BMI> 30 More Likely to Require Medication Management of Gestational Diabetes
Lisa E Moore*
Department of Obstetrics and Gynecology, Texas Tech Health Sciences Center, USA
Submission: April 19, 2017; Published: June 01, 2017
*Corresponding author: Lisa E Moore, Department of Obstetrics and Gynecology, Texas Tech Health Sciences Center, 4801 Alberta Ave El Paso, Texas 79905, USA Email: lisa.e.moore@ttuhsc.edu
How to cite this article: Lisa E M. BMI> 30 More Likely to Require Medication Management of Gestational Diabetes. J Gynecol Women's Health. 2017; 5(2): 555658. DOI: 10.19080/JGWH.2017.05.555658.
Abstract
Objective: Obesity is a well-known risk factor for diabetes. We sought to determine if a high BMI also increases the risk of requiring medication to achieve euglycemia.
Methods: This is a planned secondary analysis of a cohort of women who received determination of the HbAlC at the first prenatal visit to evaluate the efficacy of the HbAlC as a triaging tool in patients at high risk of gestational diabetes. BMI was calculated at the first visit. Women with pre-existing diabetes were excluded. After delivery charts were reviewed for diagnosis of GDM and for medication use. BMI was broken up into 6 categories: underweight <18.5; appropriate weight 18.5-24.9; overweight 25-29.9; obesel 30-39.9, obese 2 40-50;obese 3>50.
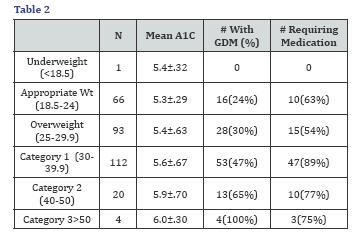
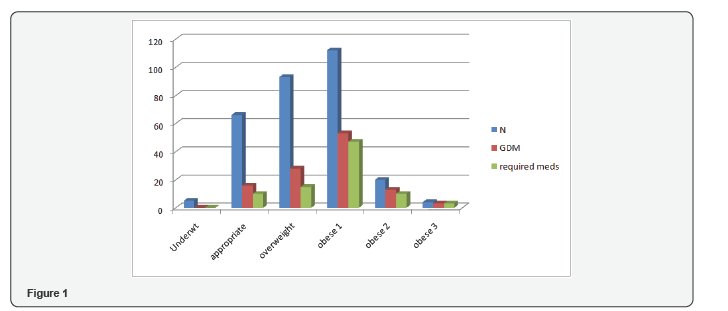
Results: 300 patients were included in the study. No patients in the underweight group had GDM. 66 patients were normal weight and 16(24%) had GDM and 10 of 16(63%) required medication. In the overweight group (N=93) 28 had GDM (30%) and 15/28(54%) required medication. In the obese 1 group (N-112); 53(47%) had GDM and 47/53(89%) required medication. Of patients in group obese 2 (N=20) 13 had GDM (65%) and 10(77%) required medication. Obese 3 contained 4 patients and all had GDM and 3(75%) required medication. BMI of 30 appeared to be a cut point. For every 1 point increase in BMI >30 there was an 8.5% increase in the odds of being on medication. A 5 point increase in BMI increased the odds of requiring medication by 50%. Patients with a BMI≥ 30 had a 3.5 fold increased risk of GDM compared to patients with in the normal weight category (95% CI = 1.3-9.4).
Conclusion: For every 1 point increase in BMI >30, the risk of requiring medication to achieve euglycemia increased by 8.5%.
Keywords: Gestational diabetes; Pregnancy; Diabetes in pregnancy, BMI
Introduction
In the United States two-thirds of adults and one-third of children are either overweight or obese [1]. The World Health Organization defines obesity in adults as a BMI ≥30 and overweight as a BMI ≥25. In 2014, 15% of women in the world were obese [2]. Gestational Diabetes (GDM) complicates between 4-14% of all pregnancies. Maternal obesity is considered the greatest risk factor for the development of GDM and of subsequent type 2 diabetes. Other complications of obesity during pregnancy include hypertensive disorders, increased risk of cesarean delivery and an increased risk of anomalies. While it is logical that a high BMI is associated with an increased risk of requiring medication to maintain euglycemia in patients with GDM, to our knowledge no studies have evaluated the association between BMI and medication usage. The goal of our study was to determine if the presumed association between BMI and the need for medication to control blood glucose levels is factual.
Materials and Methods
This is a planned secondary analysis of a prospective cohort study looking at Hemoglobin A1C at the first prenatal visit.
To be included in the study, patients had the first prenatal visit prior to 20 weeks and no history of type 1 or type 2 diabetes. Patients with GDM in a previous pregnancy were eligible for inclusion if there was no diagnosis of diabetes other than in pregnancy. BMI was calculated at the first prenatal visit and Hemoglobin A1C (A1C) was included as part of routine prenatal labs.
Patients were diagnosed with Gestational Diabetes (GDM) by two step testing according to the American College of Obstetrics and Gynecology (ACOG) guidelines. The testing was performed between 24-28 weeks using an initial 50 g oral glucose challenge and a 1 hour cutoff of 130mg/dl (7mmol/L). Patients with a 1 hour value ≥130mg/dl received a 100g oral glucose challenge with determination of glucose levels fasting, and at one, two and three hours. Cutoffs for each value were fasting >95mg/ dl (5.3mmol/L); 1 hour >180mg/dl (10.0mmol/L); 2 hour >155mg/dl (8.6mmol/L) and 3hour >140mg/dl (7.8mmol/L). Two abnormal values were considered diagnostic of GDM.
Medication use was defined as any oral antidiabetic agent or any type of insulin used to control blood glucose. Per protocol, medication was started when 20% of values failed to meet glycemic goals for two consecutive weeks. Glycemic goals were fasting<95mg/dl (5.3mmol/L) and a one-hour postprandial< 140mg/dl (7.8mmol/L).
BMI was separated into 6 categories: Underweight BMI <18.5; Appropriate weight BMI between18.5-24.0; Overweight BMI between 25-29.9; obese 1 BMI between 30-39.9; obese 2 BMI between 40-50;obese 3 BMI >50.
Statistical Analysis
Statistical analysis was performed using the SAS package version 9.3. Logistic regression was used to calculate the odds of being on medicine based on BMI. Tukey multiple comparison procedure was used to compare A1C means in each group.
Results
Two-hundred and ninety-six patients were included in the analysis.
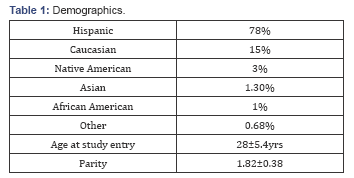
Demographics are shown in Table 1. The majority of the patients in the study (78%) were Hispanic. The next largest ethnic group was Caucasian (15%) followed by Native American, Asian, African American, and Other who each represented less than 5% of the study population. The average age at entry into the study was 28 years. The average parity for patients in the study was greater than one previous child.
No underweight patients were diagnosed with GDM. There was no difference in medication use between appropriate weight patients and patients in the overweight BMI category (63% and 54% respectively). There was also no difference in medication use between patients with a BMI in obese2 (77%) compared to obese 3 (100%). There was a significant difference in medication use between appropriate weight (63%) and obese 1 (89%) (P=.01); and between overweight (54%) and obese 1(89%) P=.0004.
As shown in Table 2, A1C increased as BMI increased but BMI was a better predictor than A1C of being diagnosed with GDM and of requiring medication for management of GDM. The change in A1C as BMI increased did not reach statistical significance for any category of BMI. As expected, BMI was an independent risk factor for GDM.
For every 1 point increase in BMI above 30, the risk of requiring medication increased by 8.5%. A five point increase in BMI increased the odds of being on medication by 50% and a 10 point increase in BMI increased the odds of requiring medication by 126%.
Comment
In our study a BMI ≥30 appeared to be a threshold beyond which the risk of both GDM and of requiring medication for management of GDM increased. To our knowledge no studies have evaluated the BMI during pregnancy as a risk for GDM and for medication use for GDM management
The Nurse Health Study II looked at 14613 women with no history of diabetes who had singleton pregnancies. 722 (4.9%) developed GDM. In that study a BMI of 25 at age 18 was a strong predictor of developing GDM [3].
A meta-analysis of studies evaluating pre-pregnancy BMI and the risk of GDM found that the odds ratio for BMI 25-29 was 1.97 and for BMI >30 was 3.76. [4] Our study is consistent with these findings.
Screening for GDM may be undertaken based on risk factors or may be performed universally. A BMI >30 is considered a risk factor for GDM and based on the results of our study it is also a risk factor for requiring medication to control blood glucose. This information may be useful in preconception counseling and in counseling women with a new diagnosis of GDM.
Author Contribution
Lisa E Moore, MD is the sole author of this work.
Institutional Review Board Statement
This study was approved by the institutional review board at the University of New Mexico and assigned number 11-414.
Informed Consent Statement
This study is a secondary analysis and was deemed exempt by the IRB.
Conflict of Interest Statement
Lisa E. Moore, MD has no conflicts of interest related to the manuscript.
Data Sharing Statement
No additional data available.
Core Tip
A BMI >30 is associated with an increased risk of requiring medication for management of gestational diabetes. For every 1 point increase in BMI > 30, the risk of requiring medication to treat gestational diabetes increased by 8.5%.
Citation
Moore LE BMI > 30 more likely to require medication management of gestational diabetes mellitus.
References
- Overweight and Obesity Statistics 2016.
- WHO (2016) Obesity and Overweight 2016. World Health organization, Geneva, Switzerland.
- Solomon CG, Willett WC, Carey VJ, Rich-Edwards J, Hunter DJ, et al. (1997) A prospective study of pregravid determinants of gestational diabetes mellitus. Jama 278(13): 1078-1083.
- Torloni MR, Betran AP, Horta BL, Nakamura MU, Atallah AN, et al. (2009) Prepregnancy BMI and the risk of gestational diabetes: a systematic review of the literature with meta-analysis. Obes Rev 10(2): 194-203.






