Case of Spontaneous Heterotopic Pregnancy in Patient with Intrauterine Contraceptive Device
Maheshgir S Gosavi*
Siraj Hospital, India
Submission: June 20, 2017 ; Published: July 06, 2017
*Corresponding author: Maheshgir S Gosavi, Bhiwandi Scan Centre, Prabhu Ali , Mandai, Bhiwandi Maharashtra, India, Tel: +91-02522-253200; Email: dentismmg@rediffmail.com
How to cite this article: Maheshgir S G. Case of Spontaneous Heterotopic Pregnancy in Patient with Intrauterine Contraceptive Device. J Gynecol Women's Health 2017; 5(5): 555674. DOI: 10.19080/JGWH.2017.05.555674.
Abstract
Heterotopic pregnancy is defined as the coexistence of intrauterine and extrauterine gestation. The incidence of heterotopic pregnancy is very low. The frequency was originally estimated on theoretical basis to be 1 in 30,000 pregnancies. We present a rare case of heterotopic pregnancy with non viable intrauterine gestation and right adnexal gestation in a natural conception.
Keywords: Transvaginal sonography; Heterotopic pregnancy; Intra-uterine contraceptive device
Case Presentation
A 32-year-old woman with 6 weeks of amenorrhea presented for emergency ultrasound scan of pelvis with clinical features of p.v.bleeding, lower abdominal pain. Urine pregnancy test was positive.
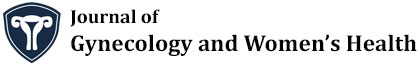
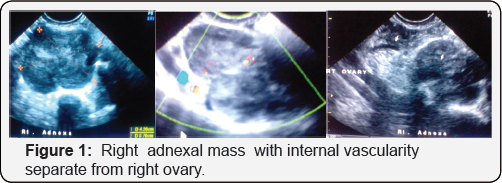
Transvaginal ultrasound revealed mild amount of free fluid in the peritoneal cavity with a intrauterine gestation corresponding to 4 weeks 4 days. Subchorionic hematoma is noted. A complex ill defined right adnexal mass measuring approximately 4.6x3.4cm was also noted (Figure 1). The Doppler study of right adnexal mass showed low resistance flow.
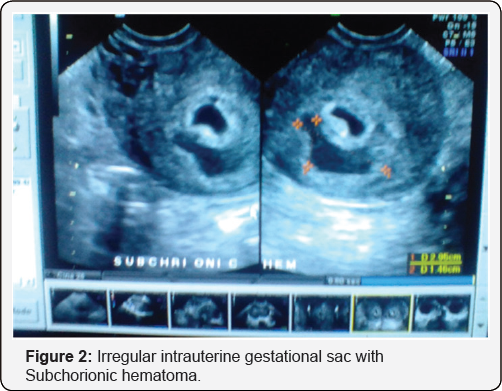
Right ovary is visualised separately from this lesion. Left ovary shows cystic lesion (corpus luteal cyst) measuring 4.6x3.4cm.
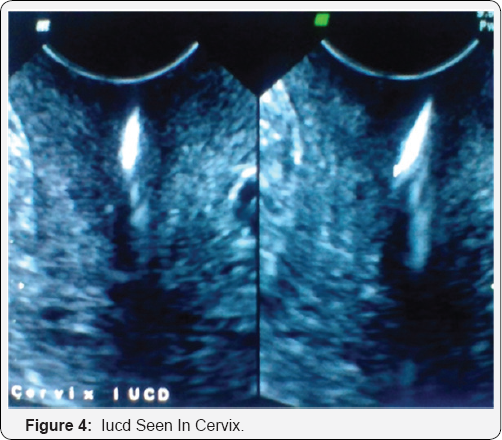
I.UC.D was seen in cervix and lower uterine cavity
Provisional diagnosis of a heterotopic pregnancy with ruptured right ectopic gestation was suggested in view of clinical history, mild amount of free intraperitoneal fluid, and an intrauterine gestation. The patient underwent emergency laparotomy. There was ruptured right-sided tubal pregnancy with hemoperitoneum and right salphingectomy was done; curettage of intrauterine pregnancy was done (Figure 2).
Pathology confirms the diagnosis of right tubal ectopic pregnancy and non viable intrauterine gestation.
Discussion
A heterotopic gestation is difficult to diagnose clinically. Typically, laparotomy is performed because of tubal pregnancy. At the same time, uterus is congested, softened, and enlarged; ultrasound examination can nearly always show gestational products in uterus.
The incidence was originally estimated on theoretical basis to be 1 in 30,000 pregnancies. However, more recent data indicate that the rate is higher due to assisted reproduction and is approximately 1 in 7000 overall and as high as 1 in 900 with ovulation induction [1].
The increased incidence of multiple pregnancy with ovulation induction and IVF increases the risk of both ectopic and heterotopic gestation. The hydrostatic forces generated during embryo transfer may also contribute to the increased risk [2] (Figure 3 & 4).
There may be an increased risk in patients with previous tubal surgeries [3].
Heterotopic pregnancy can have various presentations. It should be considered more likely
a. After assisted reproduction techniques.
b. With persistent or rising chorionic gonadotropin levels after dilatation and curettage for an induced/spontaneous abortion.
c. When the uterine fundus is larger than for menstrual dates.
d. When more than one corpus luteum is present in a natural conception.
e. When vaginal bleeding is absent in the presence of signs and symptoms of ectopic gestation [4].
A heterotopic gestation can also present as hematometra and lower quadrant pain in early pregnancy [5].
Most commonly, the location of ectopic gestation in a heterotopic pregnancy is the fallopian tube. However, cervical and ovarian heterotopic pregnancies have also been reported [6,7].
Majority of the reported heterotopic pregnancies are of singleton intrauterine pregnancies. Triplet and quadruplet heterotopic pregnancies have also been reported, though extremely rare [8,9]. It can be multiple as well [4]. They can be seen frequently with assisted conceptions.
Intrauterine gestation with hemorrhagic corpus luteum can simulate heterotopic/ectopic gestation both clinically and on ultrasound. Other surgical conditions of acute abdomen can also simulate heterotopic gestation clinically and hence the difficulty in clinical diagnosis. Bicornuate uterus with gestation in both cavities may also simulate a heterotopic pregnancy.
High resolution transvaginal ultrasound with color Doppler will be helpful as the trophoblastic tissue in the adnexa in a case of heterotopic pregnancy shows increased flow with significantly reduced resistance index.
The treatment of a heterotopic pregnancy is laparoscopy/ laparotomy for the tubal pregnancy
The illustrated case did not have any risk factor for the heterotopic gestation and presented with ruptured tubal pregnancy and history of p.v.bleeding. Patient did not suspected pregnancy as she had I.U.C.D insertion and was post partum last delivery 8 months back.
A heterotopic pregnancy, though extremely rare, can still result from a natural conception; it requires a high index of suspicious for early and timely diagnosis; a timely intervention can result in a successful outcome of the intrauterine fetus.
Conclusions
A spontaneous heterotopic pregnancy can occur in patients who have no known predisposing factor. Early diagnosis has made this disorder amenable to appropriate management. The high-resolution Transvaginal Sonography is very helpful in the diagnosis of this condition [10,11].
Acknowledgement
The author would like to thank the pathologists, gynaecologists who provided very important feedback with regard to the clinical aspect of this patient's condition. They contributed significantly to the patient being promptly diagnosed and receiving a high standard of care.
References
- Lyons EA, Levi CS, Sidney M (1998) Dashefsky in diagnostic ultrasound. In: Rumak CM, Wilson SR, Charboneau WK, (Eds.), (2nd edn), Volume 2, Mosby, p. 999.
- Glassner MJ, Aron E, Eskin BA (1990) Ovulation induction with clomiphene and the rise in heterotopic pregnancies: A report of two cases. J Reprod Med 35: 175-178.
- Gruber I, Lahodny J, Illmensee K, Losch A (2002) Heterotopic pregnancy: Report of three cases. Wien Klin Wochenschr 114(5): 229232.
- Ectopic Pregnancy, text book of -Williams Obstetrics Multifetal Ectopic Pregnancy. (21st edn), 34: 888-889.
- Cheng PJ, Chueh HY, Qiu JT (2004) Heterotopic pregnancy in a natural conception cycle presenting as haematometra. Obstet Gynecol 104(5 Pt 2): 195-198.
- Hirose M, Nomura T, Wakuda K, Ishguro T, Yoshida Y (1994) Combined intrauterine and ovary pregnancy: A case report. Asia Ocaena J Obstet Gynaecol 20: 25-29.
- Peleg D, Bar-Hava I, Neaman-Leavin M, Ashkena , Ben-Rafaelz IJ (1994) Early diagnosis and successful non surgical treatment of viable combined intrauterine and cervical pregnancy. Fertil Steril 62(2): 405408.
- Alsunaidi MI (2005) An unexpected spontaneous triplet heterotopic pregnancy. Saudi Med J 26(1): 136-138.
- Sherer DM, Scibetta JJ, Sanko SR (1995) Heterotopic quadruplet gestation with laparoscopic resection of ruptured interstitial pregnancy and subsequent successful outcome of triplets. Am J Obslet Gynecol 172(1 Pt 1): 216-217.
- Sohail S (2005) Haemorrhagic corpus luteum mimicking heterotopic pregnancy. J Coll Physicians Surg Pak 15(3): 180-181.
- Espinosa PM, Alcantar Mendoza MA (1997) Heterotopic pregnancy: Report of a case and review of literature. Ginecol Obstet Mex 65: 482486.