagnosis. In our study, we found that the hypoechoic retroplacental space lost in 71.1% of cases with sensitivity 65%, specificity 74%, accuracy of 70%, PPV 67% and NPP 72%.
Cali et al. [15] reported recently that the absence of the uteroplacental demarcation was the most effective sonographic criterion for detection of an invasive placenta, with a negative predictive value of 96.7%. In these study irregularity and thinning of uterine bladder interface were with sensitivity 45%, 68% & specificity 38%, 52% & accuracy 42%,55% & PPV 80%, 65% and NPP 53%, 50% . For placental lacunar spaces 24.4% of cases were of grade 1 lacunar spaces, 42.2% of grade 2 and 33.3% of grade 3 lacunar spaces with sensitivity 70%, specificity 78%, accuracy 75%, PPV 75% and NPP 77%. Comstock et al. [12] conducted a prospective study on patients with previous cesarean delivery and anterior placenta or placenta previa. They found that visualization of irregular vascular spaces within the placenta is associated with increased incidence of placenta accreta. On the other hand they found that obliteration of the retroplacental space not a reliable diagnostic sign for placenta accreta.
Finberg and Williams [13] found that number and bizarre appearance of lacunar spaces was directly correlated with certainty and severity of morbidly adherent placenta. In a recent systematic review, overall pooled sensitivity and specificity of lacunar spaces from 13 studies was 77% and 95% with an overall diagnostic accuracy of 0.884 [13]. When multiple, especially 4 or more lacunae, these findings have been correlated with a detection rate of 100% for placenta accreta. This marker also has low false-positive rates, but it should be noted that placenta accreta has been reported with absent multiple vascular lacunae. The myometrial thickness in our study has high predictive value. It was ranging between 1mm and 15mm with mean of 7.07±3.81for placenta accreta, 4.95±2.65 for placenta increta and 3.80±2.30 for placenta percreta. The sensitivity was 86.7%, specificity 73.3%, accuracy 75%, PPV 75% and NPV 80%. The cutoff point was 3.5, the myometrial thickness <3.5 indicate accreta.
Twickler et al. [16] found that a smallest myometrial thickness <1 mm identified in third-trimester pregnancies at risk for placental invasion was 100% sensitive and 72% specific with a PPVand NPVof 72% and 100%, respectively. Hypervascularity of the uterine-bladder interface and bridging vessels using both 2- and 3-dimensional Doppler ultrasound were found almost in all of our cases. D'Antonio et al. [11] reported that the presence of bridging vessels identified with color Doppler imaging was the most predictive ultrasound parameter of morbidly adherent placenta, with an overall diagnostic accuracy of 0.95. Placental bulge and focal exophytic mass not seen in any case in our study although there was 4 cases underwent bladder repair after its injury during the cesarean hysterectomy [11]. We found that a score derived from the ultrasound parameters of smallest myometrial thickness, lacunar spaces, and presence of vascularity, in addition to the number of prior cesarean deliveries and placental location, was highly predictive of placental invasion among pregnancies at increased risk.
Instead of using each ultrasound variable individually, our model establishes a scoring system for ultrasound evaluation of all patients at risk for morbidly adherent placenta. The application of the score system can be helpful in stratifying individual risk of invasion above the a prior risk based on number of prior cesarean deliveries and placental location. Assigning a score in clinical practice may be helpful in the antenatal diagnosis of MAP and seems to be a key factor in reducing maternal and fetal morbidity and mortality, by allowing multidisciplinary counseling, and planning and timing of delivery. Tovbin et al. [17] reported a series of 258 women, twenty-three (8.9%) women had a diagnosis of MAP and 2 35 (91.1%) had no clinical evidence of an adherent placenta. The mean SD maternal age was 33.8±4.5 years, mean gestational age at diagnsosis was 33.9 range (1641) weeks, mean SD maternal gravidity and parity were 4.0±1.6 and 2.0±1.2, respectively and mean gestational age at delivery was 37.7±1.7 range (24-41)weeks.
Each individual sonographic parameter that were assessed in the scoring system was significantly associated with MAP (P<0.0001). The overall sensitivity, specificity, and positive and negative predictive values of a high probability score diagnosing MAP were 69.6% , 98.7% , 84.2% and 97.1% , respectively The positive and negative likelihood ratios were 54.5 and 0.31, respectively. The overall sensitivity (detection rate) was 91.3% and the specificity was 93.6%. Number and size of placental lacunae, obliteration of demarcation between uterus and placenta was the most effective sonographic criteria for detection of an invasive placenta. Gilboa et al. [18] reported a series of 21 women with placenta percreta that was identified at surgery and proposed a scoring system based on the sonographic findings. Their detection rate of placenta percreta was 63.6%. However, the main goal of their scoring system was to identify patients with Stage 3 MAP and offer a prophylactic pelvic artery catheterization. Color Doppler imaging included: increased subplacental vascularity, presence of lacunar flow, vessels bridging from placenta to uterine margin, bladder uterine serosa interface hypervascularity, vessels extending from placenta to bladder and vessels crossing placental tissue interface disruption.
Overall, grayscale sonography is an excellent tool for the prenatal diagnosis of placenta accreta in women at risk for this abnormality. It's sensitivity has been reported in some reports in the range of 77% to 87% with specificity of 96% to 98%, a positive predictive value (PPV) of 65% to 93%, and a negative predictive value (NPV) of 98%.
Conclusion
Our study concludes that the use of scoring system for prenatal diagnosis is effective in identifying the condition. This helps in proper planning of management and reduction of the associated morbidity and mortality.
Conflict of Interest
Authors declare there is no conflict of interest regarding publication of this article.
References
- Khong TY (2008) The pathology of placenta accreta, a worldwide epidemic. J Clin Pathol 61(12): 1243-6.
- Oyelese Y, Smulian JC (2006) Placenta previa, placenta accreta, and vasa previa. Obstet Gynecol 107(4): 927-41.
- Silver RM, Landon MB, Rouse DJ (2006) Maternal morbidity associated with multiple repeat cesarean deliveries. Obstet Gynecol 107(6): 12261232.
- Stirnemann J, Forner S, Bernard J, Ville Y (2010) Screening for placenta accreta by ultrasound in the first trimester. Ultrasound Obstet Gynecol 36:139-140.
- Esakoff TF, Sparks TN, Kaimal AJ (2011) Diagnosis and morbidity of placenta accreta. Ultrasound Obstet Gynecol 37(3): 324-327.
- Shih JC, Palacios JJM, Su YN (2009) Role of three dimensional power Doppler in the antenatal diagnosis of placenta accreta: comparison with gray-scale and color Doppler techniques. Ultrasound Obstet Gynecol 33: 193-203.
- Comstock CH (2005) Antenatal diagnosis of placenta accreta: a review Ultrasound Obstet Gynecol 26(1): 89-96.
- (2011) Royal College of Obstetricians and Gynaecologists. Placenta praevia, placenta praevia accreta and vasa praevia: diagnosis and management. Clinical guideline. London: RCOG Press 27.
- Snelgrove JW (2009) Postpartum haemorrhage in the developing world; a review of clinical management strategies. McGill J Med 12(2): 61-66.
- Comstock CH (2010) The antenatal diagnosis of placental attachment disorders. Curr Opin Obstet Gynecol 23(2):117-122.
- DAntonio F, Iacovella C, Bhide A (2013) Prenatal identification of invasive placentation using ultrasound: systematic review and metaanalysis. Ultrasound Obstet Gyneco 42(5): 509-517.
- Comstock CH, Bronsteen RA (2014) The antenatal diagnosis of placenta accreta. BJOG 121(2): 171-81.
- Finberg HJ, Williams JW (1992) Placenta accreta: prospective sonographic diagnosis in patients with placenta previa and prior cesarean section. J Ultrasound Med 11(7): 333-43.
- Collins SL, Stevenson GN, Noble JA, Impey L, Welsh AW (2012) Influence of power Doppler gain setting on Virtual Organ Computer- aided AnaLysis indices in vivo: can use of the individual sub-noise gain level optimize information? Ultrasound Obstet Gynecol 40(1): 75-80.
- Cali G, Giambanco I, Puccio G, Foriani F (2013) Morbidly adherent placenta: evaluation of ultrasound diagnostic criteria and differentiation of placenta accreta from percreta. Ultrasound Obstet Gynecol 41(4): 406-412.
- Twickler DM, Lucas MJ, Balis AB, Santos RR, Martin L, et al. (2000) Color flow mapping for myometrial invasion in women with a prior cesarean delivery. J Matern Fetal Med 9(6): 330-335.
- Tovbin J, Melcer Y, Shor S (2016) Prediction of morbidly adherent placenta using a scoring system. Ultrasound Obstet Gynecol 48(4): 504-510.
- Gilboa Y, SpiraM, Mazaki TS, Schiff E, Sivan E, et al. (2015) A novel sonographic scoring system for antenatal risk assessment of obstetric complications in suspected morbidly adherent placenta. J Ultrasound Med 34(4): 561-567.






























