Comparison of Efficacy of Stress Urinary Incontinence Surgeries: Tvt alone vs Tvt Plus Concomitant Surgery
Ağahan Han, Emre Sinan Güngör*, Erbil Karaman and Huseyin Kiyak
Suleymaniye Maternity Research Training & Hospital, Turkey
Submission: July 22, 2017; Published: July 31, 2017
*Corresponding author: Emre Sinan Güngör, Suleymaniye Maternity Research Training & Hospital, Kaptanpaşa Mahallesi Halit Ziya Türkkan Sokak No:10 A Blok Daire 24, şişli Istanbul, Turkey, Tel: +90 5325574055; Email: doksinangungor@hotmail.com
How to cite this article: Aoahan H, Emre S G, Erbil K, Huseyin K. Comparison of Efficacy of Stress Urinary Incontinence Surgeries: Tvt alone vs Tvt Plus Concomitant Surgery. J Gynecol Women's Health 2017; 6(3): 555688. DOI: 10.19080/JGWH.2017.06.555688.
Abstract
Objectives: Urinary incontinence is one of the most common functional pathology for women during the pre- and post-menopausal periods. Tension-free vaginal tape (TVT) is a commonly performed surgical technique for stress urinary incontinence (SUI). The aim of this study is to evaluate the efficacy and success rate of TVT operation performed alone with comparison to TVT plus concomitant procedure of vaginal hysterectomy (VH).
Methods: We reviewed patients with SUI from January 2012 to December 2014. 105 patients underwent TVT operation alone (group 1) and 94 patients underwent TVT and VH operation (Group 2). All patients filled The International Consultation on Incontinence Questionnaire- Short Form (ICIQ-SF) pre and postopeartively. Each patient underwent physical examination and urodynamic study. The primary outcome measure was the objective cure rate of SUI following TVT.Secondary outcome measure was subjective cure rate of SUI and this was evaluated by ICIQ-SF. Intra-operative and postoperative complications were also recorded.
Results: There were no significant differences between the two groups with respect to patients' demographic characteristics. Postoperative SUI was seen significantly lower in group 1 than group 2 (5.71% vs 14.89%, p<0.05). Complication rate was statistically higher for group 2 (4.76% vs 18.08% respectively, p<0.05). Post-voiding residuel urine volumes were significantly lower for group 1 than group 2 both preoperative and postoperatively.
Conclusion: Patients in both groups had benefit from TVT surgery but when the groups were compared according to subjective and objective results, it was appareant that the TVT alone group had statistically higher success rates than TVT+VH group.
Keywords: Prolapse; Stress urinary incontinance; Tension-free vaginal tape; Urinary retention; Vaginal hysterectomy
Abbreviations: TVT: Tension-Free Vaginal Tape; SUI: Stress Urinary Incontinence; VH: Vaginal Hysterectomy; ICIQ-SF: Incontinence Questionnaire-Short Form; POP-Q: Prolapsus Quantification System
Introduction
Urinary incontinence is one of the most common functional pathologyfor women during the pre- and post- menopausalperiods [1]. Urethral hypermobility is the main anatomic abnormality in the pathogenesis of incontinent women [2]. Tension-free vaginal tape (TVT) is a commonly performed surgical technique for stress urinary incontinence (SUI). It ensures a suburetral vaginal hammock and its short-term results confirms that TVT procedure is a safe and effective technique, when performed alone [3,4].
Women undergoing surgical treatment of SUI generally need accompanying surgical proceduresrelated to pelvic relaxation such as uterine prolapse, rectocele or cystocele. Performing TVT during other pelvic surgical procedures have some advantages such as lower cost, reduced risk of anesthesia realted morbidity and a shorter hospital stay [5]. Howeverthere are controversials on the safety of concomitant surgeries and the success rates of TVT performed during other pelvic surgeries.
The aim of this study is to evaluate the efficacy and success rate of TVT operation performed alone with comparison to TVT plus concomitant procedure of vaginal hysterectomy (VH).
Material and Methods
We reviewed 240 patients with stress incontinence from January 2012 to December 2014, but we could not reach 41 patients' data so 199 patients were enrolled for the study Approval for the study was given by the hospital's ethical committee. 105 patients underwent TVT operation alone (Group 1) and 94 patients underwent TVT and vaginal hysterectomy operation (Group 2). All patients filled The International Consultation on Incontinence Questionnaire-Short Form (ICIQ- SF) pre-operatively and post-opeartively according to data record policy of our urogynecology clinic. ICIQ-SF is validated for Turkish speaking population. It is a subjective measure for evaluating the severity of urinary loss. This questionnaireconsists of three components measuring:
i. Frequency,
ii. Severity, and
iii. Quality of Life.
Validity, reproducibility and responsiveness of the testhave recently been investigated by several authors [6]. TVT operations were performed as described by Ulmsten et al. [7]. A non-elastic monofilament polyprophilene tape was used in the mid-urethral sling procedure (Betamix vaginal sling, Betatech laboratories, TURKEY).
Before TVT operation, each patient underwent physical examination andurodynamic study. Physical examination was performed with the patient in the litho to my position. Patients were hydrated two hours before physical examination. Loss of urine was tested during coughing and stress. A positive cough stress test was defined as the involuntary loss of urine during cough. The stress test was performed during moderate coughing in lithotomy when the bladder volume measured 300-350ml, in 3 dimensions using ultrasound guidance. The stage of the prolapse was assessed in the lithotomy position while the patient performed a valsalva maneuver. The degree of pelvic organ prolapsus was assesed by the pelvic organ prolapsus quantification system (POP-Q) during gynecologic examination [8].
The primary outcome measure was theobjective cure rate of SUI following TVT. Patients were considered objectively cured when no SUI was evident during post operative period determined as stres test nagative. Secondary outcome measure was subjective cure rate of SUI and this was evaluated by ICIQ- SF. Intra operative and postoperative complications were also recorded.
All the prolapse patients enrolled in the study had documented objective SUI.
In patients who needed concomitant VHand/or colporrhaphy, the TVT sling was insertedafterwards with the anterior vaginal wall incision extendedto reach the level of the mid-urethra. A Foley catheter was always inserted for 24 hours for bladderdrainage after the procedure and postvoid residual urinary volumes were measured by intermittent catheterization until patients resumed spontaneous voiding with a postvoid residual volume of less than 100ml during two consecutive micturitions.
Statistical analysis was performed using Student's t test and Mann-Whitney U test for parametric and non-parametric continuous variables respectively and the Chi-square test or Fisher's exact test, where appropriate for categorical variables. p-value <0.05 was considered statistically significant.
Results
There were no significant differences between thetwo groups with respect to patients' demographic characteristics (mean age, mean gravida, BMI, menopausal status) and urodynamicindices (Table 1).
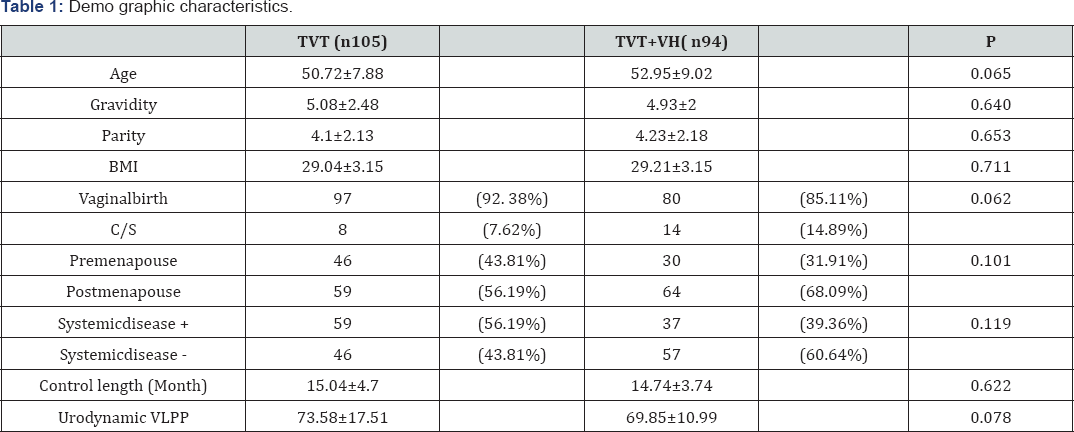
BMI: Body Mass Index
VLPP: Valsalva Leak Point Pressure
The mean durationof follow-up was 15, 04±4, 7 months in the TVT group and14, 74±3, 74 months in the TVT+VH group.
Group 1 underwent a total of 154 concomitant procedures: 90 anterior colporrhaphies, 48 posterior colporrhaphies and 16 cervical amputations. Group 2 underwent a total of 230 concomitant operations beside vaginal hysterectomy: 94 anterior colporrhaphies, 82 posterior colpoperineorrhaphies, 54 sacrospinous ligament fixation of the vaginal vault.
In group 1, two bladder perforations (2/105) occured and one patient experienced mesh rejection and mesh was removed 5 months after the operation. Urinary retantion longing more than 5 days occured for 2 patients, urethral catheterization was performed for these patients and mesh was removed from one patient 20 days after the operation and overall complication rate for group 1 was 4.76% (5/105).
In group 2, four bladder perforations (4/94) occured during surgery. Urinary retantion longing more than 5 days occured for 5 patients, urethral catheterization was performed for these patients and mesh was removed from two patients 15 and 20 days after the operation, respectively. 1 cuff enfection, 1 rectovaginal hematoma, 2 pelvic discomfort occured. 2 patients needed postoperative blood transfusion and the overall complication rate for group 2 was 15.95%(15/94). Complication rate was statistically higher for group 2 (4.76% vs 18.08% respectively, p<0.05). Distrubition of all complications developed during surgeries are shown in Table 2.

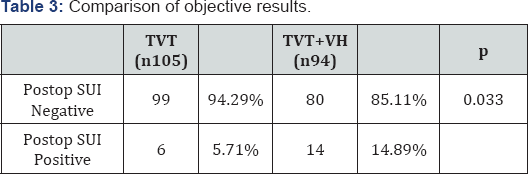
Postoperative SUI was seen significantly lower in group 1 than group 2 (5.71% vs 14.89%) and success rate was higher in group 1 ( 94.29% vs 85.11% respectively, p<0.05) (Table 3). According to our objective cure results, although successs rates of TVT for the treatment of SUI when performed with prolapsus surgery is not bad at all, if TVT is performed alone for SUI, its success rate is higher than when performed with vaginal hysterectomy.
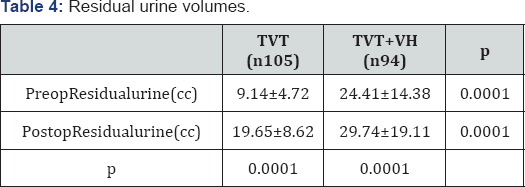
Post-voiding residuel urine volumes were significantly lower for group 1 than group 2 both preoperative and postoperatively (p=0.0001). Postoperative residuel urine volumes were significantly higher than preoperative residuel urine volumes for both group 1 and group 2 (Table 4).
When analysing the ICIQ-SF scores, our results demonstrated that TVT surgery significantly improves SUI for both groups when pre and post operative results compared. However, when we evaluated the patients according to the questions one by one, it was found that the total scores of responses that evaluated the frequency of urinary incontinence, the amount of urine that leaks and total scores were significantly higher in TVT alone group preoperatively when compared to TVT+VH group (Table 5).

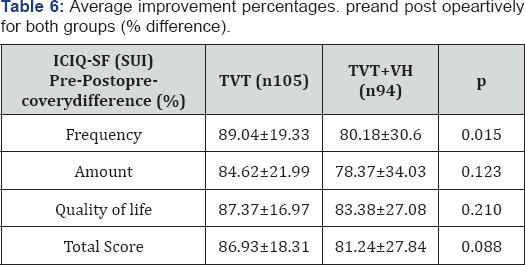
In order to interpret more precisely the outcomes of operations, the difference between pre-post operative success rates were evaluated.Recovery differences in both groups were compared between eachother, there was not a statistically significant difference for average improvement percentages (Table 6).
Discussion
TVT is a simple and effective procedure for thetreatment of female SUI. Insertion of TVT is an apparently safe procedure, as demonstrated by the low complication rate in our study. Most complications were short-term, and were managed conservatively. As these patients with SUI may also have additional problems such as uterine prolapsus or myomas, concomitant surgical proceduresto SUI surgerymay have the potential to save time and prevent the patient from the risks of another surgery scene.
Jeffry et al reported 89.3% objective cure rate and 66% subjective cure ratewith the TVT procedure and the difference between these results were statistically significant (p<0.05) [9]. On the contrary to them, our subjective cure rates were high for both groups; 86.9% for TVT alone group and 81.2% for TVT+VH group respectively (p=0.08). Yip et al. [10] reported that group having TVT with concomitant procedures have a similar cure rate when compared with the group having TVT alone after 1 year follow up (94.6% vs 93% respectively, p=0.4) [10]. Different from them we found that objective cure rates were significantly higher for TVT alone group than TVT-VH group (94.2% vs 85.1% respectively, p<0.05). Even so, our results suggest that TVT can be performed concomitantly with hysterectomy or pelvic floor reconstruction with good results.
Our mean complication rate was 18.08% (17/94) for TVT+VH group and 4.76 (5/105) for TVT group (p<0.05). Overall our complication rate was 11.05% (22/199) and it was in the ranges reported by Neuman et al. [11] and Natale et al. [12]. We experianced more bladder perforations and more postoperative urinary retentions when the TVT is performed in addition to other procedures, such as hysterectomy. Similar to us, although Houwing et al reported similar complication rates between TVT only group and TVT with prolapse repair group, they found higher estimated blood loss, longer operating time, longer length of hospital stay and longer time to normal voiding for patients TVT with prolaps repair [13]. Different from us Darai et al reported similar overall complication rates between the two groups (14/41-34% for TVT without hysterectomy group vs 14/40-30% for TVT with hysterectomy group, p>0.05) [1].
As urinary retantion is an embrassing result of TVT surgery,patients must be counseled about the occureance of this preoperatively about the risk of catheterization and tape release. However, most patients in retention can attain normal voidingwithin less than a month after the TVT procedure.
We observed that patients were significantly received beneficial effect from SUI surgery when evalauted by the responses to the pre-post operative ICIQ-SF scores. According to the ICIQ-SF (subjective evaluation) scores, the pre-post operative recovery difference in patients underwent TVT alone were foundto be statistically significantly higher than patients underwent TVT plus VH.
On the other hand, examination of patients objectively showed that the SUI positivity in postoperative period was found to be 5.71%(6/105) in TVT alone group whereas 14.89%(14/94) in TVT+VH group.
Our study showed that patients in both groups had benefit from TVT surgery but when the groups are compared according to subjective and objective results, it was appareant that the TVT alone group had statistically higher success rates than TVT+VH group.
Conclusion
In conclusion, the success rate of TVT operation is statistically significantly falling in case of incontinence surgery performed concomitantly with pelvic floor defect repair rather than TVT surgery alone.
References
- Daraï E, Jeffry L, Deval B, Birsan A, Kadoch O, et al. (2002) Results of tension-free vaginal tape in patients with or without vaginal hysterectomy. Eur J Obstet Gynecol Reprod Biol 103(2): 163-167.
- Klutke JJ, Carlin BI, Klutke CG (2000) The tension-free vaginal tape procedure: correction of stress incontinence with minimal alteration in proximal urethral mobility. Urology 55(4): 512-514.
- Ulmsten U, Johnson P, Rezapour M (1999) A 3 years follow-up of tension free vaginal tape for surgical treatment of female stress urinary incontinence. Br J Obstet Gynaecol 106(4): 345-350.
- Olsson I, Kroon U (1999) A three-year post-operative evaluation of tension-free vaginal tape. Gynecol Obstet Invest 48(4): 267-269.
- Rafii A, Paoletti X, Haab F, Levardon M, Deval B (2004) Tension-free vaginal tape and associated procedures: a case control study. Eur Urol 45(3): 356-361.
- Avery K, Donovan J, Abrams P (2001) Validation of a new questionnaire for incontinence: the international consultation on incontinence questionnaire (ICI-Q). Neurourol Urodyn 20: 86.
- Ulmsten U, Henriksson L, Johnson P, Varhos G (1996) An ambulatory surgical procedure under local anesthesia for treatment of female urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct 7(2): 8185.
- Bump RC, Mattiasson A, B 0 K, Brubaker LP, DeLancey JO (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175(1): 10-17.
- Jeffry L, Deval B, Birsan A, Soriano D, Daraï E (2001) Objective and subjective cure rates after tension-free vaginal tape for treatment of urinary incontinence. Urology 58(5): 702-706.
- Yip SK, Pang MW (2006) Tension-free vaginal tape sling procedure for the treatment of stress urinary incontinence in Hong Kong women with and without pelvic organ prolapse: 1-year outcome study. Hong Kong Med J 12(1): 15-20.
- M Neuman, Y Lavy (2007) Conservation of the prolapsed uterus is a valid option: medium term results of a prospective comparative study with the posterior intravaginal slingoplasty operation. International Urogynecology Journal Pelvic Floor Dysfunct 18(8): 889-893.
- Natale F, La Penna C, Saltari M, Piccione E, Cervigni M (2009) Voiding dysfunction after anti-incontinence surgery. Minerva Ginecol 61(2): 167-172.
- Houwing MM, Schulz JA, Flood CG, Baydock S, Rosychuk RJ (2013) A retrospective review of tension-free vaginal tape/transobturator tape procedures done concomitantly with prolapse repair. J Obstet Gynaecol Can 35(4): 340-347.






























