Laparoscopic Surgery of Massive Ovarian Edema: A Case Report and Literature Review
Yuji Tanaka*, Mayuko Nagasaka, Mariko Takahashi and Masashi Kobayashi
Department of Obstetrics and Gynecology, Kohka Public Hospital, Japan
Submission: March 08, 2017 ; Published: March 17, 2017
*Corresponding author: Yuji Tanaka, Department of Obstetrics and Gynecology, Kohka Public Hospital, Minakuchichomatsuo 1256, Koka, Shiga, 528-0074, Japan, Tel: +81-748-62-0234; Email: fcyxw581@gmail.com
How to cite this article: Yuji T, Mayuko N, Mariko T, Masashi K. Laparoscopic Surgery of Massive Ovarian Edema: A Case Report and Literature Review. J Gynecol Women's Health. 2017; 3(2): 555607.DOI:10.19080/JGWH.2017.03.5555605
Abstract
Massive ovarian edema (MOE) is a rare benign clinical entity that can be confused with neoplastic ovarian tumor. Usually, ovarian torsion develops secondary to an ovarian tumor, but at times, it might develop even in a normal ovary. Most MOE occurs because of intermittent torsion of the normal ovary and compromised venous or lymphatic drainage, which subsequently involve the arteries. The major symptoms of MOE are abdominal pain, due to torsion of the stem. Since it is not a neoplastic disease, a therapy that preserves fertility should be the principle of treatment. We present here, our case along with a literature review on the subject. A 9-year-old girl was admitted in our hospital with abdominal pain and was diagnosed with MOE based on ultrasonography and Magnetic Resonance Imaging findings. After the first onset, conservative therapy with analgesics was administered for about 7 months during repeat exacerbations. A second episode of severe abdominal pain occurred after 7 months. Although ovarian blood flow was preserved on imaging investigations, laparoscopic surgery was performed due to increasing pain. Untwisting and wedge resection of the ovary and ovarian fixation was performed. Clinical follow-up at 5 months using ultrasonography examination revealed no recurrence of the torsion. If the ovarian blood flow is maintained as in this case, conservative treatment is possible, but surgical therapy is considered if there is a worsening of symptoms such as pain or absence of ovarian blood flow. Laparoscopic surgery for untwisting the torsion is initially recommended. Wedge resection of the ovary should be considered. There are pros and cons for ovarian fixation, but it should be enforced in cases where there is a concern about revolving easily.
Keywords: Massive ovarian edema; Ovarian torsion; Laparoscopic surgery
Abbreviations: MOE: Massive Ovarian Edema; CT: Computed Tomography; MRI: Magnetic Resonance Image
Introduction
Massive ovarian edema (MOE) is a rare benign clinical entity that could be confused with neoplastic ovarian tumor. The average age of patients with MOE is about 20years [1,2]; hence, preserving the ovary should be the goal of therapy for these patients, in order to preserve hormonal function and fertility. We report a case where we preserved the ovaries and prevented recurrence through conservative treatment and laparoscopic surgery. We also present a literature review for this condition.
Case Presentation
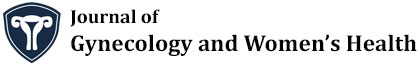
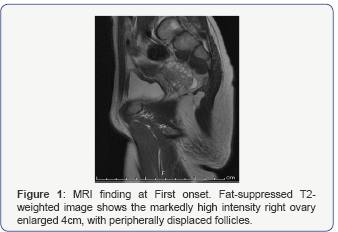
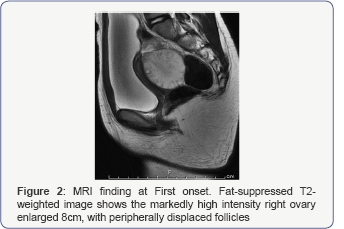
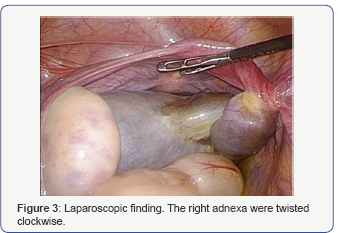
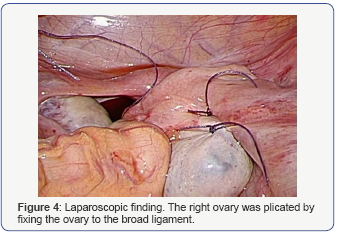
A female patient aged 9 years was admitted with a history of right abdominal pain of 3days duration. Ultrasonography revealed a partly solid and cystic mass with thick contents and measuring 4cm, arising from the right ovary. The mass appeared to be freely mobile, with a smooth surface. Ovarian blood flow was preserved. Computed Tomography (CT) revealed similar findings. T2-weighted abdominal magnetic resonance images (MRI) showed asymmetric ovarian enlargement in a teardrop configuration, hyper intense peripherally displaced follicles, and twisting of the vascular pedicle between the enlarged ovary and uterus (Figure 1). On laboratory investigations, the hormonal levels were in the normal range as expected in a female before menarche. Tumor markers were under the limits. A diagnosis of MOE was made. Conservative treatment with analgesics was success. A second episode of severe abdominal pain occurred 7 months later. Ultrasonography and MRI showed that the right ovary was enlarged to 8cm (Figure 2). Conservative treatment with analgesics and defecation and bladder catheterization was administered for 3days. Although ultrasonography showed that the ovarian blood flow was preserved; laparoscopic surgery was performed due to severe, increasing pain. On laparoscopy, the right ovary was enlarged, edematous (8cm), rotated by 540 degrees, and displaced to the posterior side of the broad ligament (Figure 3). The surface of the right ovary was reddish brown. The left ovary was slightly enlarged (4cm). The uterus appeared normal in shape and size. After untwisting the ovarian ligament and the fallopian tube, wedge resection of the right ovarian cysts was performed. After untwisting, the color of the ovary promptly returned to white and pink. The right ovary was fixing the ovary to the broad ligament, as the ligament was extended and the risk of re-twisting was high (Figure 4). The postoperative period was uneventful. On the fifth postoperative day, ultrasonography revealed shrinkage of the right ovarian diameter to 6cm. She was discharged on the sixth postoperative day. Histopathological findings showed noneoplastic change, but presence of MOE. At 5 months post-surgery, no recurrence was seen, and the ovaries we real most normal size.
Discussion
MOE was first described by Kalstone et al. [3], and is defined by WHO Formation of a tumour-like enlargement of one or both ovaries by oedema fluid [4]. MOE patients are between 6 and 33 years of age, and the average age is 21 years [1,2,4].
There are two types of MOE: primary MOE occurs when the ovary is not diseased but there is torsion or twisting of the ovarian pedicle to the extent that it interferes with the venous and lymphatic drainage leading to edema, but does not affect the arterial blood flow. The major symptoms of primary MOE are acute or chronic pain, and the duration of pain depends on the character of the torsion [5]. The condition frequently occurs on the right side; accounting for about 75% of cases [6], probably due to higher pressure in the right ovarian vein caused by the distinct anatomy of venous drainage from the right ovary [7]. Secondary MOE occurs in a diseased ovary, such as ovarian tumor [8-12] and malignant tumor [13-15], or in patients on hormonal therapy for ovulation induction [16]. Various theories have been postulated about the mechanism of onset of secondary MOE [17]; however, there is no established mechanism yet. Of all MOE cases, 85% are primary, and 15% are secondary [5].
In the past, pre-operative diagnosis of MOE was difficult, and most cases were diagnosed based on the postoperative pathological findings. Many cases were over-treated due to the confusion with ovarian malignant tumors. In a series by Praveen et al. [5] 82% of the cases were subjected to salpingo-oophorectomy and 7% to total hysterectomy and bilateral oophorectomy; only 11% patients under went fertility-preserving surgery [5]. However, in the current times, MRI and ultrasonography enable a precise preoperative diagnosis. The typical findings on MRI and ultrasonography are multiple cysts at the peripheral cortex of an enlarged ovary. The image findings depend on histological characteristics [18-21]. Histological, multiple ovarian follicles at the peripheral cortex and edematous ovarian stroma are seen, and the ovarian architecture is preserved [22].
An important aspect of treating young women with MOE is the preservation of fertility and preventing multiple surgeries. There are two possible approaches to MOE: conservation therapy or surgical treatment. Guvenal et al. [23] reported that MOE could be managed conservatively, if ovarian blood flow is maintained on ultrasonography, as in our case, conservative treatment should be the first choice of therapy. Conservative treatment of MOE includes administration of analgesics, indwelling catheterization of the bladder and/or injection of saline into the bladder, aiding defecation, and waiting for a natural untwisting of the ovarian torsion. Surgical therapy is necessary if there is a worsening of symptoms such as pain or absence of ovarian blood flow. Laparoscopic surgery is recommended, since it is less invasive than laparotomy, and offers both diagnostic and therapeutic advantages [24-28]. Laparoscopic untwisting of the ovarian torsion is the basic surgery for primary MOE. However, the optimal surgical procedure following untwisting of the ovarian torsion is still unknown. There are two surgical options, wedge resection of massive ovary or ovarian fixation. Prevention of recurrence of the torsion is expected due to volume reduction in wedge resection [25,26,28], but formation of adhesions is a cause for concern. If the diagnosis of MOE cannot be confirmed on preoperative investigations, or a malignant tumor is suspected, histological analysis of the frozen sample obtained during wedge resection of the ovary can lead to a confirmatory diagnosis [27]. Some authors have recommended fixation of the ovary to the posterior aspect of the uterus or broad ligament or round ligament, for prevention of torsion recurrence [28-30]. Some other authors do not recommend ovarian fixation surgery as this might reduce the blood flow and function of the ovary [31], and might not prevent recurrence. The type of surgical technique to be employed needs to be individualized for each case.
Acknowledgment
The authors would like to thank Dr. Michio Yamasaki and Katsuji Imoto for their help with radiological considerations.
Conflict of Interest
The authors report no declarations of interest.
References
- Geist RR, Rabinowitz R, Zuckerman B, Shen O, Reinus C, et al. (2005) Massive edema of the ovary: a case report and review of the pertinent literature. J Pediatr Adolesc Gynecol 18(4): 281-284.
- Coakley FV, Glenn OA, Qayyum A, Barkovich AJ, Goldstein R, et al. (2004) Fetal MRI: a developing technique for the developing patient. AJR Am J Roentgenol 182: 243-252.
- Kalstone CE, Jaffe RB, Abell MR (1969) Massive edema of the ovary simulating fibroma. Obstet Gynecol 34(4): 564-571.
- WHO (2003) WHO classification of tumours, Tumours of Breast and Genital Organs 2003. IARC Press, France, pp. 190.
- Praveen R, Pallavi VR, Rajashekar K, Usha A, Umadevi K, et al. (2013) A clinical update on massive ovarian oedema- a pseudotumour? Ecancermedical science 7: 318.
- Hall BP, Printz DA, Roth J (1993) Massive ovarian edema: ultrasound and MR characteristics. J Comput Assist Tomogr 17(3): 477-479.
- Li YT, Kuon LC, Lee PN, Kuo TC (2005) laparoscopic Detorsion of Twisted Ovary. Journal of the Chinese Medical Association 68(12):595-598.
- Gehrig PA, Fowler WC, Lininger RA (2000) Ovarian capillary hemangioma presenting as an adnexal mass with massive ascites and elevated CA-125. Gynecol Oncol 76(1): 130-132.
- Hameed A, Ying AJ, Keyhani-Rofagha S, Xie D, Copeland LJ (1997) Ovarian mucinous cystadenoma associated with mural leiomyomatous nodule and massive ovarian edema. Gynecol Oncol 67(2): 226-229.
- Khalbuss WE, Dipasquale B (2006) Massive ovarian edema associated with ovarian serous cystadenoma: a case report and review of the literature. Int J Gynecol Cancer 16(Suppl 1): 326-330.
- Lakhey M, Upreti D, Kulshrestha R, Rani S (2003) Massive ovarian edema with contralateral mature cystic teratoma–a case report of an uncommon combination. Indian J Pathol Microbiol 46(2): 219-221.
- Sakaki M, Hirokawa M, Horiguchi H, Wakatsuki S, Sano T, et al. (2000) Ovarian fibrothecoma with massive edema. J Med Invest 47(3-4): 148-151.
- Krasevic M, Haller H, Rupcic S, Behrem S (2004) Massive edema of the ovary. A report of two cases due to lymphatic permeation by metastatic carcinoma from the uterine cervix. Gynecol Oncol 93(2): 564-567.
- Bazot M, Detchev R, Cortez A, Uzan S, Darai E (2003) Massive ovarian edema revealing gastric carcinoma: a case report. Gynecol Oncol 91(3): 648-650.
- Wong SY (1989) Bilateral massive ovarian oedema-report of a case due to lymphangiitiscarcinomatosa. Virchows Arch A Pathol Anat Histopathol 414(4): 355-358.
- Patty JR, Galle PC, McRae MA (1993) Massive ovarian edema in a woman receiving clomiphene citrate. A case report. J Reprod Med 38(6): 475-479.
- Machairiotis N, Stylianaki A, Kouroutou P, Sarli P, Konstantinos N, et al. (2016) Massive ovarian oedema: a misleading clinical entity. Diagn Pathol 11: 18.
- Coakley FV, Anwar M, Poder L, Wang ZJ, Yeh BM, et al. (2010) Magnetic resonance imaging of massive ovarian edema in pregnancy. J Comput Assist Tomogr 34(6): 865-867.
- Umesaki N, Tanaka T, Miyama M, Nishimura S, Kawamura N, et al. (2000) Successful preoperative diagnosis of massive ovarian edema aided by comparative imaging study using magnetic resonance and ultrasound. Eur J Obstet Gynecol Reprod Biol 89(1): 97-99.
- Umesaki N, Tanaka T, Miyama M, Kawamura N (2000) Sonographic characteristics of massive ovarian edema. Ultrasound Obstet Gynecol 16(5): 479-481.
- Gobara A, Yoshizako T, Yoshida R, Okada N, Makihara K, et al. (2016) Magnetic resonance imaging features of massive ovarian edema in pregnancy: utility for decisions in expectant management. Springer plus 5(1): 1444.
- Roth LM, Deaton LM, Sternberg WH (1979) Massive ovarian oedema. A clinicopathological study of five cases including ultra structural observations and review of the literature. Am J Surg Pathol 3(1): 11-21.
- Guvenal T, Cetin A, Tasyurt A (2001) Unilateral massive ovarian edema in a woman with polycystic ovaries. Eur J Obstet Gynecol Reprod Biol 99(1): 129-130.
- Cohen SB, Wattiez A, Seidman DS, Goldenberg M, Admon D, et al. (2003) Laparoscopy versus laparotomy for detorsion and sparing of twisted ischemic adnexa. JSLS 7(4): 295-299.
- Kallipolitis G, Sklia E, Milingos S, Michalas S (1999) Laparoscopic treatment of massive ovarian edema. J Am Assoc Gynecol Laparosc 6(4): 513-516.
- Kocak M, Caliskan E, Haberal A (2002) Laparoscopic conservation of the ovaries in cases with massive ovarian oedema. Gynecol Obstet Invest 53(2): 129-132.
- Cepni I, Ocal P, Erkan S, Saricali FS (2005) Massive edema of the ovary diagnosed with laparoscopic biopsy and frozen section. J Postgrad Med 51(4): 336-337.
- Cheng MH, Tseng JY, Suen JH, Yang CC (2006) Laparoscopic plication of partially twisted ovary with massive ovarian edema. J Chin Med Assoc 69(5): 236-239.
- Grunewald B, Keating J, Brown S (1993) Asynchronous ovarian torsion--the case for prophylactic oophoropexy. Postgrad Med J 69(810): 318-319.
- Fuchs N, Smorgick N, Tovbin Y, Ben Ami I, Maymon R, et al. (2009) Oophoropexy to prevent adnexal torsion: how, when, and for whom? J Minim Invasive Gynecol 17(2):205-258.
- Breech LL, Hillard PJ (2005) Adnexal torsion in pediatric and adolescent girls. Curr Opin Obstet Gynecol 17(5): 483-489.