To Study Association of Female Genital Tuberculosis Symptomatology with Endometrial Biopsy Tb Pcr
Indu gautam1, Shantanu vyas2*, Charul vyas3, Chand kishan vyas4
1Department of obstetrics and gynaecology,SMS Medical College, Jaipur
2Department of plastic surgery SMS Medical College, Jaipur
3Department of radio diagnosis, Mgmch medical college, jaipur
44Department of aneasthesiology, SMS Medical College, Jaipur
Submission: October 19, 2016 ; Published: December 01, 2016
*Corresponding author: Shantanu Vyas, Sms Medical college, ajmer road, J 65 a tagore Nagar, Jaipur, 302019, India Tel:9214010448; Email:dr.shanuvyas@gmail.com
How to cite this article:Indu g, Shantanu v, Charul v, Chand kishan v. To Study Association of Female Genital Tuberculosis Symptomatology with Endometrial Biopsy Tb Pcr. J Gynecol Women’s Health. 2016; 1(5): 555574 DOI: 10.19080/JGWH.2016.01.555574
Introduction
More than 2 billion people, equal to one-third of the world’s population are infected with tuberculosis (TB) bacilli. 1 in 10 people with TB bacilli will become sick with active TB in their lifetime1. TB exists in two forms; pulmonary tuberculosis and extra-pulmonary tuberculosis. Genital tuberculosis is one form of extra pulmonary TB that affects about 12% of patients with pulmonary tuberculosis and represents15-20% of extra-pulmonary tuberculosis 2. It is estimated that 5-13 percent of the females presenting in infertility clinics in India have genital TB and majority are in the age group of 20-40 years 3. Moreover, it is also estimated that at least 11% of the patients lack symptoms and genital TB is often detected in diagnostic workup of women attending infertility clinics4. In genital TB; the fallopian tubes are affected in almost 100% followed by the endometrium in 50%, ovaries in 20%, cervix in 5% and vagina and vulva in 1%5-6. There is no way to take the fallopian tube out, but a specimen from the endometrium can be taken to detect genital TB. Early diagnosis of tuberculosis and initiating optimal treatment would not only enable a cure of an individual patient but will also curb the transmission of infection and disease to others in the community. Conventional diagnostic tests, excluding culture method, are unable to detect active tuberculosis. Culture method is still corner stone on which definitive diagnosis of tuberculosis relies, but it is time consuming due to very slow growth of Mycobacterium7. Molecular methods like polymerase chain reaction (PCR) are highly specific, sensitive and very fast as compared to the gold standard culture method. BD MGIT (Mycobacteria Growth Indicator Tube) system is a rapid and sensitive method, amongst other culture methods, for early diagnosis of pulmonary and extrapulmonary TB but for maximum recovery of Mycobacteria; a combination of both MGIT and LJ media should be used8. False positive cases reported in TB
PCR are basically because of contamination of clinical specimens with M.tuberculosis DNA product from the PCR laboratory. A special negative control (template RNA without RT enzyme) has been introduced in our assay to check the DNA contamination. Considerable work has already gone into resolving the problem of contamination 9-11.
Therefore, we have focused on the issues of preserving microbial viability in endometrial tissue specimens and STN RT-PCR. In viable Mycobacteria; there is plasmid DNA, 16S rRNA and mRNA while, in dormant stage of Mycobacteria; there is DNA and 16S rRNA and in dead stage; there is only DNA present in Mycobacteria. We took advantage of the fact that mycobacterial mRNA has an extremely short half-life, averaging only 2-3 minutes12, so by targeting mycobacterial mRNA by the reverse transcription PCR (RT-PCR) would indicate the presence or absence of recently viable organism. Moreover, the nested RT-PCR would make the procedure more reliable for diagnostic purposes because it can detect even single copy of the gene of MTB; hence it is highly specific and sensitive than RT-PCR. The mRNA coding for the ubiquitous 85 B antigen protein is known to be secreted in large quantities from growing Mycobacteria13.
Declared global emergency in 1993 by WHO - 9.4 million annually affected, 2 million deaths Indian scenario 2.2 Million annually affected ; 0.2 million deaths FGTB in 1-19%
Material and Method
The present study was undertaken to detect mycobacterial infection in endometrial biopsy samples by PCR and find its relation to symptomatology. A total of 50 women with infertility attending out-patient department of Zenana Hospital, Jaipur were included in the study. Male factor infertility and other known cause of infertility were excluded.
Detailed information encompassing socioeconomic status, complaints, past & present medical and surgical history and family history of TB & ATT was obtained. General examination done. Endometrial biopsy sample collected for PCR. Acc. to PCR report two groups formed, PCR +ve and PCR-ve. Tabulation of observations done and comparisons made.
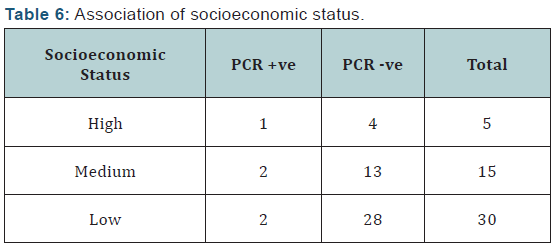
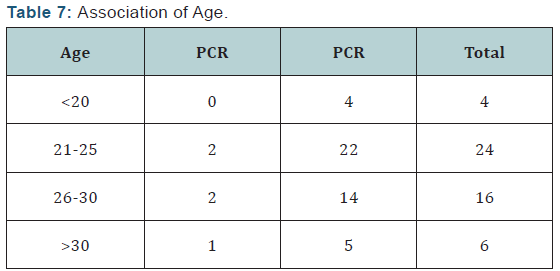
Diagnosis of genital tuberculosis was made in 10 %( n-5) of women in study group by PCR. PCR has high sensitivity (31.3%) and specificity. P Kumar et al. [1], Jindal UN et al. [2] concluded that endometrial TB PCR has high specificity and sensitivity. Highest occurrence was in age group 21-30 yrs, although not significantly associated. Mridu Manjari et al. [3] showed Tuberculosis Endometriotic peak in 20-30 yrs age. In this study 60% of women were of lower socioeconomic strata. Gupta N & J B Sharma [4] support this.
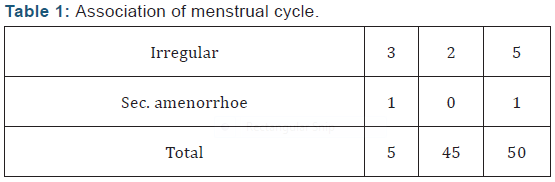
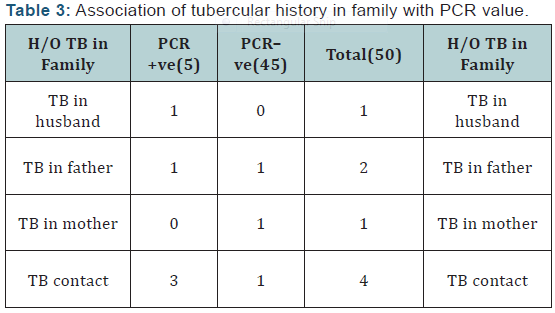
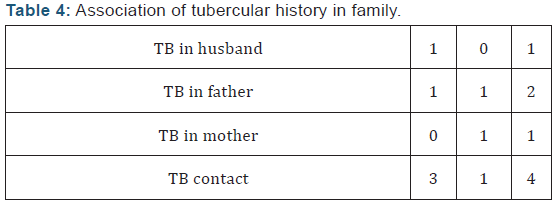
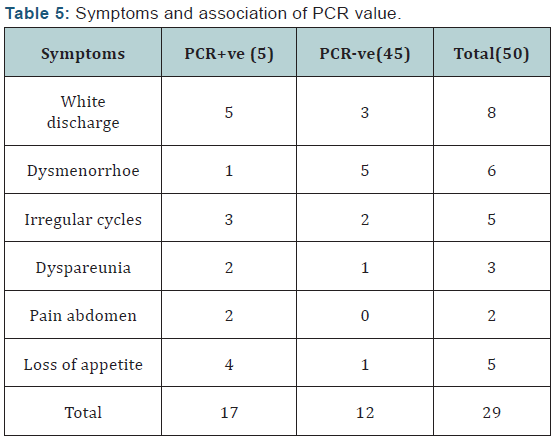
Menstrual disturbance, vaginal discharge and pain abdomen were significantly associated. Family history and self history of tuberculosis was also significantly associated. P Kumar et al. [1] also show significant association.
Conclusion
Hence women with infertility having other gynaecological complaints should necessarily be offered PCR early so as to ensure diagnosis and treatment of FGTB before other interventions. Suman Puri et al. [5] concluded that PCR has increased sensitivity in determining FGTB and significant number of patients conceived after regular ATT Table(1),Table(2),Table (3),Table(4),Table(5),Table(6) and Table(7).

References
- Kumar P, Shah NP, Singhal A, Chauhan DS, Katoch VM, et al. (2008) Association of Tuberculous Endometritis with infertility and other gynaecological complaints of women in India. J Clin Microbiol Dec 46(12): 4068-4070.
- Jindal UN, Bala Y, Sodhi S, Jindal S (2010) Female genital tuberculosis: Early diagnosis by laparoscopy and endometrial polymerase chain reaction. Int J Tuberc Lung Dis 14(12): 1629-1634.
- Manjari M, Khanna S, Arora U, Kahlon Sk, Laxmi gulati V, et al. (1995) Tuberculous endometritis in strile females: A clinocopathological and bacteriological study. Ind J Tub 42(4): 227-228.
- Gupta N, Sharma JB, Mittal S, Singh N, Misra R, et al. (2007) genital TB in Indian infertility patients. Int J Gynaecol Obstet 97 (2): 135-138.
- Puri S Bnsal B (2009) Diagnostic value of PCR in female TB leading to infertility and conception rate after ATT. JK Science 11 (1): 31-33.







