Practices for Prevention, Therapy of Primary Dysmenorrhoea
S Chhabra* and S Gokhale
Obstetrics Gynaecology, Mahatma Gandhi Institute of Medical Sciences, India
Submission: July 23, 2016; Published: August 08, 2016
*Corresponding author: S Chhabra, Director Professor, Obstetrics Gynaecology, Mahatma Gandhi Institute of Medical Sciences, Sevagram- 442102, Wardha, Maharashtra, India.
How to cite this article: S Chhabra, S Gokhale. Practices for Prevention, Therapy of Primary Dysmenorrhoea. J Gynecol Women’s Health. 2016; 1(3): 555563. DOI: 10.19080/JGWH.2016.01.555563
Abstract
Background: Dysmenorrhea is very common gynaecologic disorder which distresses girls, curbs their daily activities, causes social withdrawal. Girls use all sorts of remedies, some on their own, due to practices in family, some after consultation.
Objectives: Present prospective study was carried out with aim of knowing remedies used, including change in life style for prevention, treatment of dysmenorrhea.
Materials & Methods: Post menarcheal adolescent girls (282) from four schools, around institution, and 100 first year medical/nursing students of study place, were randomly interviewed.
Results: Among school girls 197 (69.85%) had dysmenorrhoea, 74.5 % of 185 urban, 60.82% of 97 rural. Of medical/nursing students 65.75% of 73 urban, 51.85 % of 27 rural students, reported dysmenorrhoea. Overall 197 school girls had dysmenorrhoea, 60(30.45%) of 197 school girls said pain was aggravated with everyday work. Of 118 between 14-15 yrs, 81(68.64%) resorted to rest, 19 (16.10%) to hot fomentation and 10(8.4%) analgesics. Other methods used were lying down prone, doing yogic exercises, putting asafetida in naval region and drinking milk with turmeric. There was no difference in practices in different economic classes, 76% girls from upper, upper-middle class, 69.35% of lower class resorted to rest. Analgesics were used by 8.1% from upper, upper-middle class, 8.9% of lower class. However more of lower economic class girls resolved to kitchen medicine, 8.9% against 2.7% upper class.
Among nursing/medical students, 48.38% with dysmenorrhoea reported that pain was aggravated by exercise like jogging, aerobics which they abandoned during menstruation, 25.80% reported aggravation with walking, climbing stairs, 19.35% with any work. Overall most girls reported that work, exercise aggravated and rest relieved pain. Of medical/nursing students, 79.03% resorted to analgesics and 19.35% to rest for pain relief. Of 29 medical/nursing students of 21-22 years with dysmenorrhea, 16(55.17%) reported pain aggravated with exercise, 5(17%) daily work, 5(17%) while walking. No nursing /medical student reported having consulted doctor for dysmenorrhoea, although self medication, analgesics were used by 79% (49 of 62). Of school girls 9.42% (13 of 138) urban, 3 of 59(5.08%) rural had sought help from doctor. However 7(16.66%) out of 42 school girls with severe pain, (on a scale of 3), 12 (10%) out of 120 with moderate pain and 3 (8.5%) out of 35 with mild pain had sought help from nurses, teachers, village health workers, traditional birth attendants (TBA) and quacks.
Overall of 282 school girls, 207 (73%) did not alter their food habits during menstruation, 168(81.15%) had dysmenorrhoea .Seventy five (27%) girls changed their diet as per family practices, 29 (38.6%) of them reported dysmenorrhoea. Of 100 medical/nursing students, 53 (53%) did not change food habits, 47 (49%) had dysmenorrhoea and 47(47%) avoided certain food items to prevent pain and reduce bleeding, 15 (32%) of them had dysmenorrhoea.
Conclusion: Dysmenorrhoea is highly prevalent in adolescents and lots of learning/working hrs are lost. Simple measures are taken as family practices. Since dietary, life style changes during menstruation were reported to be beneficial in reducing pain ,even blood loss, research is needed which will not only help in prevention, treatment of dysmenorrhoea but might provide information which may be useful for other disorders . Also research with reverse pharmacology needs to be explored.
Keywords: Dysmenorrhoea; Practices; Prevention; Therapies
Background
Primary dysmenorrhea, pain during menstruation in the absence of any identifiable pelvic disorder is the most common menstrual disorder and is reported to occur in 30 to 50% of young women; though the real numbers are not known [1-3]. During the last decade, substantial progress has been made towards understanding the nature and the potential management of dysmenorrhea; however it still manages to confound clinicians [4]. Disappointed clinicians tend to adopt a nihilistic approach even when dysmenorrhoea is severe, dismiss the disorder as a normal physiological event and even label the girls as neurotic. Although it is only temporarily disabling, its regularity, frequency and effects make it worthy of renewed appraisal.
Objective
Prospective study was carried out with the objective of knowing modalities used by young girls for prevention and treatment of primary dysmenorrhea.
Materials & Methods
Four schools, in and around Sevagram were chosen randomly looking at the access and necessary approvals were taken. Post menarcheal girls, making a total of 282 coming from villages and townships of age between 12-19 years were interviewed with the help of a predesigned, pretested tool for collecting information about treatment/advice sought, dietary habits for prevention and/ or treatment of dysmenorrhoea. For detail analysis the girls were divided according to the presence or absence of dysmenorrhoea. Of 282 school girls, 197(69.86%) had dysmenorrhoea, of 185 urban 138(74.5) and of 97 rural, 59 (60.82%) (P<0.016 significant difference) Of 197 girls with dysmenorrhoea, 29(14.7) were of 12- 13 years, 118(59.89%) 14-15 years, 40 (20.30%) 16-17 years and 10(5.07%) 18-19 years. Three (1.06%) were from upper economic class, 13(6.5%) upper-middle, 58(29.44%) middle, (30.96%) lower-middle and 62(31.47%) lower EC. Out of 100 medical and nursing students, 10 were from upper EC, 32 from upper-middle, 45 from middle and 13 from lower-middle class, no one was from lower EC. All medical and nursing students were of 18 to 25 years, 73 belonged to cities, 48(65.75%) of them and 14(51.85%) of 27 rural had dysmenorrhoea (P=0.203 insignificant difference). Of total 62 medical /nursing students with dysmenorrhea, 29(80.56%) of 36 of 21-22 years, 20(52.63%) of 38 of 19-20 years, 9 (81.81%) of 11 of 23-24 years and 4 (26.66%) of 15 were around 18 years.
Results
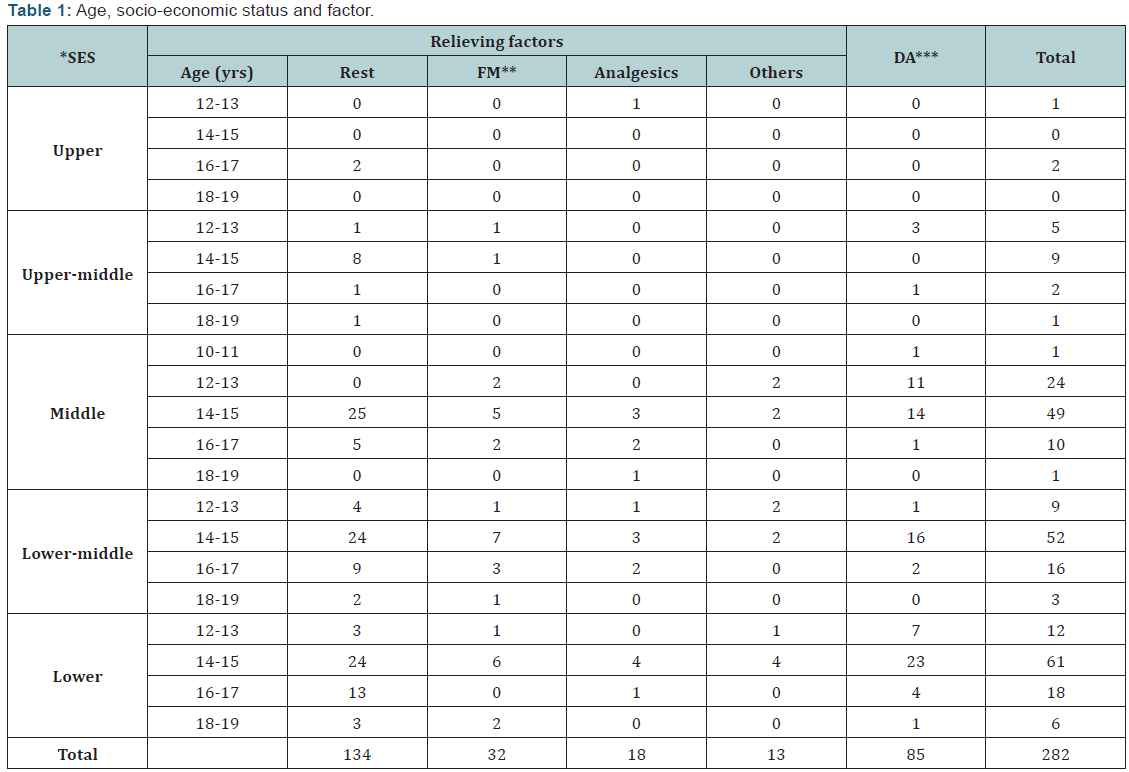
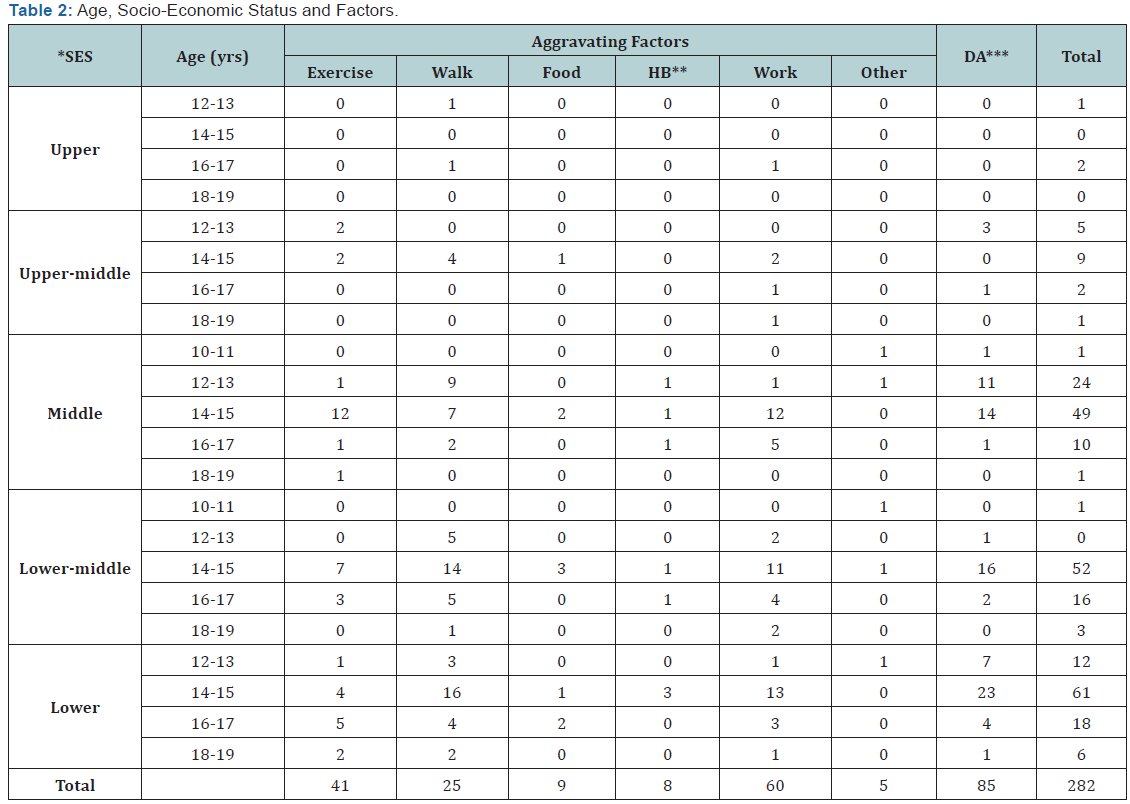
Of 282 school girls interviewed, 197 (69.86%) had dysmenorrhoea. Sixty (30.45%) of those with dysmenorrhea reported that pain got aggravated with everyday work, 19(31.08%) of 61 girls of the upper and middle EC, 18 (30.08%) of 62 of lower EC. Overall 41 (20.81%) of 197 girls reported that they had pain with exercises like skipping, physical training, drills and 25(12.6%) said even with walking (Table 1). Of 118 school girls of 14-15 yrs, 81(68.64%) resorted to rest, 19(16.10%) to hot fomentation and 10(8.4%) to analgesics for pain relief. Of 13 upper-middle EC, 10(76%), 43 of 62(69.35%) of lower EC reported pain relief with rest. Other methods used were lying down prone, yogic exercises, putting asafetida in naval region and drinking milk with turmeric (Table 2).
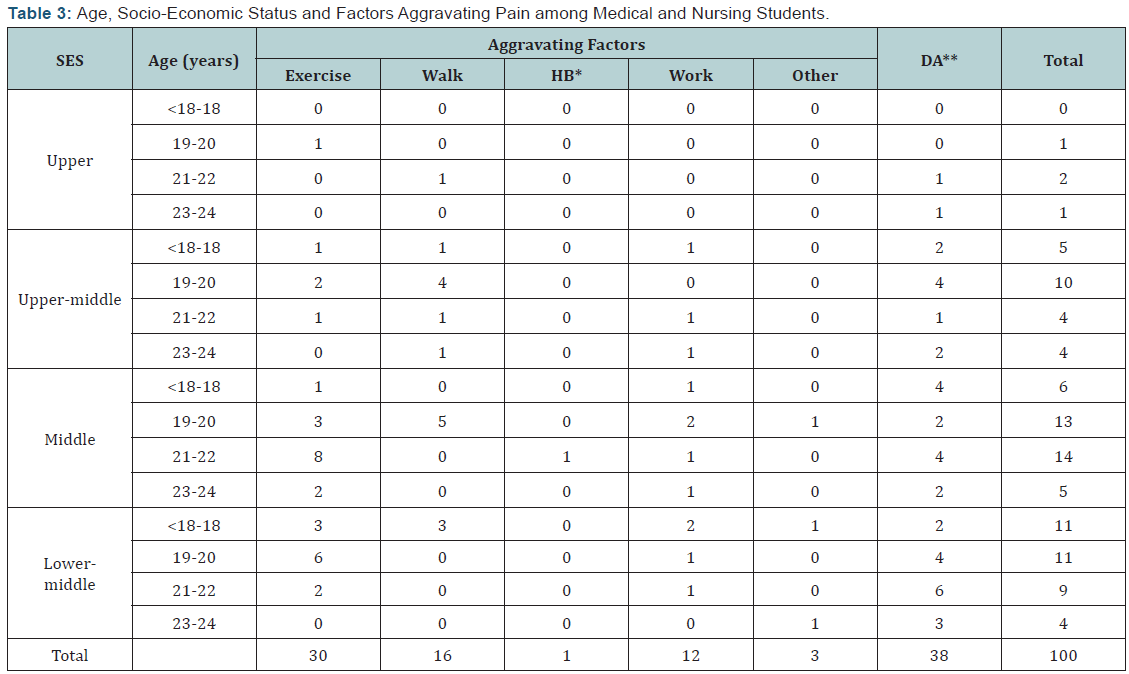
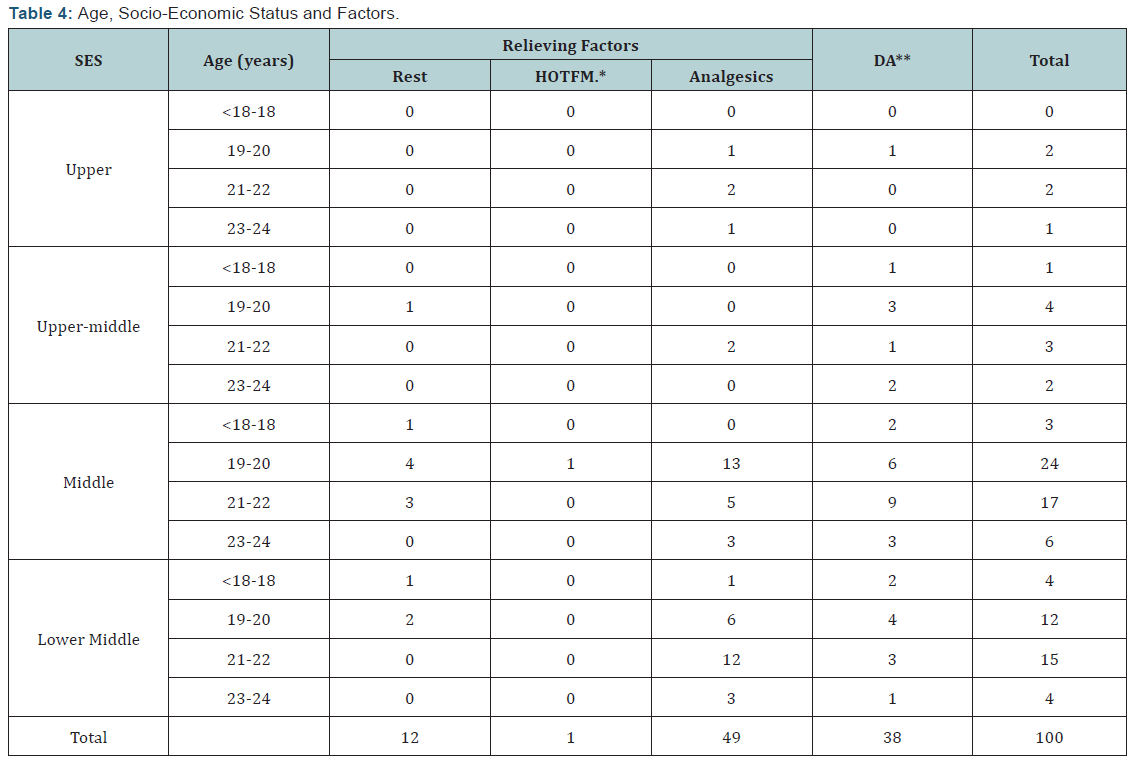
Of 62 medical/nursing students with dysmenorrhea, 30 (48.38%) reported pain aggravated with exercises, like jogging and aerobics which they abandoned during menstruation, 16 (25.80%) reported aggravation of pain even with walking, climbing stairs and 12 (19.35%) with any work. Of 29 medical/ nursing students, of 21-22 yrs age, 16(55.17%) reported pain aggravated with exercise, 5(17%) daily work and 5(17%) while walking. Other factors reported to be aggravating pain were standing for long hours and also lying down in supine position. Twenty six of 21-22 yrs (90%) took analgesics for pain relief. Out of 100 medical/nursing students, 62 had dysmenorrhoea, and 49(79.03%) took analgesics, some in anticipation (Table 3 & 4). Overall most girls said that rest relieved their pain and work, exercise aggravated it. So quite often they missed school and college during menstruation.
There was not much difference in modalities adopted for pain relief in various EC, 76% school girls from upper and uppermiddle EC resorted to rest and 69.35% of lower EC also resorted to rest. Analgesics were used by 8.1% of upper and upper-middle EC and 8.9% lower EC girls. However, lower EC girls resorted more often to kitchen medicine, 8.9% against, 2.7% from upper EC girls (significant difference p<0.05). The type of self medication varied from inserting asafetida in naval region, drinking milk with turmeric, chewing aniseeds, king’s cumin with sugar. More of medical and nursing students resorted to analgesics (79.03%), rest (19.35%).
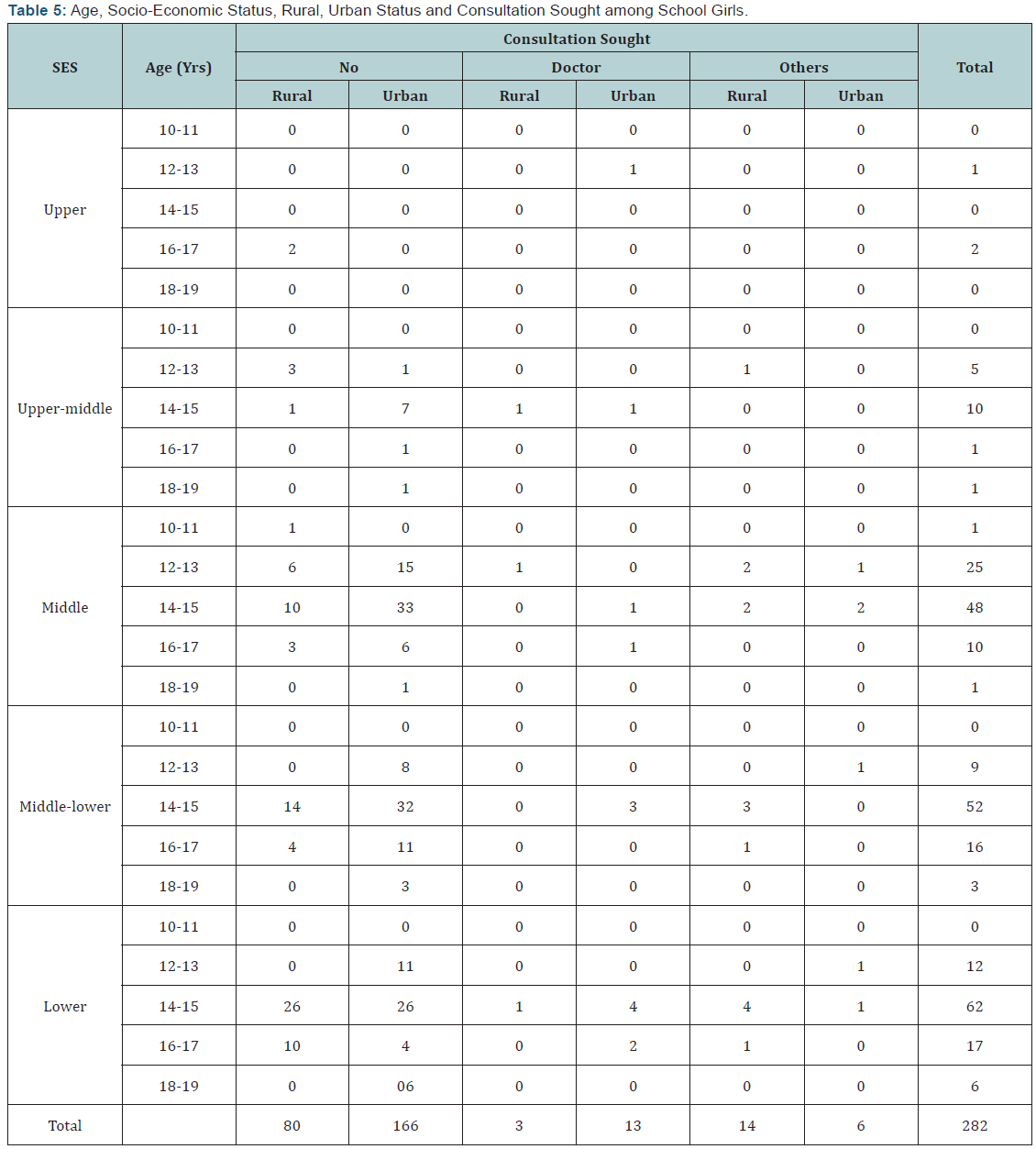
Only 13 (6.59%) of 197 urban school girls and 3(3.19%) of 97 rural school girls had sought help from a doctor, however 14(14.43%) rural and 6(3.2%) urban girls had consulted either nurses or teachers or village health worker, traditional birth attendant and quacks of the village (Table 5).
Of 282 girls, 207 (73%) did not alter their food habits during menstruation from their usual, 168 (81.15%) of them had dysmenorrhoea compared to 29 (38.6% of 75) who changed their diet according to the prevailing customs (p= 0.0001 significant difference). Of these 29 girls who changed diet and still had dysmenorrhoea, 8 used more of vegetables and fruits (believed to decrease pain and blood loss), 10 reported eating more sweets (as it created a sense of well being) and 4 consumed more spicy food (believed to improve their poor appetite during menstruation). Amongst 46 girls who did not have dysmenorrhoea after change of food, 42 (49.41%) used to eat fruits and vegetables during menstruation (believing them to be easier to digest and also prevent pain and excessive blood loss) (Table 6).
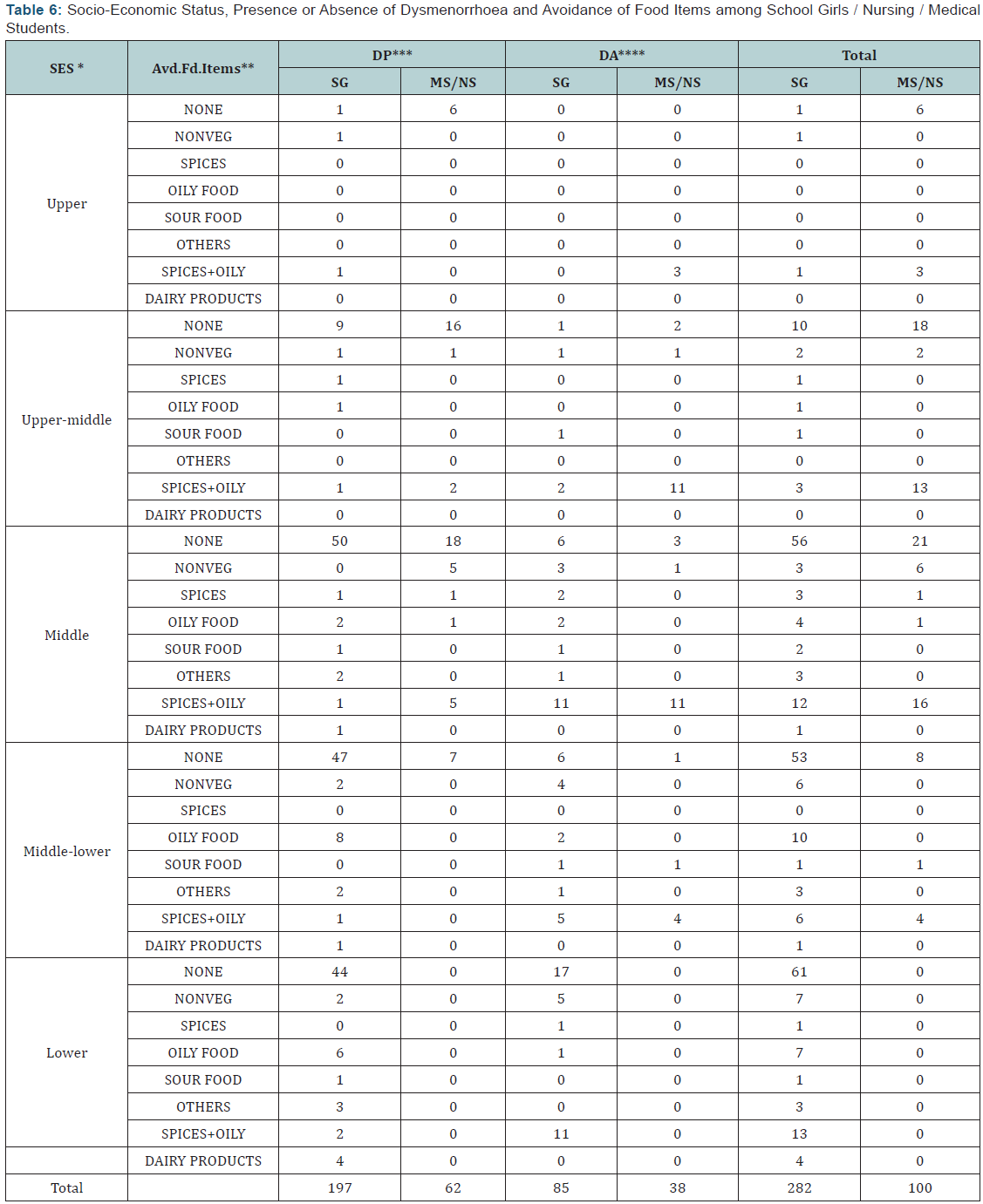
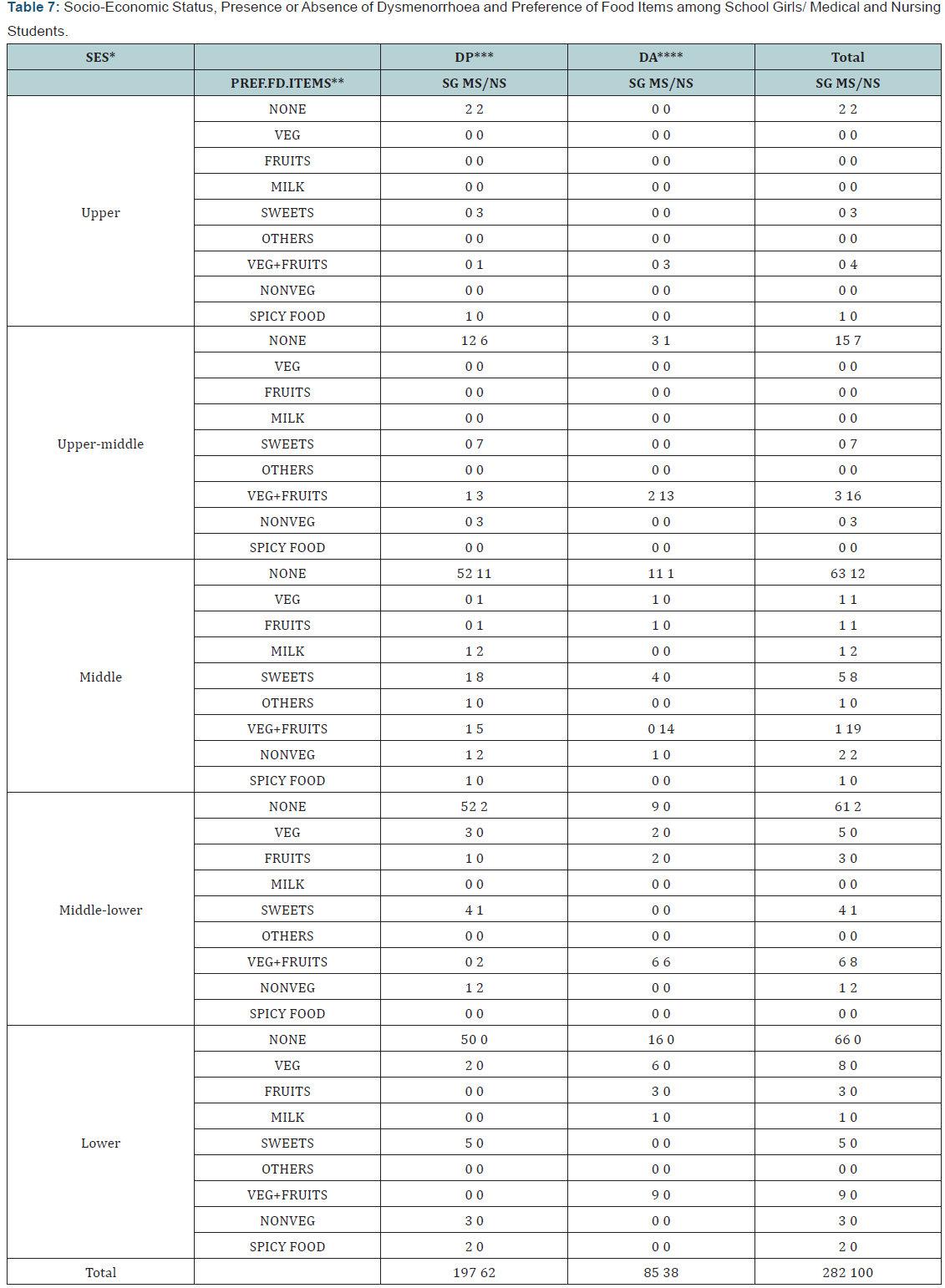
Of 100 medical/nursing students 53 (53%) reported no change of food items, during menstruation, 47(47%) avoided certain food items as per their family culture and customs. Of the 53 girls who had no food change, 47 (89%) had dysmenorrhoea compared to 15 of 47(32%) girls who avoided certain food items during menstruation (p=0.0001 significant difference). Out of these 15 girls, 9(60%) avoided spicy &/or oily food (believed to cause more pain and blood loss), and 6(40%) avoided non vegetarian food (believed to be difficult to digest during menstruation). Of medical /nursing students, 21 (39.62%) out of 53 girls without any food change and 41(87.32%) of 47 who changed during menstruation had dysmenorrhoea. Of the 41 girls who had food change and dysmenorrhoea, 13(31.7%) consumed more of vegetables &/or fruits so that the pain was less and 19 girls reported a craving for sweets including chocolates. Among girls without dysmenorrhoea it was noted that they preferred to consume more of vegetables and fruits during menstruation (believing it protected them from having pain). This alteration of food habit was noted in all the socio-economic strata (Table 7).
Discussion
Primary dysmenorrhea is by far the most common gynaecological problem in menstruating women. It is so common that many women fail to report it in medical interviews, even when their daily activities are restricted. It is usually defined as cramping pain in the lower abdomen occurring at the onset of menstruation in the absence of any identifiable pelvic disease [5].
The pain is difficult to measure partly because it is an individual issue, affected by the mental makeup of the person experiencing pain, and also because it is accompanied by other unpleasant symptoms and many other visible/invisible issues.
In the present study attempts were made to assess the dietary influences by asking the girls which food items they preferred to eat or avoided during menstruation. Seventy three percent school girls reported no alteration/preference of food items from their routine and 27% reported change in food pattern. Among medical/nursing students, 53% reported no change of food habits during menstruation and 47% avoided certain types of food. Dysmenorrhoea was in 89% girls who showed no change in food habits as against 31.9% among those who made dietary changes. Sixty percent of girls with dysmenorrhoea had avoided spicy &/ or oily food and 40% avoided non vegetarian food, 90.6% of girls who did not have dysmenorrhoea had avoided oily &/or spicy food, believing it protected them from pain. Barnard et al. [6] also reported that a low fat vegetarian diet was associated with increased serum sex binding globulin concentration and reduction in dysmenorrhoea duration and intensity. In the present study 27% of school girls who had dysmenorrhoea had no food change and 49.41% of school girls who did not have dysmenorrhoea had changed food items with more vegetables and fruits, believed to decrease blood loss and pain. Likewise Balbi et al. [7] reported that in Naples, girls between 14 to 21 years consumed more of fish and fruits to have protection from dysmenorrhoea.
Years back Klein et al. [8] had reported that only 14.5% of adolescents with dysmenorrhea sought help from a physician for their problem and 30% of parents were not even aware of their daughters dysmenorrhoea and Andersch [9] reported 22% consulted a doctor for their dysmenorrhoea. Not much has changed in decades . Many girls accept dysmenorrhoea as a normal part of their growing up, may be inhibited by social constraints, shyness, in coming forward with their problem or maybe they are told by mother, sisters to bear the pain as “normal”.
Sadiq et al. [10] reported that 38% of girls neither make change in quality nor quantity of food during menstruation, while 21% of them consume more fruits & vegetables as they believe that such food will replenish the lost blood during menstrual flow and 12% of the girls reported hot drinks helpful in alleviating pain during menstrual cycle and 3% reported that sour & spicy food should be avoided during menstruation because they believed that such food will disturb or stop the menstrual flow. Such beliefs were also reported from Singur, West Bengal in which 50% of the 160 adolescent girls who did not consume sour food during menstruation [11], Nair et al. [12] reported that 56% of girls did not consume spicy food. In another study from West Bengal more than half girls made restriction of certain types of food during menstruation [13], Of the adolescent girls 84.2% restricted their physical activities during menstruation to alleviate pain, such practice completely lacks the information in that exercise seems to reduce menstrual symptoms, including pain [14], much higher than the study done in West Bengal in which 42.65% of the 160 girls did not play, 33.82% girls did not perform any household work, during menstruation [11]. The study from Delhi percentage approximates the present study (68%), while only 8% of the Brazilian girls restrict their activity [12,15].
In a study done in Tehran with 250 adolescent girls, about 33% avoided any physical activity during menstrual period [16]. Sadiq et al. [10] reported that 22.6% of the girls do not take bath during menstruation. Bharthi et al. [17] found a decrease in sickness absenteeism and pain during the first day of menstruation in girls who sit in hot water tub. Nair et al. [12] reported that 1.6% avoided bathing during menstruation. While for the study done in West Bengal, 85.7% of the girls had daily bath and the rest felt that bathing should be restricted in the first two days of menstruation as bathing increases the menstrual flow [13]. Poureslami et al. [14] reported that 32% of the adolescent girls practiced the personal health behaviour, such as taking bath. Singh [18] reported that 22.4% adolescent girls of Haryana, India, used analgesics. Harlow [15] reported 21% adolescent girls used analgesics. Over 67% of the girls in Tehran reported taking medicine for their menstrual pain without prescription by a doctor [14], in comparison to 10.8% students in urban, Nigeria who sought medical help [19], only 5.3% consulted a doctor in Haryana [18].
Since dietary changes during menstruation were believed to be beneficial in decreasing blood loss and pain, more research is needed in this particular field, which will not only help in prevention, treatment of dysmenorrhoea but can lead to information about other related disorders. There is need to work on reverse pharmacology.
Conclusion
Dysmenorrhoea is very common. Simple measures are taken for prevention, therapy of dysmenorrhea. Since dietary changes during menstruation were reported to be beneficial in decreasing blood loss and pain, more research is needed in this particular field, which will not only help in prevention, treatment of dysmenorrhoea but can lead to information about other related disorders.
References
- Coupey SM, Ahlstrom P (1989) Common menstrual disorders. Pediatric Clinics of North America 36(3): 551-571.
- French L (2005) Dysmenorrhoea. Am Fam Physician 71(2): 285-291.
- Harada T (2013) Dysmenorrhea and Endometriosis in Young Women. Yonago Acta Med 56(4): 81-84.
- Lefebvre G, Viola Antao, Black A, Burnett M, Feldman K (2005) Primary Dysmenorrhea Consensus Guideline, No 169, pp. 1122.
- Lefebvre G, Pinsonneault O, Antao V, Black A, Burnett M, et al. (2005) SOGC Clinical Practice Guideline; Primary Dysmenorrhea Consensus Guideline. No 169.
- Medyhealth Team (2015) 5 Most Common Gynae Problems Every Woman Must Know.
- Barnard ND, Scialli AR, Hurlock D, Bertron P (2000) Diet and Sex‐ Hormone Binding Globulin, Dysmenorrhea, and Premenstrual Symptoms. Obstet Gynecol 95(2): 245-250.
- Balbi C, Musone R, Menditto A, Di Prisco L, Cassese E, et al. (2000) Influence of menstrual factors and dietary habits on menstrual pain in adolescence age. Eur J Obstet Gynecol Reprod Biol 91(2):143-148.
- Klein JR, Litt IF (1981) Epidemiology of adolescent dysmenorrhea. Pediatrics 68(5): 661-664.
- Andersch B, Milsom I (1982) An epidemiological study of young women with dysmenorroea. Am J Obstet Gynecol 144(6): 655-660.
- Sadiq MA, Salih AA (2013) Knowledge and Practice of Adolescent Females about Menstruation in Baghdad. J Gen Pract 2: 138.
- Dasgupta A, Sarkar M (2008) Menstrual Hygiene: How Hygienic is the Adolescent Girl? Indian J Community Med 33(2): 77-80.
- Nair P, Grover VL, Kannan AT (2007) Awareness and practices of menstruation and pubertal changes amongst unmarried female adolescents in a rural area of East Delhi. Indian J Community Med 32(2): 156-157.
- Yasmin S, Manna N, Mallik S, Ahmed A, Paria B (2013) Menstrual hygiene among adolescent school students: An in depth crosssectional study in an urban community of West Bengal, India. IOSR Journal of Dental and Medical Sciences 5(6): 22-26.
- Poureslami M, Osati-Ashtiani F (2002) Assessing Knowledge, Attitudes and Behavior of Adolescent Girls in Suburban Districts of Tehran about Dysmenorrhea and Menstrual Hygiene. Journal of International Women’s Studies 3(2): 51-61.
- Harlow SD, Campbell OM (2000) Menstrual dysfunction: a missed opportunity for improving reproductive health in developing countries. Reprod Health Matters 8(15): 142-147.
- Smith RP, Kaunitz AM (2013) Patient information: Painful menstrual periods (dysmenorrhea) (Beyond the Basics) Up To Date.
- Bharthi HP, Murthy SN, Babina N, Kadam A, Raghavendra M (2012) Management of pelvic pain in primary dysmenorrhea using a hot hipbath: a pilot study. Altern Ther Health Med 18(1): 24-25.
- Singh MM, Devi R, Gupta SS (1999) Awareness and health seeking behaviour of rural adolescent school girls on menstrual and reproductive health problems. Indian J Med Sci 53(10): 439-443.
- Esimai O, Esan GO (2010) Awareness of menstrual abnormality amongst college students in urban area of ile-ife, osun state, Nigeria. Indian J Community Med 35(1): 63-66.







